Abstract
Purpose
The treatment of pain in bone metastases is currently multidisciplinary. Among the various therapies, local radiotherapy is the gold standard for pain palliation from single metastasis, even though the maximum benefit is obtained between 12 and 20 weeks from initiation. In carefully selected patients, several ablation therapies achieve this objective in 4 weeks. The purpose of this study was to assess the technical success, effectiveness and possible complications of percutaneous ablation therapies in patients with symptomatic bone metastases.
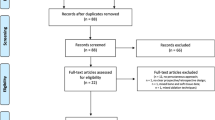
Materials and methods
From November 2003 to May 2008, ten ablation treatments were performed in ten patients with acute pain from metastatic bone lesions. Patient selection and choice of the most appropriate ablation treatment was made based on lesion characteristics. Three patients were treated with radiofrequency, one with plasma-mediated radiofrequency, two with plasma-mediated radiofrequency and cementoplasty, three with radiofrequency and cementoplasty and one with microwave.
Results
Assessments were based not only on imaging but also on the visual analogue scale (VAS) score for determining pain and on changes in morphine-equivalent doses. In both cases, 3-month follow-up showed a statistically significant reduction of pain. In no case did local complications occur either during or after treatment. Only one patient treated with radiofrequency (1/9, 11%) developed low-grade fever and general malaise during the 6 days following the procedure, compatible with a post-radiofrequency syndrome, which was treated with acetaminophen (paracetamol) only and resolved on day 7.
Conclusions
Percutaneous ablation therapies represent a safe and valuable alternative for treating localised pain from single bone metastasis, providing rapid (4-week) relief of symptoms and a significant reduction in morphine doses. This contributes to improving the quality of life of patients with metastatic disease.
Riassunto
Obiettivi
Il trattamento del dolore nelle metastasi ossee è attualmente multidisciplinare. Tra le varie terapie, la radioterapia locale è il gold-standard nella palliazione del dolore da metastasi singola, anche se il massimo beneficio si ottiene tra le 12 e le 20 settimane dall’inizio della terapia. In pazienti accuratamente selezionati, varie terapie ablative raggiungono quest’obiettivo in 4 settimane. Scopo di questo lavoro è valutare il successo tecnico, l’efficacia e le eventuali complicanze delle terapie ablative percutanee in pazienti affetti da metastasi ossee sintomatiche.
Materiali e metodi
Da novembre 2003 a maggio 2008 sono stati effettuati 10 trattamenti in 10 pazienti con dolore acuto da lesioni metastatiche ossee. La selezione dei pazienti e la scelta del trattamento ablativo più idoneo è stata fatta sulla base delle caratteristiche della lesione. Tre pazienti sono stati trattati con radiofrequenza, 1 con radiofrequenza plasma-mediata, 2 con radiofrequenza plasma mediata e cementoplastica, 3 con radiofrequenza e cementoplastica, 1 con microonde.
Risultati
La valutazione è stata effettuata non solo con imaging, ma anche con una VAS score (visual analoge scale) per la determinazione del dolore e con la variazione delle dose equivalenti di morfina. In entrambi i casi la riduzione è stata statisticamente significativa. In nessun caso si sono verificate complicanze locali sia durante che dopo il trattamento. Solamente in un paziente trattato con radiofrequenza (1/9, 11%) abbiamo riscontrato nei 6 giorni successivi al trattamento insorgenza di febbricola e malessere generale compatibile con la “sindrome post-radiofrequenza”, risoltasi poi al settimo giorno e trattata solo con acetaminofene (paracetamolo).
Conclusioni
Le tecniche ablative percutanee rappresentano una sicura e valida alternativa al trattamento del dolore localizzato da metastasi ossee singole, apportando in breve tempo (4 settimane) un miglioramento della sintomatologia e una sensibile riduzione delle dosi di morfina. Ciò concorre a migliorare la qualità della vita in pazienti affetti da malattia metastatica.
Similar content being viewed by others
References/Bibliografia
Scutellari PN, Antinolfi G, Galeotti R, Giganti M (2003) La malattia ossea metastatica. Strategia della diagnostica per immagini. Minerva Med 94:77–90
Callstrom MR, Charboneau JW, Goetz MP et al (2006) Image-guided ablation of painful metastatic bone tumors: a new and effective approach to a difficult problem. Skeletal Radiol 35:1–15
Agarawal JP, Swangsilpa T, Van Der Liden Y et al (2006) The role of external beam radiotherapy in the management of bone metastases. Clinical Oncology 18:747–760
Gangi A, Kastler B, Klinkert A, Dietermann JL (1994) Injection of alcohol into bone metastases under CT guidance. J Comput Assist Tomogr 18:932–935
Kojima H, Tanigawa N, Kariya S et al (2006) Clinical assessment of percutanoeus radiofrequency ablation for painful metastsatic bone tumors. Cardiovasc Intervent Radiol 29:1022–1026
Toyota N, Naito A, Kakizawa H et al (2005) Radiofrequency ablation therapy combined with cementoplasty for painful bone metastases: initial experience. Cardiovasc Intervent Radiol 28:578–583
Kelekis A, Lovblad KO, Mehidzade A et al (2005) Pelvic osteoplasty in osteolytic metastases: technical approach under fluoroscopic guidance and early clinical results. J Vasc Interv Radiol 16:81–88
