Abstract
Objective
To report our experience with the use of intravoxel incoherent motion (IVIM) magnetic resonance imaging (MRI) and dynamic contrast-enhanced (DCE)-MRI in bone marrow before and after administration of granulocyte colony-stimulating factor (GCSF). Moreover, a small series of patients with bone metastases from breast cancer have been evaluated by IVIM DW-MRI and DCE-MRI before and after GCSF administration.
Materials and methods
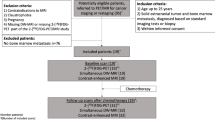
We studied with IVIM-MRI and DCE-MRI 14 patients with rectal or uterine cervix cancer studied before and 4–18 days after administration of GCSF; the second MR examination was obtained after three chemotherapy courses. IVIM perfusion fraction (f), pseudo-diffusion coefficient (D*), true diffusion coefficient (D) and apparent diffusion coefficient (ADC) as well area under the curve at 60 s (AUC60) were calculated for bone marrow before and after GCSF administration. Moreover, two different IVIM parametric maps (i.e., ADC and ADClow) were generated by selecting two different intervals of b values (0–1000 and 0–80, respectively). Furthermore, four patients affected by pelvic bone metastases from breast adenocarcinoma who received GCSF administration were also qualitatively evaluated for evidence of lesions on ADC maps, ADClow maps and DCE-MRI.
Results
ADC, D, D*, f and AUC60 values were significantly higher in hyperplastic bone marrow than in untreated bone marrow (p values < 0.0001, < 0.0001, < 0.001, < 0.001, < 0.0001, respectively). All bone metastases were clearly differentiable from hyperplastic bone marrow on ADClow maps, but not on ADC maps and DCE-MRI.
Conclusion
MR functional imaging techniques, such as DW-, IVIM DW- and DCE-MRI are effective tools in assessing the response of bone marrow to the administration of growth factors. Although an overlap between signal of hyperplastic bone marrow and lytic bone metastases can occur on ADC maps and DCE-MRI, evaluation of ADClow maps by IVIM DW-MRI could permit to differentiate hyperplastic bone marrow from lytic bone metastases. Further studies are needed to confirm our data.


Similar content being viewed by others
References
O’Connor JP, Jackson A, Parker GJ et al (2007) DCE-MRI biomarkers in the clinical evaluation of antiangiogenic and vascular disrupting agents. Br J Cancer 96:189–195
Evelhoch JL (1999) Key factors in the acquisition of contrast kinetic data for oncology. J Magn Reson Imaging 10:254–259
Li SP, Padhani AR, Makris SA (2011) Dynamic contrast-enhanced magnetic resonance imaging and blood oxygenation level-dependent magnetic resonance imaging for the assessment of changes in tumor biology with treatment. J Natl Cancer Inst Monogr 43:103–107
Gaeta M, Benedetto C, Minutoli F et al (2014) Use of diffusion-weighted, intravoxel incoherent motion, and dynamic contrast-enhanced MR imaging in the assessment of response to radiotherapy of lytic bone metastases from breast cancer. Acad Radiol 21:1286–1293
Le Bihan D, Breton E, Lallemand D et al (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 168:497–505
Stejskal EO, Tanner JE (1965) Spin diffusion measurements: spin echoes in the presence of a time-dependent field gradient. JChemPhys 42:288–292
Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intra-voxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401–407
Patel J, Sigmund EE, Rusinek H, Oei M, Babb JS, Taouli B (2010) Diagnosis of cirrhosis with intravoxel incoherent motion diffusion MRI and dynamic contrast-enhanced MRI alone and in combination: preliminary experience. J Magn Reson Imaging 31:589–600
Luciani A, Vignaud A, Cavet M et al (2008) Liver cirrhosis: intravoxel incoherent motion MR imaging–pilot study. Radiology 249:891–899
Chow AM, Gao DS, Fan SJ et al (2012) Liver fibrosis: an intravoxel incoherent motion (IVIM) study. J Magn Reson Imaging 36:159–167
Lemke A, Laun FB, Klauss M et al (2009) Differentiation of pancreas carcinoma from healthy pancreatic tissue using multiple b-values: comparison of apparent diffusion coefficient and intravoxel incoherent motion derived parameters. InvestRadiol 44:769–775
Ichikawa S, Motosugi U, Ichikawa T, Sano K, Morisaka H, Araki T (2013) Intravoxel incoherent motion imaging of the kidney: alterations in diffusion and perfusion in patients with renal dysfunction. Magn Reson Imaging 31:414–417
Wirestam R, Borg M, Brockstedt S, Lindgren A, Holtas S, Stahlberg F (2001) Perfusion-related parameters in intravoxel incoherent motion MR imaging compared with CBV and CBF measured by dynamic susceptibility-contrast MR technique. Acta Radiol 42:123–128
Federau C, Maeder P, O’Brien K, Browaeys P, Meuli R, Hagmann P (2012) Quantitative measurement of brain perfusion with intravoxel incoherent motion MR imaging. Radiology 265:874–881
