Abstract
Purpose
The aim of our prospective study was to compare the diagnostic accuracy of early, delayed and dual-time-point positron emission tomography (PET) acquisition with contrast enhanced computed tomography (CT) within a PET-CT examination in the evaluation of pulmonary solitary nodules (SPNs).
Materials and methods
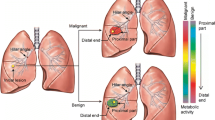
Thirty patients were enrolled in the study. All the patients underwent a dual-time-point PET-CT examination. Whole-body PET images were acquired at 50 min after fluorine18-fluorodeoxyglucose (18F-FDG) administration (early), followed by a chest acquisition (delayed). Lung nodules with maximum standardised uptake value SUVmax ≥2.5 were considered malignant. SUVmax was calculated on early and delayed images; SUV increasing ≥10% (Δ SUVmax) was considered suggestive of malignancy. Absence of significant lung nodule enhancement (<15 Δ HU) at CT was considered strongly predictive of benignity. For the CT morphological assessment, the irregularity of the shape of each lesion was rated. PET-CT results were related to histological assays and clinical records. Diagnostic accuracy was assessed by area under the receiveroperarting characteristic (ROC) curves analysis.
Results
Early and delayed SUVmax of malignant nodules were significantly higher than those of benign disease. Early SUVmax sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 77%, 91%, 79.5% and 66.7%; delayed SUVmax corresponding values were 77%, 66%, 74% and 66%; dual-time-point SUVmax values were 83%, 67%, 75% and 74%; ΔHU values were 94%, 34%, 67%, 96%; CT morphologic evaluation values were 61%, 46%, 60%, 47%. Area under the curve (AUC) for early SUVmax was 0.79, for delayed SUVmax 0.80, for dual-time-point SUVmax 0.85, for ΔHU 0.63 and for CT morphologic assessment 0.58.
Conclusions
In our small series of patients, early and delayed SUVmax showed comparable accuracies, whereas morphological and contrast enhanced CT evaluations showed the lowest accuracies. Dual-time-point SUVmax showed the largest AUC. However, dual-time-point SUVmax was most sensitive, whereas single-time-point SUVmax was most specific.
Riassunto
Obiettivo
Scopo del nostro studio è stato quello di comparare l’accuratezza diagnostica dell’acquisizione PET in fase precoce, in fase tardiva e dual-time associata all’esecuzione di TC con mezzo di contrasto in un’unica sessione nella valutazione del nodulo polmonare solitario (SPN).
Materiali e metodi
Presso il nostro Dipartimento sono stati sottoposti a valutazione PET-TC dual-time con mezzo di contrasto 30 pazienti con nodulo polmonare solitario. Le immagini PET total-body sono state acquisite 50 minuti dopo la somministrazione di 18F-FDG (fase precoce) seguite da un’acquisizione del torace (fase tardiva). I noduli polmonari con SUVmax≥2,5 sono stati considerati maligni. È stato calcolato il valore di SUVmax sulle immagini precoci e tardive: l’incremento (Δ SUVmax) del SUVmax tra fase precoce e fase tardiva ≥10% è stato considerato suggestivo di malignita; in valutazione TC invece è stata considerato suggestivo di benignità l’assenza di un significativo incremento di densità (<15 HU) tra l’acquisizione basale e quella post-contrastografica. Le caratteristiche morfologiche dei noduli alla TC sono state analizzate quantificando l’irregolarità della forma della lesione in una scala da 1 a 4. I risultati della PET-TC sono stati correlati ai dati clinici e a campioni istologici. L’accuratezza diagnostica è stata misurata mediante curva ROC.
Risultati
Il valore di SUVmax in fase precoce e tardiva nei noduli maligni è risultato significativamente più elevato di quello riscontrato per i noduli benigni. La sensibilità, la specificità, il VPP e il VPN del SUVmax ottenuto in fase precoce sono state del 77%, 91%, 79,5% e 66,7% rispettivamente; in fase tardiva abbiamo ottenuto valori di 83%, 67%, 75% e 74% rispettivamente. La differenza del valore in HU (ΔHU) tra acquisizione TC basale e quella post-contrastografica ha mostrato valori di sensibilità del 94%, di specificità del 34%, VPP del 67% e VPN del 96%. La valutazione TC morfologica ha riportato valori di sensibilita, specificita, di VPP e di VPN di 61%, 46%, 60%, 47%. La curva AUC del valore di SUVmax in fase precoce è stata di 0,79, in fase tardiva è stata di 0,80, riguardo all’acquisizione dual-time (Δ SUVmax) di 0,85 e riguardo al ΔHU di 0,63 e per quanto riguarda la valutazione morfologica di 0,58.
Conclusioni
Nel nostro piccolo gruppo di pazienti il valore di SUVmax sia in fase precoce che tardiva ha mostrato accuratezza sovrapponibile, le valutazioni TC morfologica e contrastografica hanno mostrato l’accuratezza piu bassa. Il valore di SUVmax calcolato in dual-time (Δ SUVmax) ha mostrato l’accuratezza diagnostica maggiore. Tuttavia il valore di SUVmax in dual-time pur mostrandosi piu sensibile rispetto al valore di SUVmax ottenuto con singola acquisizione, è risultato meno specifico.
