Abstract
Background and purpose
COVID-19 constitutes a worldwide threat, prompting Italian Government to implement specific measures on March 8, 2020, to protect patients and health workers from disease transmission. The impact of preventive measures on daily activity of a radiotherapy facility may hamper the ability to fulfill normal workload burden. Thus, we assessed the number of delivered treatments in a specific observation period after the adoption of preventive measures (since March 11 to April 24, 2020) and compared it with the corresponding period of the year 2019.
Materials and methods
Overall number of delivered fractions was related to actual time of platform daily activity and reported as a ratio between number of delivered fractions and activity hours (Fr/Hrs). Fr/Hrs were calculated and compared for two different periods of time, March 11–April 24, 2019 (Fr/Hrs1), and March 11–April 24, 2020 (Fr/Hrs2).
Results
Fr/Hrs1 and Fr/Hrs2 were 2.66 and 2.54 for year 2019 and 2020, respectively, for a Fr/Hrsratio of 1.07 (95% CI 1.03–1.12, p = 0.0005). Fr/Hrs1 was significantly higher than Fr/Hrs2 for SliR and PreciseR, with Fr/Hrsratio of 1.92 (95% CI 1.66–2.23, p < 0.0001) and 1.11 (95% CI 1.03–1.2, p = 0.003), respectively. No significant difference was reported for SynergyR and CyberknifeR with Fr/Hrsratio of 0.99 (95% CI 0.91–1.08, p = 0.8) and 0.9 (95% CI 0.77–1.06, p = 0.2), respectively. Fr/Hrs1 was significantly lower than Fr/Hrs2 for TomotherapyR, with Fr/Hrsratio of 0.88 (95% CI 0.8–0.96, p = 0.007).
Conclusion
Preventive measures did not influence workload burden performed. Automation in treatment delivery seems to compensate effectively for health workers number reduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and purpose
Coronavirus (COVID-19) disease currently constitutes a worldwide threat [1], and pandemic status was declared by World Health Organization on March 11, 2020. Europe faced this issue after the China outbreak, and Italy was one of the most affected countries [2, 3]. Early experiences of emergency management within the framework of a public National healthcare system have already been published [4, 5], but the risk of a widespread propagation of COVID-19 between patients referring to hospitals prompted the Italian Government to implement specific preventive measures on March 8, 2020 [6]. Main actions consisted in temperature check and hand disinfection at departments entrance, use of personal protective equipment (PPE) for all health workers and patients, limitation of caregivers access into hospital and healthcare personnel shortage. Specifically, technical staff (Medical Physics, Radiology Technician, MD) was divided into different working groups to prevent the spread of disease between healthcare personnel reducing inter-operator contacts. Moreover, waiting room for patients was reorganized to reduce and space the seats, limiting the access to patients waiting for their treatment. These measures are particularly important for oncological care, considering that cancer patients are a fragile population, due to the synergistic immunodepressive effects of disease and antineoplastic treatments, with higher risk of COVID-19 and poorer prognosis in this setting [7, 8]. Reduction of population density in the clinical environment (e.g., lower number of health workers and caregivers together) is of utmost importance. However, the impact of preventive measures on daily activity of a radiotherapy facility is a potential issue, hampering the ability to fulfill normal workload burden. This is critical especially considering that oncological treatments (e.g., definitive, adjuvant or palliative radiotherapy) are often non-deferrable. Indeed, the reduction of elective services remains still challenging due to the heterogeneity of cancer treatments [9]. The reduction in terms of output is unacceptable to avoid impact on waiting list of a radiotherapy facility. One of the most intuitive output measures in this context is amount of daily delivered treatments. For this reason, we assessed the number of delivered treatments in a specific observation period after the adoption of preventive measures (since March 11 to April 24, 2020) and compared it with the corresponding period of the year 2019, aiming to assess the impact of COVID-19 prevention on daily routine of our department.
