Abstract
Objective
Accurate calculation of set-up margin is a prerequisite to arrive at the most optimal clinical to planning target volume margin. The aim of this study was to evaluate the compatibility of different on-board and in-room stereoscopic imaging modalities by calculating the set-up margins (SM) in stereotactic body radiotherapy technique accounting and unaccounting for rotational positional errors (PE). Further, we calculated separate SMs one based on residual positional errors and another based on residual + intrafraction positional errors from the imaging data obtained in a dual imaging environment.
Materials and methods
A total of 22 lung cancer patients were included in this study. For primary image guidance, four-dimensional cone beam computed tomography (4-D CBCT) was used and stereoscopic ExacTrac was used as the auxiliary imaging. Following table position correction (TPC) based on the initial 4-D CBCT, another 4-D CBCT (post-TPC) and a pair of stereoscopic ExacTrac images were obtained. Further, during the treatment delivery, a series of ExacTrac images were acquired to identify the intrafraction PE. If a, b and c were the observed translational shifts in lateral (x-axis), longitudinal (y-axis) and vertical direction (z-axis) and α, β and γ were the rotational shifts in radians about the same axes, respectively, then the resultant translational vectors (A, B and C) were calculated on the basis of translational and rotational values. Set-up margins were calculated using residual errors post-TPC only and also using intrafraction positional errors in addition to the residual errors.
Results
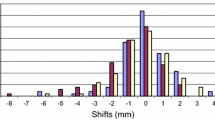
Residual and residual + intrafraction SM were calculated from a dataset of 82 CBCTs and 189 ExacTrac imaging sessions. CBCT-based mean ± SD shifts in translational and rotational directions were 0.3 ± 1.8 mm, 0.1 ± 1.8 mm, − 0.4 ± 1.6 mm, 0.1 ± 0.4°, 0.0 ± 1.0° and 0.3 ± 0.7°, respectively, and for ExacTrac − 0.1 ± 1.8 mm, 0.2 ± 2.4 mm, − 0.6 ± 1.8 mm, 0.1 ± 1.2°, − 0.2 ± 1.3° and − 0.1 ± 0.6°, respectively. Residual SM without considering the rotational correction in x, y and z directions were 5.0 mm, 4.5 mm and 4.4 mm; rotation-corrected SM were 4.4 mm, 4.0 mm and 5.5 mm, respectively. Residual plus intrafraction SM were 5.5 mm, 6.6 mm and 6.2 mm without considering the rotational corrections, whereas they were 5.0 mm, 6.3 mm and 6.2 mm with rotational errors accounted for.
Conclusion
Accurate calculation of set-up margin is required to find the clinical to planning target volume margin. Primary and auxiliary imaging margins fall in the range of 4.0 to 5.5 mm and 5.0 to 7.0 mm, respectively, indicating a higher SM for X-ray-based planar imaging techniques over three-dimensional cone beam images. This study established the degree of mutual compatibility between two different kinds of widely used set-up imaging modalities, on-board CBCT and in-room stereoscopic imaging ExacTrac. It also describes the technique to calculate the residual and residual plus intrafraction SM and its variation in a dual imaging environment accounting for rotational PE in stereotactic body radiotherapy of lung.




Similar content being viewed by others
References
Timmerman R, Paulus R, Galvin J et al (2010) Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA 303:1070–1076
Fakiris AJ, McGarry RC, Yiannoutsos CT et al (2009) Stereotactic body radiation therapy for early-stage non-small-cell lung carcinoma: four year results of a prospective phase II study. Int J Radiat Oncol Biol Phys 75:677–682
Baumann P, Nyman J, Hoyer M et al (2009) Outcome in a prospective phase II trial of medically inoperable stage I non-small-cell lung cancer patients treated with stereotactic body radiotherapy. J Clin Oncol 27:3290–3296
McGrath SD, Matuszak MM, Yan D et al (2009) Volumetric modulated arc therapy for delivery of hypofractionated stereotactic lung radiotherapy: a dosimetric and treatment efficiency analysis. Radiother Oncol 90:422–423
Holt A, van Vliet-Vroegindeweij C, Man A et al (2011) Volumetric-modulated arc therapy for stereotactic body radiotherapy of lung tumors: a comparison with intensity-modulated radiotherapy techniques. Int J Radiat Oncol Biol Phys 81:1560–1567
Paul S, Sarkar B, Ganesh T, Munshi A, Kumar R, Mohanti BK (2014) EP-1641: PTV margin calculation and time dependency monitoring of intrafraction isocenter movement in lung SBRT by ExacTrac. Radiother Oncol 1(111):S221