Hierholzer J, Anselmetti G, Fuchs H et al (2003) Percotaneous osteoplasty as a treatment for painful malignant bone lesions of the pelvis and femur. J Vasc Interv Radiol 14:773–777
Dupuy DE, Hong R, Oliver B, Goldberg SN (2000) Raddiofrequency ablation of spinal tumors: temperature distribution in the spinal canal. AJR Am J Roentgenol 175:1263–1266
Simon CJ, Dupuy DE, William W (2005) Microwave ablation: principles and applications. Radiographics 25:69–83
Callstrom MR, Charboneau JW (2007). Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 10:120–131
Carrafiello G, Laganà D, Ianniello A et al (2007) Post-radiofrequency ablation syndrome after percutaneous radiofrequency of abdominal tumors: one centre experience and review of published works. Australas Radiol 51:550–554
Guaraldi M, Martoni A (2005) Metastasi ossee. In: Lopez M (ed) Oncologia medica pratica. Società editrice universitaria, Roma, pp 2131–2137
Ditonno P, Battaglia M, Selvaggi FP (2003) Tumori dell’apparato urogenitale. In: Schena FP, Selvaggi FP (eds) Malattie dei reni e delle vie urinarie. McGraw-Hill ed, Milano, pp 487–540
Pecorelli S, Sartori E, Palai N (2000) Tumori mammari. In: Grella PV, Massobrio M, Pecorelli S, Zichella L (eds) Compendio di ginecologia e ostetricia. Monduzzi Ed, Bologna, pp 381–408
Frassica FJ, Frassica DA, Lietman SA et al (2001) Metastatic bone disease. In: Chapman’s (ed) Orthopaedic surgery. Lippincott Williams & Wilkins ed, Philadelphia, pp 3469–3481
Yazawa Y, Frassica FJ, Chao EY et al (1990) Metastatic bone disease: a study of the surgical treatment of 166 pathologic humeral and femoral fractures. Clin Orthop 251:213–219
Wunderlich T, Blumlein H, Steeger D (1980) Tumor prothesis in the treatment of metastases, loosening of prothesis and fractures at the proximal femur. Z Orthop Ihre Grenzgeb 118:61–65
Tordiglione M, Luraghi R, Antognoni P (1999) Il ruolo della radioterapia palliativa e sintomatica delle metastasi ossee. Radiol Med 97:372–377
Lin A, Ray ME (2006) Targeted and systemic radiotherapy in the treatment of bone metastasis. Cancer Metastasis Rev 25:669–675
Wolrd Healt Organization (1990) Cancer pain relief and palliative care: report of a WHO expert committee. World Healt Organization, Geneve
Simon JC, Dupuy DE (2005) Image-guided ablative techniques in pelvic malignancies: radiofrequency ablation, cryoablation, microwave ablation. Surg Oncol Clin N Am 14:419–431
Simon JC, Dupuy DE (2006) Percutaneous minimally invasive therapies in the treatment of bone tumors: thermal ablation. Semin Muscoloskelet Radiol 10:137–144
Buy X, Basile A, Bierry G et al (2006) Saline-infused bipolar radiofrequency ablation of high-risk spinal and paraspinal neoplasms. AJR Am J Roentgenol 186:322–326
Georgy BA, Wong W (2007) Plasma-mediated radiofrequency ablation assisted percutaneous cement injection for treating advanced malignant vertebral compression fractures. Am J Neuroradiol 28:700–705
Mannion RJ, Wolf CJ (2000) Pain mechanisms and management: a central perspective. Clin J Pain 16:144–156
Honore P, Luger NM, Sabino MA et al (2000) Osteoprotegerin blocks bone cancer-induced skeletal destruction, skeletal pain and pain-related neurochemical reorganization of the spinal cord. Nat Med 6:521–528
Callstrom MR, Charboneau JW, Goetz MP et al (2002) Painful metastases involving bone: feasibility of percutaneous CT- and US- guided radio-frequency ablation. Radiology 224:87–97
Goetz MP, Callstrom MP, Charboneau W et al (2004) Percutaneous imageguided radiofrequncy ablation of painful metastases involving bone: a multicenter study. J Clin Oncol 22:303–306
Masala S, Manenti G, Roselli M et al (2007) Percutaneous combined therapy for painful sternal metastases: a radiofrequency thermal ablation (RFTA) and cementoplasty protocol. Anticancer Res 27:4259–4262
Carrafiello G, Laganà D, Recaldini C et al (2007) Combined treatment of ablative therapy with percutaneous radiofrequency and cementoplasty of a symptomatic metatstatic lesion of the acetabulum: case report. Australas Radiol 51(Suppl B): 344–348
Nakatsuka A, Yamakado K, Maeda M et al. (2004) Radiofrequency ablation combined with bone cement injection for the treatment of bone malignancies. J Vasc Interv Radiol 15:707–712
Hoffmann RT, Jakobs TF, Trumm C et al (2008) Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. J Vasc Interv Radiol 19:419–425
Schaefer O, Lohrmann C, Markmiller M et al (2003) Combined treatment of a spinal metastasis with radiofrequency heat ablation and vertebroplasty. AJR Am J Roentgenol 180:1075–1077
Basile A, Giuliano G, Scuderi V et al (2008) Cementoplasty in the management of painful extraspinal bone metastases: our experience. Radiol Med 113:1018–1028
Caudana R, Renzi Brivio L, Ventura L et al (2008) CT-guided percutaneous verteboplasty: personal experience in the treatment of osteoporotic fractures and dorsolumbar metastases. Radiol Med 113:114–133
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carrafiello, G., Laganà, D., Pellegrino, C. et al. Percutaneous imaging-guided ablation therapies in the treatment of symptomatic bone metastases: preliminary experience. Radiol med 114, 608–625 (2009). https://doi.org/10.1007/s11547-009-0395-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0395-5