Materials and methods
Data about delivered treatments and daily time of scheduled activity of all linear accelerators available in Careggi Hospital Radiotherapy Department (Florence, Italy) were collected and reported. Overall equipment consisted in 3 linear accelerators (LINACS): SliR, PreciseR, SynergyR (Elekta, Stockholm, Sweden), one TomotherapyR and one Cyberknife systemR (Accuray, Sunnyvale, California). Data about SliR, PreciseR, SynergyR and TomotherapyR were downloaded from MosaiqR patients and treatment data management system (Elekta, Stockholm, Sweden). Workload for CyberknifeR system was manually registered from daily schedule. Differences in terms of percentages of treatment fractions delivered on the same platform in the two different periods were tested by comparison of proportions. Overall number of delivered fractions was related to actual time of platform daily activity and reported as a ratio between number of delivered fractions and activity hours (Fr/Hrs). All planned interventions for equipment maintenance and quality assessment occurred in the period analyzed were deducted from overall platform activity time. Fr/Hrs were calculated for two different periods of time, March 11–April 24, 2019 (Fr/Hrs1), and March 11–April 24, 2020 (Fr/Hrs2). Preventive measures for COVID-19 pandemic were adopted on March 8, 2020. Fr/Hrs1 and Fr/Hrs2 were compared through test based method, and their ratio (Fr/Hrsratio) was calculated by Exact Poisson Method. Briefly, a Fr/Hrsratio > 1 suggested that higher number of fractions for hour of activity were delivered on the same platform in 2019 if compared to 2020. All statistical analyses were performed through MedCalc Statistical Software version 18.9.1 (MedCalc Software bv, Ostend, Belgium).
Results
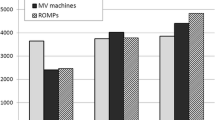
Overall, 4267 and 4031 treatment fractions were delivered in a total activity time of 1600 and 1584 h in 2019 and 2020, respectively. Workload burden for each single platform was compared between the two different periods: 12.8 vs 7%, 34.4 vs 33%, 25.6 vs 28%, 8.2 vs 7% and 19 vs 25% of overall amount of treatment fractions were delivered on SliR, PreciseR, SynergyR, CyberknifeR and TomotherapyR in 2019 vs 2020, respectively. Differences were statistically significant for SliR, SynergyR, CyberknifeR and TomotherapyR, with variations between 2019 and 2020 of − 5.8 (95% CI 4.5;7%, p < 0.0001), + 2.4 (95%CI 0.49;4.3, p = 0.01), − 1.2 (95%CI 0.05;2.34, p = 0.03) and + 6% (95%CI 4.2;7.8, p < 0.0001), respectively. Conversely, no significant difference was detected for PreciseR, with − 1.4% (95%CI -0.64;3.4, p = 0.17). Fr/Hrs1 and Fr/Hrs2 were 2.66 and 2.54 for year 2019 and 2020, respectively, for a Fr/Hrsratio of 1.07 (95% CI 1.03–1.12, p = 0.0005). In particular Fr/Hrs1 and Fr/Hrs2 were 2.8 vs 1.4, 3.73 vs 3.34, 2.78 vs 2.8, 1.44 vs 1.59 and 2.14 vs 2.44 on SliR, PreciseR, SynergyR, CyberknifeR and TomotherapyR, respectively. Fr/Hrs1 was significantly higher than Fr/Hrs2 for SliR and PreciseR, with Fr/Hrsratio of 1.92 (95% CI 1.66–2.23, p < 0.0001) and 1.11 (95% CI 1.03–1.2, p = 0.003), respectively. No significant difference was reported for SynergyR and CyberknifeR with Fr/Hrsratio of 0.99 (95% CI 0.91–1.08, p = 0.8) and 0.9 (95% CI 0.77–1.06, p = 0.2), respectively. Conversely, Fr/Hrs1 was significantly lower than Fr/Hrs2 for TomotherapyR, with Fr/Hrsratio of 0.88 (95% CI 0.8–0.96, p = 0.007). Sensitivity analyses were conducted also grouping all platforms equipped only with manual setup corrections (SliR and PreciseR), and all platforms were automated setup corrections and/or tumor tracking is available (SynergyR, CyberknifeR and TomotherapyR).
Overall, significant difference between 2019 and 2020 was detected for SliR and PreciseR, with a 6.4% decrease in terms of delivered treatment fractions (95%CI − 8.6; − 4.33, p < 0.0001), as well as for SynergyR, CyberknifeR and TomotherapyR, showing a 6.5% increase (95%CI 4.5; 8.6, p < 0.0001). Moreover, results showed that Fr/Hrs1 was significantly higher than Fr/Hrs2 for the first group, with a Fr/Hrsratio of 1.26 (95% CI 1.18–1.34, p < 0.0001). Conversely Fr/Hrs1 was significantly lower than Fr/Hrs2 for the second group, with a Fr/Hrsratio of 0.91 (95% CI 0.86–0.96, p = 0.002). Main results are summarized in Table 1 and Fig. 1.