van Herk M, Bruce A, Kroes AG, Shouman T, Touw A, Lebesque JV (1995) Quantification of organ motion during conformal radiotherapy of the prostate by three dimensional image registration. Int J Radiat Oncol Biol Phys 33(5):1311–1320
van Herk M (2004) Errors and margins in radiation oncology. Semin Radiat Oncol 14:52–64
Higgins J, Bezjak A, Hope A, Panzarella T, Li W, Cho JB, Craig T, Brade A, Sun A, Bissonnette JP (2011) Effect of image-guidance frequency on geometric accuracy and SMin radiotherapy for locally advanced lung cancer. Int J Radiat Oncol Biol Phys 80(5):1330–1337
Fuss M, Salter BJ, Rassiah P, Cheek D, Cavanaugh SX, Herman TS (2004) Repositioning accuracy of a commercially available double-vacuum whole body immobilization system for stereotactic body radiation therapy. Technol Cancer Res Treat 3:59–67
Guckenberger M, Meyer J, Vordermark D, Baier K, Wilbert J, Flentje M (2006) Magnitude and clinical relevance of translational and rotational patient set-up errors: a cone-beam CT study. Int J Radiat Oncol Biol Phys 65(3):934–942
Guckenberger M, Meyer J, Wilbert J, Baier K, Sauer O, Flentje M (2007) Precision of image-guided radiotherapy (IGRT) in six degrees of freedom and limitations in clinical practice. Strahlenther Onkol 183(6):307–313
Suzuki O, Nishiyama K, Ueda Y, Miyazaki M, Tsujii K (2012) Influence of rotational set-up error on tumor shift in bony anatomy matching measured with pulmonary point registration in stereotactic body radiotherapy for early lung cancer. Jpn J Clin Oncol 42(12):1181–1186
Josipovic M, Persson GF, Logadottir A, Smulders B, Westmann G, Bangsgaard JP (2012) Translational and rotational intra- and inter-fractional errors in patient and target position during a short course of frameless stereotactic body radiotherapy. Acta Oncol 51(5):610–617
Fatunase T, Wang Z, Yoo S, Hubbs JL, Prosnitz RG, Yin FF, Marks LB (2008) Assessment of the residual error in soft tissue set-up in patients undergoing partial breast irradiation: results of a prospective study using cone-beam computed tomography. Int J Radiat Oncol Biol Phys 70(4):1025–1034
Sarkar B, Roy J, Manikandan A (2015) In Regard to Onimaruet al. Int J Radiat Oncol Biol Phys 93(5):1166
Sarkar B, Ray J, Ganesh T, Manikandan A, Munshi A, Rathinamuthu S, Kaur H, Anbazhagan S, Giri UK, Roy S, Jassal K (2018) Methodology to reduce 6D patient positional shifts into a 3D linear shift and its verification in frameless stereotactic radiotherapy. Phys Med Biol 63(7):075004
Sarkar B, Munshi A, Ganesh T, Manikandan A, Krishnankutty S, Chitral L, Pradhan A, Kalyan MB (2019) Rotational positional error corrected intrafraction set-up margins in stereotactic radiotherapy: a spatial assessment for coplanar and noncoplanar geometry. Med Phys 5:196
Ganesh T, Paul S, Munshi A, Sarkar B, Krishnankutty S, Sathya J, George S, Jassal K, Roy S, Mohanti B (2014) SU-E-J-39: comparison of PTV margins determined by in-room stereoscopic image guidance and by on-board cone beam computed tomography technique for brain radiotherapy patients. Med Phys 41(6):163
Sarkar B, Ganesh T, Manikandan A, Krishnankutty S, Chitral L, Munshi A, Mohanti BK (2019) Rotation corrected set-up margin calculation for stereotactic body radiation therapy in dual imaging environment. Med Phys 46(6):E307–E307
Garibaldi C, Piperno G, Ferrari A, Surgo A, Muto M, Ronchi S, Bazani A, Pansini F, Cremonesi M, Jereczek-Fossa BA, Orecchia R (2016) Translational and rotational localization errors in cone-beam CT based image-guided lung stereotactic radiotherapy. Physica Med 32(7):859–865
Lee J, Kim JI, Ye SJ, Kim HJ, Carlson J, Park JM (2015) Dosimetric effects of roll rotational set-up errors on lung stereotactic ablative radiotherapy using volumetric modulated arc therapy. Br J Radiol 88(1055):20140862
Yeung AR, Li JG, Shi W, Newlin HE, Chvetsov A, Liu C, Palta JR, Olivier K (2009) Tumor localization using cone-beam CT reduces SMin conventionally fractionated radiotherapy for lung tumors. Int J Radiat Oncol Biol Phys 74(4):1100–1107
Fu W, Yang Y, Li X, Heron DE, Huq MS, Yue NJ (2006) Dosimetric effects of patient rotational set-up errors on prostate IMRT treatments. Phys Med Biol 51(20):5321
Wang H, Shiu A, Wang C, O’Daniel J, Mahajan A, Woo S, Liengsawangwong P, Mohan R, Chang EL (2008) Dosimetric effect of translational and rotational errors for patients undergoing image-guided stereotactic body radiotherapy for spinal metastases. Int J Radiat Oncol Biol Phys 71(4):1261–1271
Li W, Purdie TG, Taremi M, Fung S, Brade A, Cho BJ, Hope A, Sun A, Jaffray DA, Bezjak A, Bissonnette JP (2011) Effect of immobilization and performance status on intrafraction motion for stereotactic lung radiotherapy: analysis of 133 patients. Int J Radiat Oncol Biol Phys 81(5):1568–1575
