Abstract
Purpose
This study evaluated transition-point morphology for defining the nature of bowel obstructions.
Materials and methods
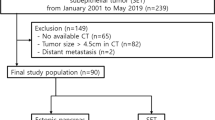
Computed tomography (CT) examinations of 95 patients affected by severe bowel obstruction (23 neoplastic, 72 nonneoplastic) were retrospectively reviewed.
Results
The transition point was identified in 89 patients (94%); morphology in relation to the proximal loop was concave in 64 cases (68%), linear in five (5%) and convex in 20 (21%). Concave transition-point morphology was indicative of a nonneoplastic condition, with sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy values of 89%, 100%, 100%, 74% and 92%, respectively. A linear shape had almost identical incidence among neoplastic (60%) and nonneoplastic (40%) conditions. A convex appearance correlated with neoplastic disease with sensitivity, specificity, PPV, NPV and diagnostic accuracy values of 87%, 100%, 100%, 96% and 97%, respectively.
Conclusions
In the case of bowel obstruction, transitionpoint detection indicates the obstruction site, whereas its morphological evaluation can contribute to defining the nature of the obstruction. A concave morphology indicates a nonneoplastic condition with a high probability; a convex morphology correlates with neoplastic disease, whereas linearity is not significant.
Riassunto
Obiettivo
Scopo del nostro lavoro è stato valutare la morfologia del punto di transizione nella definizione della natura di un’occlusione.
Materiali e metodi
Sono stati valutati retrospettivamente gli esami in tomografia computerizzata (TC) di 95 pazienti affetti da occlusione intestinale di grado severo (23 neoplastiche, 72 non neoplastiche) ed è stata considerata la morfologia del punto di transizione.
Risultati
Il punto di transizione era evidente in 89 pazienti (94%) e la sua morfologia rispetto all’ansa a monte era concava in 64 pazienti (68%); lineare in 5 (5%); convessa in 20 (21%). Una morfologia concava del punto di transizione è risultata indicativa di una condizione non neoplastica, con valori di sensibilità, specificità, valore predittivo positivo (VPP), valore predittivo negativo (VPN) ed accuratezza diagnostica rispettivamente di 89%, 100%, 100%, 74% e 92%. Un aspetto lineare ha presentato incidenza quasi sovrapponibile nei casi di occlusione neoplastica (60%) e non neoplastica (40%). Un aspetto convesso è risultato correlato a patologia neoplastica, con valori di sensibilità, specificità, VPP, VPN ed accuratezza diagnostica rispettivamente di 87%, 100%, 100%, 96% e 97%.
Conclusioni
Nelle occlusioni intestinali il riconoscimento del punto di transizione indica la sede dell’occlusione, mentre la sua valutazione morfologica può contribuire a definirne la natura. Una morfologia concava indica, con elevato grado di probabilità, una condizione non neoplastica; una morfologia convessa, un’occlusione neoplastica, mentre un aspetto lineare non è significativo.