Discussion
Overall, results seem to suggest a significant change in terms of platform commitment between comparable time periods of years 2019 and 2020. Indeed, significant reduction in terms of treatment fractions delivered with SliR and CyberknifeR was detected during COVID-19 pandemic, while other platforms (SynergyR and TomotherapyR) registered significant increase in their activity during this period. In our opinion, trend to deliver hypofractionated treatment schedule during the pandemic may have influenced these data. Indeed, palliative treatment schedules consisting in 30 Gy in 10 fractions, usually delivered with a direct posterior field technique through SliR platform, may have been discouraged in favor of equieffective schedules consisting in 25 Gy in 5 fractions delivered by volumetric modulated arc therapy through SynergyR platform. Thus, a significant amount of treatment fractions may have been shifted from SliR to SynergyR for this reason. CyberknifeR platform use has been probably affected by the need to avoid any additional procedure (e.g., fiducials placement for tracking purposes) during the pandemic, if compared to year 2019.
Of course, simultaneous integrated boost (SIB) techniques have been encouraged in 2020, aiming to reduce overall treatment duration, contributing to the increase in TomotherapyR platform use. Impact of hypofractionated schedules and SIB techniques has been important specially to reduce number of treatment fractions for prostate cancer (both in definitive and postoperative setting) and breast cancer (specially in postoperative setting). Data from the present analysis show a significant difference in terms of number of delivered fractions per hour of platform activity, with a 7% decrease during the COVID-19 pandemic if compared to the homologous time period of 2019. This may be related to the lower number of healthcare professionals working at the same time on the different platforms, to the variation in the logistics of facility, to the increased time needed to care for the single patient due to the precautions requested (e.g., PPE dressing and check before and during clinical activity) or to the overall deceleration of tasks due to multiple checks established. However, the overall impact of COVID-19 diffusion preventive measures on the daily workload burden performed was, in the end, sustainable, considering that only 1 treatment fraction was lost for each 14 delivered.
During the first days of the outbreak, many radiotherapy facilities in Italy were forced to significantly reduce their clinical activity [10], and currently it is not known whether special measures undertaken for COVID-19 outbreak will be maintained also after number of cases decrease in our country [6]. However, these data are encouraging, underlining that present organization could be sustained for a radiotherapy department also in the next future, providing the correct social distancing between healthcare workers and patients while keeping a low impact on treatment delay of undeferrable oncological cares. Indeed, experiences in different fields show that patients requiring high-priority interventions may pose challenges in allocation of resources in the current COVID-19 pandemic [11] and that responses to the COVID-19 outbreak have to be carefully optimized [12]. However, impact of preventive measures on workload burden performed and waiting list represent an important issue for cancer management, considering that careful balance should be performed between the oncological risk of delayed cancer intervention versus the risks of COVID-19 to the patient, treating healthcare professionals and the healthcare system [13]. Indeed, the risk of postponing scheduled procedures, focusing only on COVID-19 situation (the so-called distraction effect) may have negative health and social costs [14]. Conversely, this influence could be considered negligible for our department, a complex institution routinely managing both palliative and curative radiotherapy, systemic treatments (chemo- and immunotherapies) and radiometabolites administration. This is a representative scenario of integration between complete oncological care and preventive measures during the COVID-19 pandemic. Moreover, preventive measures seem to have limited impact on satisfaction of patients treated in our department. Indeed, two validated questionnaires (EORTC QLQ-C30, FACIT-TS-G version 1) and 14 specific questions evaluating perception of COVID-19 measures were administered to patients during pandemic period. Results suggest high level of cancer outpatient satisfaction [15] underlining that both clinical activity and patient perception are unchanged despite the current situation. Interestingly, all platforms equipped with systems allowing to correct the setup without accessing to the bunker were not influenced by the actual measures. Probably, the workflow in these cases is not affected because of the lower direct contact of healthcare workers with the patient and the higher automation of treatment delivery. This aspect deserves further consideration, highlighting that referral to centers with the availability of modern radiotherapy platform may help to reduce unnecessary health workers density during clinical activity. Of note, no COVID-19-infected patients were treated in our institution during the outbreak, and workload burden would have probably been negatively influenced in that eventuality. Of course, referral to validated common recommendations will further improve clinical routine and help to reduce unnecessary workload burden. National guidelines as well as practical recommendations regarding radiotherapy during COVID-19 outbreak have been published [16,17,18,19]. These data will be interesting especially in the next future, when national healthcare institutions will have to decide whether preventive measures should be discontinued or maintained. Indeed, this setting will require careful evaluation of the balance between the impact of these measures on cancer clinical care and the need to avoid the risk of new infective outbreaks.