Nakamura M, Takamiya M, Akimoto M, Ueki N, Yamada M, Tanabe H, Mukumoto N, Yokota K, Matsuo Y, Mizowaki T, Kokubo M (2015) Target localization errors from fiducial markers implanted around a lung tumor for dynamic tumor tracking. Physica Med 31(8):934–941
Li JS, Jin L, Pollack A, Horwitz EM, Buyyounouski MK, Price RA Jr, Ma CM (2009) Gains from real-time tracking of prostate motion during external beam radiation therapy. Int J Radiat Oncol Biol Phys 75(5):1613–1620
Tehrani JN, O’Brien T, R, Poulsen PR, Keall P, (2013) Real-time estimation of prostate tumor rotation and translation with a kV imaging system based on an iterative closest point algorithm. Phys Med Biol 58(23):8517
Huang CY, Tehrani JN, Ng JA, Booth J, Keall P (2015) Six degrees-of-freedom prostate and lung tumor motion measurements using kilovoltage intrafraction monitoring. Int J Radiat Oncol Biol Phys 91(2):368–375
Yang Y, Catalano S, Kelsey CR, Yoo DS, Yin FF, Cai J (2014) Dosimetric effects of rotational offsets in stereotactic body radiation therapy (SBRT) for lung cancer. Med Dosim 39(1):117–121
Stieb S, Malla M, Graydon S, Riesterer O, Klöck S, Studer G, Tanadini-Lang S (2018) Dosimetric influence of pitch in patient positioning for radiotherapy of long treatment volumes; the usefulness of six degree of freedom couch. Br J Radiol 91:20170704
Giri U, Ganesh T, Saini V, Munshi A, Sarkar B, Mohanti B (2016) SU-F-J-47: inherent uncertainty in the positional shifts determined by a volumetric cone beam imaging system. Med Phys 43(6):3416
Jassal K, Munshi A, Sarkar B, Paul S, Sharma A, Mohanti BK, Ganesh T, Chougule A, Sachdev K (2014) Validation of an integrated patient positioning system: Exactrac and iViewGT on synergy platform. Int J Cancer Therapy Oncol 2(2):5433
Sarkar B, Munshi A, Krishnankutty S, Ganesh T, Kalyan MB (2017) Positional errors in linear accelerator based frameless cranial stereotaxy: a note of caution. J BU ON Off J Balkan Union Oncol 22(6):1606
Acknowledgement
The authors sincerely acknowledge Mr. Sanjib Chanda for his help in figure preparation.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have declare that they have no conflict of interest.
Human and animals rights
None.
Informed consent
Applicable-Obtained
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Theory of rotational error correction for inertial frame of references
Appendix: Theory of rotational error correction for inertial frame of references
We begin with explaining the theory of rotational correction in inertial frame of reference, considering two different scenarios. First, the origin of the coordinate system or origin (isocentre) is off from the tumour centre; in the second scenario, isocentre is at the tumour centre. Figure
5A graphically explains the situation when tumour centre is away from the centre of the coordinate system (origin) or isocentre. In the left panel, in the solid coordinate system the solid arrow crosses the solid star in certain angle. A certain amount of rotational error, analogous to the patient positional set-up error, was introduced to the solid star and identified as dotted. As shown in the left panel of Appendix Figure 5, it is not possible to find the same angle between dotted arrow–star to that of solid arrow–star only by a rotation. In such situation, a linear coordinate transformation or Galilean transformation is required to obtain a new origin and further apply the rotational correction. Right panel of Figure 5A shows that it is possible to find the appropriate dotted arrow–star puncture angle to that of the solid arrow–star before the introduction of rotational error.
In the second scenario as shown in Fig. 5b, isocentre is at the tumour centre offers a much more simpler geometrical condition. No linear coordinate transformation is required to obtain the desired angle. The solid star can be punctured by the solid arrow in the same angle as that of dotted star–arrow combination only by a rotation of the coordinate system (Fig. 6).
Scenario I: When tumour centre away from isocentre.
Rights and permissions
About this article
Cite this article
Sarkar, B., Ganesh, T., Munshi, A. et al. Rotational positional error-corrected linear set-up margin calculation technique for lung stereotactic body radiotherapy in a dual imaging environment of 4-D cone beam CT and ExacTrac stereoscopic imaging. Radiol med 126, 979–988 (2021). https://doi.org/10.1007/s11547-021-01355-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-021-01355-7