Similar content being viewed by others
References/Bibliografia
Tuddenham WI (1984) Glossary of terms for thoracic radiology: recommendations of the Nomenclature Committee of the Fleischner Society. AJR Am J Roentgenol 143:509–517
Bunyaviroch T, Coleman RE (2006) PET evaluation of lung cancer. J Nucl Med 47:451–469
Winer-Muram HT (2006) The solitary pulmonary nodule. Radiology 239:34–49
Henschke CI, McCauley DI, Yankelevitz DF et al (1999) Early lung cancer action project: overall design and findings from baseline screening. Lancet 354:99–105
Diederich S, Wormanns D, Semik M et al (2002) Screening for early lung cancer with low-dose spiral CT: prevalence in 817 asymptomatic smokers. Radiology 222:773–781
Swensen SJ, Jett JR, Hartman TE et al (2003) Lung cancer screening with CT: Mayo Clinic experience. Radiology 226:756–761
Siegelman SS, Khouri L, Frank E et al (1986) Solitary pulmonary nodules: CT assessment. Radiology 160:307–312
Tang AWK, Moss HA, Robertson RJH (2003) The solitary pulmonary nodule. Eur J Radiol 45:69–77
Ost D, Fein A (2000) Evaluation and management of the solitary pulmonary nodule. Am J Respir Crit Care Med 162:782–787
Sergiacomi G, Schillaci O, Leporace M et al (2006) Integrated multislice CT and Tc-99m Sestamibi SPECT-CT evaluation of solitary pulmonary nodules. Radiol Med 111:213–224
Hara T, Kosaka N, Suzuki T et al (2003) Uptake rates of 18Ffluorodeoxyglucose and 11C-choline in lung cancer and pulmonary tuberculosis: a positron emission tomography study. Chest 124:893–901
Lowe VJ, Fletcher JW, Gobar L et al (1998) Prospective investigation of positron emission tomography in lung nodules. J Clin Oncol 16:1075–1084
de Geus-Oei LF, van Krieken JH, Aliredjo RP et al (2007) Biological correlates of FDG uptake in non-small cell lung cancer. Lung Cancer 55:79–87
Van Baardwijk A, Dooms C, van Suylen RJ et al (2007) The maximum uptake of (18)F-deoxyglucose on positron emission tomography scan correlates with survival, hypoxia inducible factor-1alpha and GLUT-1 in non small cell lung cancer. Eur J Cancer 43:1392–1398
Gould MK, Maclean CC, Kuschner WG et al (2001) Accuracy of positron emission tomography for diagnosis of pulmonary nodules and mass lesions: a meta-analysis. JAMA 285:914–924
Zhuang H, Pourdehnad M, Lambright ES et al (2001) Dual-time point 18FFDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med 42:1412–1417
Arena V, Skanjeti A, Casoni R et al (2008) Dual-phase FDG-PET: delayed acquisition improves hepatic detectability of pathological uptake. Radiol Med 113:875–886
Núñez R, Kalapparambath A, Varela J (2007) Improvement in sensitivity with delayed imaging of pulmonary lesions with FDG-PET. Rev Esp Med Nucl 26:196–207
Matthies A, Hickeson M, Cuchiara A, Alavi A (2002) Dual-time point 18FFDG PET for the evaluation of pulmonary nodules. J Nucl Med 43:871–875
Kim SK, Allen-Auerbach M, Goldin J et al (2007) Accuracy of PET/CT in characterization of solitary pulmonary lesions. J Nucl Med 48:214–220
de Geus-Oei LF, van der Heijden HF, Corstens FH, Oyen WJ (2007) Predictive and prognostic value of FDG-PET in nonsmall-cell lung cancer: a systematic review. Cancer 110:1654–1664
Li F, Sone S, Abe H et al (2004) Malignant versus benign nodules at CT screening for lung cancer: comparison of thin-section CT findings. Radiology 233:793–798
Ost D, Fein AM, Feinsilver SH (2003) Clinical practice: the solitary pulmonary nodule. N Engl J Med 348:2535–2542
Yankelevitz DF, Henschke CI (2000) Small solitary pulmonary nodules. Clin North Am 38:471–478
Cumming SR, Lillington GA, Richard RJ (1986) Estimating the probability of malignancy in solitary pulmonary nodules. A Bayesian approach. Am Rev Respir Dis 134:449–452
Zerhouni EA, Stitik FP, Siegelman SS et al (1986) CT of the pulmonary nodule: a cooperative study. Radiology 160:319–327
Nesbitt JC, Putnam JB, Walsh GL et al (1995) Survival in earlystage lung cancer. Ann Thorac Surg 60:466–472
Shields TW (1993) Surgical therapy for carcinoma of the lung. Clin Chest Med 14:121–147
Hustinx R, Smith RJ, Benard F et al (1999) Dual-time point fluorine-18 fluorodeoxyglucose positron emission tomography: a potential method to differentiate malignancy from inflammation and normal tissue in head and neck. Eur J Nucl Med 26:1345–1348
Orlacchio A, Schillaci O, Antonelli L et al (2007) Solitary pulmonary nodules: morphological and metabolic characterisation by FDG-PET-MDCT. Radiol Med 112:157–173
Alkhawaldeh K, Bural G, Kumar R, Alavi A (2008) Impact of dual-timepoint 18FFDG PET imaging and partial volume correction in the assessment of solitary pulmonary nodules. Eur J Nucl Med Mol Imaging 35:246–252
Hashimoto Y, Tsujikawa T, Kondo C et al (2006) Accuracy of PET for diagnosis of solid pulmonary lesions with 18FFDG uptake below the standardized uptake value of 2.5. J Nucl Med 47:426–431
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schillaci, O., Travascio, L., Bolacchi, F. et al. Accuracy of early and delayed FDG PET-CT and of contrast-enhanced CT in the evaluation of lung nodules: a preliminary study on 30 patients. Radiol med 114, 890–906 (2009). https://doi.org/10.1007/s11547-009-0400-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0400-z