Conclusion
Covid-19 pandemic significantly influenced platforms commitment during year 2020 in our institution. Despite a significant difference in terms of number of fractions delivered per hour of activity, current preventive measures did not influence workload burden performed in our department. Furthermore, automation in treatment delivery seems to compensate effectively for health workers number reduction. These arguments suggest that measures undertaken during COVID-19 outbreak may be sustainable, if needed, without impact on undeferrable oncological care.
References
Ippolito G, Hui DS, Ntoumi F, Maeurer M, Zumla A (2020) Toning down the 2019-nCoV media hype-and restoring hope. Lancet Respirat Med 8(3):230–231. https://doi.org/10.1016/S2213-2600(20)30070-9
Rosenbaum L (2020) Facing Covid-19 in Italy–Ethics, Logistics, and therapeutics on the epidemic’s front line. New England J Med 382(20):1873–1875. https://doi.org/10.1056/NEJMp2005492
Onder G, Rezza G, Brusaferro S (2020) Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323(18):1775–1776. https://doi.org/10.1001/jama.2020.4683
Grasselli G, Pesenti A, Cecconi M (2020) Critical care utilization for the COVID-19 outbreak in lombardy, Italy: early experience and forecast during an emergency response. JAMA 323(16):1545–1546. https://doi.org/10.1001/jama.2020.4031
Spina S, Marrazzo F, Migliari M, Stucchi R, Sforza A, Fumagalli R (2020) The response of Milan’s Emergency Medical System to the COVID-19 outbreak in Italy. Lancet (London, England) 395(10227):e49–e50. https://doi.org/10.1016/S0140-6736(20)30493-1
Remuzzi A, Remuzzi G (2020) COVID-19 and Italy: what next? Lancet (London, England) 395(10231):1225–1228. https://doi.org/10.1016/S0140-6736(20)30627-9
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J (2020) Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 21(3):335–337. https://doi.org/10.1016/S1470-2045(20)30096-6
Xia Y, Jin R, Zhao J, Li W, Shen H (2020) Risk of COVID-19 for patients with cancer. Lancet Oncol 21(4):e180. https://doi.org/10.1016/S1470-2045(20)30150-9
Simcock R, Thomas TV, Estes C, Filippi AR, Katz MA, Pereira IJ, Saeed H (2020) COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Translat Radiat Oncol 22:55–68. https://doi.org/10.1016/j.ctro.2020.03.009
Jereczek-Fossa BA, Palazzi MF, Soatti CP, Cazzaniga LF, Ivaldi GB, Pepa M, Amadori M, Antognoni P, Arcangeli S, Buffoli A, Beltramo G, Berlinghieri S, Bignardi M, Bracelli S, Bruschieri L, Castiglioni S, Catalano G, Di Muzio N, Fallai C, Fariselli L, Filippi AR, Gramaglia A, Italia C, Lombardi F, Magrini SM, Nava S, Orlandi E, Pasinetti N, Sbicego EL, Scandolaro L, Scorsetti M, Stiglich F, Tonoli S, Tortini R, Valdagni R, Vavassori V Marvaso G, CODRAL (Board of Directors of Radiation Oncology Departments in Lombardy) network (2020) COVID-19 Outbreak and Cancer Radiotherapy Disruption in Lombardy, Northern Italy. Clinical oncology (Royal College of Radiologists (Great Britain)), 32(7), e160–e161. https://doi.org/https://doi.org/10.1016/j.clon.2020.04.007
Campi R, Amparore D, Capitanio U, Checcucci E, Salonia A, Fiori C, Minervini A, Briganti A, Carini M, Montorsi F, Serni S, Porpiglia F (2020) Assessing the burden of Nondeferrable major uro-oncologic surgery to guide prioritisation strategies during the COVID-19 pandemic: insights from three Italian high-volume referral centres. Eur Urol 78(1):11–15. https://doi.org/10.1016/j.eururo.2020.03.054