Similar content being viewed by others
References/Bibliografia
Landwehr P (2006) Emergency radiology of bowel obstructions. Chirurg 77:889–897
Gatsoulis N, Roukounakis N, Kafetzis I et al (2004) Surgical management of large bowel obstruction due to colonic cancer. Tech Coloproctol 8(Suppl 1):s82–s84
Aufort S, Charra L, Lesnik A et al (2005) Multidetector CT of bowel obstruction: value of post-processing. Eur Radiol 15:2323–2329
Markus JB, Somers S, Franic SE et al (1989) Interobserver variation in the interpretation of abdominal radiographs. Radiology 171:69–71
Furukawa A, Yamasaki M, Furuichi K et al (2001) Helical CT in the diagnosis of small bowel obstruction. Radiographics 21:341–355
Gazelle GS, Goldberg MA, Wittenberg J et al (1994) Efficacy of CT in distinguishing small-bowel obstruction from other causes of small-bowel dilatation. AJR Am J Roentgenol 162:43–47
Frager D, Rovno HD, Baer JW et al (1998) Prospective evaluation of colonic obstruction with computed tomography. Abdom Imaging 23:141–146
Maglinte DD, Balthazar EJ, Kelvin FM, Megibow AJ (1997) The role of radiology in the diagnosis of small-bowel obstruction. AJR Am J Roentgenol l68:1171–1180
Angelelli G, Macarini L, Di Giulio G (1991) The potentials of computed tomography in the study of mechanical ileus of the small intestine. Radiol Med 82:629–634
Catalano O (1997) The faeces sign. A CT finding in small-bowel obstruction. Radiologe 37:417–419
Maglinte DD, Heitkamp DE, Howard TJ et al (2003) Current concepts in imaging of small bowel obstruction. Radiol Clin North Am 41:263–283
Suri S, Gupta S, Sudhakar PJ et al (1999) Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol 40:422–428
Angelelli G, Moschetta M, Binetti F et al (2010) Prognostic value of MDCT in malignant large-bowel obstructions. Radiol Med 115:747–757
Moschetta M, Stabile Ianora AA, Pedote P et al (2009). Prognostic value of multidetector computed tomography in bowel infarction. Radiol Med 114:780–791
Angelelli G, Moschetta M, Sabato L et al (2010) Value of “protruding lips” sign in malignant bowel obstructions. Eur J Radiol, in press. doi:10.1016/j. ejrad.2010.09.034
Balthazar EJ (1994) For suspected small-bowel obstruction and an equivocal plain film, should we perform CT or a small-bowel series? AJR Am J Roentgenol 163:1260–1261
Megibow AJ, Balthazar EJ, Cho KC et al (1991) Bowel obstruction: evaluation with CT. Radiology 180:313–318
Taourel PG, Fabre JM, Pradel JA et al (1995) Value of CT in the diagnosis and management of patients with suspected acute small-bowel obstruction. AJR Am J Roentgenol 165:1187–1192
Sinha R, Verma R (2005) Multidetector row computed tomography in bowel obstruction. Part 1. Small bowel obstruction. Clin Radiol 60:1058–1067
Paulson EK, Jaffe TA, Thomas J et al (2004) MDCT of patients with acute abdominal pain: a new perspective using coronal reformations from submillimeter isotropic voxels. AJR Am J Roentgenol 183:899–906
Hodel J, Zins M, Desmottes L et al (2009) Location of the transition zone in CT of small-bowel obstruction: added value of multiplanar reformations. Abdom Imaging 34:35–41
Mayo-Smith WW, Wittenberg J, Bennett GL et al (1995) The CT small bowel faeces sign: description and clinical significance. Clin Radiol 50:765–767
Fuchsjäger MH (2002) The smallbowel feces sign. Radiology 225:378–379
Lazarus DE, Slywotsky C, Bennett GL et al (2004) Frequency and relevance of the “small-bowel feces” sign on CT in patients with small-bowel obstruction. AJR Am J Roentgenol 183:1361–1366
Maglinte DD, Reyes BL, Harmon BH et al (1996) Reliability and role of plain film radiography and CT in the diagnosis of small-bowel obstruction. AJR Am J Roentgenol 167:1451–1455
Fukuya T, Hawes DR, Lu CC et al (1992) CT diagnosis of small-bowel obstruction: efficacy in 60 patients. AJR Am J Roentgenol 158:765–772
Buckley JA, Fishman EK (1998) CT evaluation of small bowel neoplasms: spectrum of disease. Radiographics 18:379–392
Buck JL, Sobin LH (1990) Carcinoids of the gastrointestinal tract. Radiographics 10:1081–1095
Sato T, Sakai Y, Sonoyama A et al (1984) Radiologic spectrum of rectal carcinoid tumors. Gastrointest Radiol 9:23–26
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angelelli, G., Moschetta, M., Cosmo, T. et al. CT diagnosis of the nature of bowel obstruction: morphological evaluation of the transition point. Radiol med 117, 749–758 (2012). https://doi.org/10.1007/s11547-011-0770-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-011-0770-x