Abstract
Objective
Computed tomography (CT) is the gold standard for evaluating glenoid bone loss in patients with glenohumeral dislocations. The aim of this study was to verify if magnetic resonance imaging (MRI) can quantify the area of bone loss without any significant difference from CT.
Materials and methods
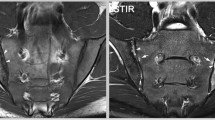
Twenty-three patients, who had experienced one or more post-traumatic unilateral glenohumeral dislocations, underwent MRI and CT. MR and multiplanar reconstruction CT images were acquired in the sagittal plane: the glenoid area and the area of bone loss were calculated using the PICO method. Mean values, percentages, Cohen’s kappa coefficients and Bland-Altman plots were all used to confirm the working hypothesis.
Results
The mean glenoid surface area was 575.29 mm2 as measured by MRI, and 573.76 mm2 as measured by CT; the calculated mean glenoid bone loss was respectively 4.38% and 4.34%. The interobserver agreement was good (k>0.81), and the coefficient of variance was 5% of the mean value using both methods. The two series of measurements were within two standard deviations of each other.
Conclusions
MRI is a valid alternative to CT for measuring glenoid bone loss in patients with glenohumeral dislocation.
Riassunto
Obiettivo
La tomografia computerizzata (TC) è il gold standard nella valutazione del danno osseo glenoideo in pazienti con lussazione gleno-omerale. Lo scopo dello studio è verificare se la risonanza magnetica (RM) può quantificare l’area di danno osseo senza significative differenze rispetto alla TC.
Materiali e metodi
Ventitre pazienti con uno o più episodi di lussazione traumatica gleno-omerale unilaterale sono stati sottoposti a RM e TC. Sono state acquisite le ricostruzioni MPR in TC e le immagini RM sul piano sagittale: la misura dell’area della glena e la misura del danno osseo sono state effettuate utilizzando il metodo PICO. Medie, percentuali, test di concordanza K di Cohen e Bland-Altman test sono stati elaborati per confermare l’ipotesi di lavoro.
Risultati
La misura dell’area glenoidea risulta di 575,29 mm2 con RM e di 573,76 mm2 con TC e le rispettive misure del deficit glenoideo sono di 4,38% e 4,34%. La concordanza inter-osservatore in TC e RM è risultata buona con k>0,81, il coefficiente di varianza è <5% del valor medio sia in TC che RM. Le due serie di misurazioni sono comprese entro 2 deviazioni standard.
Conclusioni
La RM è una valida alternativa alla TC nella misurazione del danno osseo glenoideo in pazienti con dislocazioni gleno-omerali.
Similar content being viewed by others
References/Bibliografia
Lazarus MD, Sidles JA, Harryman DT 2nd, Matsen III FA (1996) Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability: a cadaveric model. J Bone Surg Am 78:94–102
Itoi E, Lee SB, Berglund LJ et al (2000) The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 82:35–46
Gerber C, Nyffeler RW (2002) Classification of glenohumeral joint instability. Clin Orthop Rel Res 400:65–76
Tauber M, Resch H, Forstner R et al (2004) Reason for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg 13:279–285
Balg F, Boileau P (2007) The instability severity index score. A simple preoperative score to select patients for arthroscopic or open shoulder stabilization. J Bone Joint Surg Br 89:1470–1477
Mologne TS, Provencher MT, Menzel KA et al (2007) Arthroscopic stabilization in patients with an inverted pear glenoid. Results in patients with bone loss of the anterior glenoid. Am J Sports Med 35:1276–1283
Bigliani LU, Newton PM, Steinmann SP et al (1998) Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med 26:41–45
Provencher MT, Bhatia S, Ghodadra NS et al (2010) Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg 92:133–151
Sugaya H, Moriishi J, Dohi M et al (2003) Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 85:878–884
Baudi P, Righi P, Bolognesi D et al (2005) How to identify and calculate glenoid bone deficit. Chir Organi Mov 90:145–152
Jones R, Payne B (eds) (1997) Clinical investigation and statistics in laboratory medicine. ACB Venture Publications, London
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Altman DG (ed) (1991) Practical statistics for medical research. Chapman and Hall, London
Bland JM, Altman DG (1986) Statistical method for assessing agreement between two methods of clinical measurement. Lancet 8476:307–310
Sugaya H, Moriishi J, Kamisawa I, Tsuchya A (2006) Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am 88:159–169
Burkhart SS, De Beer JF, Tehrany AM, Parten PM (2002) Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 18:488–491
Lo IK, Parten PM, Burkhart SS (2004) The inverted pear glenoid: an indicator of significant bone loss. Arthroscopy 20:169–174
Huijsmans PE, Haen PS, Kidd M et al (2007) Quantification of a glenoid defect with three-dimensional computed tomography and magnetic resonance imaging: a cadaveric study. J Shoulder Elbow Surg 16:803–809
Griffith JF, Yung PS, Antonio GE et al (2007) CT compared with Arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol 189:1490–1493
Magarelli N, Milano G, Baudi P et al (2012) Comparison between 2D and 3D computed tomography evaluation of glenoid bone defect in unilateral anterior gleno-humeral instability. Radiol Med 117:102–111
Beltran J, Bencardino J, Mellado J et al (1997) MR arthrography of the shoulder: variants and pitfalls. Radiographics 17:1403–1412
Chandnani VP, Gagliardi JA, Murnane TG et al (1995) Glenohumeral ligaments and shoulder capsular mechanism: evaluation with MR arthrography. Radiology 196:27–32
Garneau RA, Renferw DL, Moore TE et al (1991) Glenoid labrum: evaluation with MR imaging. Radiology 179:519–522
Palmer WE, Brown JH, Rosenthal DI (1994) Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology 190:645–651
Stoller DW (1997) MR arthrography of the glenohumeral joint. Radiol Clin North Am 35:97–116
Guglielmi G, Biccari N, Mangano F, Toffanin R (2010) 3T magnetic resonance imaging of the muscoloskeletal system. Radiol Med 115:151–174
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stecco, A., Guenzi, E., Cascone, T. et al. MRI can assess glenoid bone loss after shoulder luxation: inter- and intra-individual comparison with CT. Radiol med 118, 1335–1343 (2013). https://doi.org/10.1007/s11547-013-0927-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-013-0927-x