Stedman M, Lunt M, Davies M, Gibson M, Heald A (2020) COVID-19: Generate and apply local modelled transmission and morbidity effects to provide an estimate of the variation in overall relative healthcare resource impact at general practice granularity. Int J Clin Pract 74(9):e13533. https://doi.org/10.1111/ijcp.13533
Wallis C, Novara G, Marandino L, Bex A, Kamat AM, Karnes RJ, Morgan TM, Mottet N, Gillessen S, Bossi A, Roupret M, Powles T, Necchi A, Catto J, Klaassen Z (2020) Risks from deferring treatment for genitourinary cancers: a collaborative review to aid triage and management during the COVID-19 pandemic. Eur Urol 78(1):29–42. https://doi.org/10.1016/j.eururo.2020.04.063
Cortiula F, Pettke A, Bartoletti M, Puglisi F, Helleday T (2020) Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann Oncol Official J Europ Soc Med Oncol 31(5):553–555. https://doi.org/10.1016/j.annonc.2020.03.286
Desideri I, Francolini G, Ciccone LP, Stocchi G, Salvestrini V, Aquilano M, Greto D, Bonomo P, Meattini I, Scotti V, Scoccianti S, Simontacchi G, Livi, L (2020) Impact of COVID-19 on patient-doctor interaction in a complex radiation therapy facility. Supportive Care Cancer Official J Multinational Assoc Support Care Cancer, pp 1–7. Advance online publication. https://doi.org/https://doi.org/10.1007/s00520-020-05793-3
Meattini I, Franco P, Belgioia L, Boldrini L, Botticella A, De Santis MC, Marvaso G, Montesi G, Parisi S, Triggiani L, Lambertini M, Livi L (2020) Radiation therapy during the coronavirus disease 2019 (covid-19) pandemic in Italy: a view of the nation’s young oncologists. ESMO open 5(2):e000779. https://doi.org/10.1136/esmoopen-2020-000779
You B, Ravaud A, Canivet A, Ganem G, Giraud P, Guimbaud R, Kaluzinski L, Krakowski I, Mayeur D, Grellety T, Lotz JP (2020) The official French guidelines to protect patients with cancer against SARS-CoV-2 infection. Lancet Oncol 21(5):619–621. https://doi.org/10.1016/S1470-2045(20)30204-7
Braunstein LZ, Gillespie EF, Hong L, Xu A, Bakhoum SF, Cuaron J, Mueller B, McCormick B, Cahlon O, Powell S, Khan AJ (2020) Breast radiation therapy under COVID-19 pandemic resource constraints-approaches to defer or shorten treatment from a comprehensive cancer center in the United States. Adv Radiat Oncol 5(4):582–588. https://doi.org/10.1016/j.adro.2020.03.013
Thomson DJ, Palma D, Guckenberger M, Balermpas P, Beitler JJ, Blanchard P, Brizel D, Budach W, Caudell J, Corry J, Corvo R, Evans M, Garden AS, Giralt J, Gregoire V, Harari PM, Harrington K, Hitchcock YJ, Johansen J, Kaanders J, Koyfman S, Langendijk JA, Le QT, Lee N, Margalit D, Mierzwa M, Porceddu S, Soong YL, Sun Y, Thariat J, Waldron J, Yom SS (2020) Practice recommendations for risk-adapted head and neck cancer radiotherapy during the COVID-19 pandemic: An ASTRO-ESTRO consensus statement. Radiotherapy Oncol J Europ Soc Therapeutic Radiol Oncol 151:314–321. https://doi.org/10.1016/j.radonc.2020.04.019
Funding
Open access funding provided by Università degli Studi di Firenze within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Francolini, G., Desideri, I., Stocchi, G. et al. Impact of COVID-19 on workload burden of a complex radiotherapy facility. Radiol med 126, 717–721 (2021). https://doi.org/10.1007/s11547-021-01338-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-021-01338-8