Padhani AR, Gogbashian A (2011) Bony metastases: assessing response to therapy with whole-body diffusion MRI. Cancer Imaging 11:S129–S145
Wu LM, Gu HY, Zheng J et al (2011) Diagnostic value of whole-body magnetic resonance imaging for bone metastases: a systematic review and meta-analysis. J Magn Reson Imaging 34:128–135
Hartman RP, Sundaram M, Okuno SH, Sim FH (2004) Effect of granulocyte-stimulating factors on marrow of adult patients with musculoskeletal malignancies: incidence and MRI findings. AJR 183:645–653
Ballon D, Watts R, Dyke JP et al (2004) Imaging therapeutic response in human bone marrow using rapid whole-body MRI. Magn Reson Med 52:1234–1238
Fletcher BD, Wall JE, Hanna SL (1993) Effect of hematopoietic growth factors on MR images of bone marrow in children undergoing chemotherapy. Radiology 189:745–751
Padhani AR, Koh DM, Collins DJ (2011) Whole- body diffusion-weighted MR imaging in cancer: current status and research directions. Radiology 261:700–718
Padhani AR, van Ree K, Collins DJ, D’Sa S, Makris SA (2013) Assessing the relation between bone marrow signal intensity and apparent diffusion coefficient in diffusion-weighted MRI. AJR 200:163–170
Doot RK, Dunnwald LK, Schubert EK et al (2007) Dynamic and static approaches to quantifying 18F-FDG uptake for measuring cancer response to therapy, including the effect of granulocyte CSF. J Nucl Med 48:920–925
Messiou C, Collins DJ, Morgan VA, De Souza NM (2011) Optimising diffusion weighted MRI for imaging metastatic and myeloma bone disease and assessing reproducibility. Eur Radiol 21:1713–1718
Cohen AD, Schieke MC, Hohenwalter MD, Schmainda KM (2015) The effect of low b-values on the intravoxel incoherent motion derived pseudodiffusion parameter in liver. Magn Reson Med 73:306–311
Takahara T, Kwee TC (2012) Low b-value diffusion-weighted imaging: emerging applications in the body. J Magn Reson Imaging 35:1266–1273
Dijkstra H, Baron P, Kappert P, Oudkerk M, Sijens PE (2012) Effects of microperfusion in hepatic diffusion weighted imaging. Eur Radiol 22:891–899
Gao Q, Srinivasan G, Magin RL, Zhou XJ (2011) Anomalous diffusion measured by a twice-refocused spin echo pulse sequence: analysis using fractional order calculus. J Magn Reson Imaging 33(5):1177–1183
Koh DM, Collins DJ, Orton MR (2011) Intravoxel incoherent motion in body diffusion-weighted MRI: reality and challenges. AJR 196:1351–1361
Li SP, Padhani AR (2012) Tumor response assessments with diffusion and perfusion MRI. J Magn Reson Imaging 35:745–763
Lieschke GJ, Burgess A (1992) Granulocyte colony-stimulating factor and granulocyte-macrophage colony-simulating factor. N Engl J Med 327:28–35
Pelletier L, Regnard J, Fellmann D, Charbord P (2000) An in vitro model for the study of human bone marrow angiogenesis: role of hematopoietic cytokines. Lab Invest 80:501–511
Altehoefer C, Bertz H, Ghanem NA, Langer M (2001) Extent and time course of morphological changes of bone marrow induced by granulocyte-colony stimulating factor as assessed by magnetic resonance imaging of healthy blood stem cell donors. J Magn Reson Imaging 14(2):141–146
Vanel D, Casadei R, Alberghini M, Razgallah M, Busacca M, Albisinni U (2009) MR imaging of bone metastases and choice of sequence: spin echo, in-phase gradient echo, diffusion, and contrast medium. Semin Musculoskelet Radiol 13:97–103
Messiou C, Collins DJ, Morgan VA et al (2010) Quantifying sclerotic bone metastases with 2D ultra short TE MRI: a feasibility study. Cancer Biomark 7:211–218
Zweifel M, Padhani AR (2010) Perfusion MRI in the early clinical development of antivascular drugs: decorations of decision making tools? Eur J Nucl Med Mol Imaging 37:S164–S182
Leach MO, Brindle KM, Evelhoch JL et al (2005) The assessment of antiangiogenic and antivascular therapies in early-stage clinical trials using magnetic resonance imaging: issues and recommendations. Br J Cancer 92:1599–1610
Andreou A, Koh DM, Collins DJ et al (2013) Measurement reproducibility of perfusion fraction and pseudodiffusion coefficient derived by intravoxel incoherent motion diffusion-weighted MR imaging in normal liver and metastases. Eur Radiol 23:428–434
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical approval
The study was approved by our institutional review board committee.
Informed consent
Informed consent was obtained from each patient before each examination.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Minutoli, F., Pergolizzi, S., Blandino, A. et al. Effect of granulocyte colony-stimulating factor on bone marrow: evaluation by intravoxel incoherent motion and dynamic contrast-enhanced magnetic resonance imaging. Radiol med 125, 280–287 (2020). https://doi.org/10.1007/s11547-019-01115-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-01115-8