Abstract
Purpose
Aim of the study is to demonstrate the main role of magnetic resonance imaging in the identification and characterization of lipomatous lesions of the head and neck.
Materials and methods
CT and MRI findings of 78 patients (43 male, 35 female) aged 12–80 (mean 47.5) years surgically treated for lipomatous lesions of the head and neck region between January 1995 and June 2005 were retrospectively analysed and correlated with the histological results.
Results
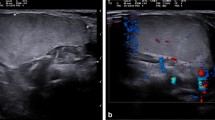
On CT images, lipomas and fibrolipomas appeared as smooth (38/50 cases) or lobulated (12/50 cases) well-defined masses associated with moderate displacement of surrounding tissues; tumours had high signal intensity on MR T1-weighted images, with relative decreasing signal on T2-weighted images. Infiltrating lipomas appeared as expansile ill-defined masses with heterogeneous signal. Angiolipomas showed a characteristic contrast enhancement on both CT and MRI. In one case of sialolipoma, the lesion appeared markedly heterogeneous in signal. MR and CT images of Madelung’s disease showed multiple symmetrical lipomatous masses involving the neck region. Intraosseous fatty lesions appeared as well-defined hypodense masses sometimes associated with cortical expansion and disruption.
Conclusions
Both CT and MRI exams are useful for detecting lipomatous lesions. MRI, however, is more accurate in the evaluation of their extent and in the characterisation of uncommon lipomatous lesions of the head and neck, and intravenous administration of gadolinium better depicts the margins of the tumour and its vascularisation.
Riassunto
Obiettivo
Lo scopo del lavoro è dimostrare il ruolo primario della risonanza magnetica nell’identificazione e nella caratterizzazione dei lipomi della regione testa-collo.
Materiali e metodi
Gli esami di tomografia computerizzata e risonanza magnetica di 78 pazienti (43 M, 35 F) di età compresa tra i 12 e gli 80 anni (media: 47,5), sottoposti ad intervento chirurgico per l’asportazione di lipomi del distretto testa-collo tra gennaio 1995 e giugno del 2005, sono stati valutati retrospettivamente e correlati successivamente ai risultati dellesame istologico.
Risultati
Nelle immagini di tomografia computerizzata i lipomi ed i fibrolipomi appaiono come masse ben definite con margini lisci (38/50 casi) o lobulati (12/50 casi) associate, con modesta dislocazione dei tessuti circostanti; le lesioni appaiono iperintense nelle immagini di risonanza magnetica ottenute con sequenze T1-pesate con riduzione proporzionale del segnale nelle immagini T2-pesate. I lipomi infiltranti appaiono come masse espansive scarsamente definite e dotate di segnale eterogeneo. Le immagini di tomografia computerizzata e di risonanza magnetica della malattia di Madelung mostrano lesioni multiple e simmetriche nel distretto testa-collo. Le lesioni intraossee appaiono come aree ipodense ben definite talora associate ad espansione e distruzione della corticale.
Conclusioni
La tomografia computerizzata e la risonanza magnetica sono entrambe utili per la diagnosi dei lipomi; la risonanza magnetica, tuttavia, costituisce la tecnica più leaccurata nella valutazione della loro estensione e nella caratterizzazione delle lesioni rare del distretto testa-collo. La somministrazione intravenosa di mezzo di contrasto definisce con maggiore dettaglio i margini del tumore ed il suo pattern di vascolarizzazione.
Similar content being viewed by others
References/Bibliografia
Kransdorf FM (1995) Benign softtissue in a large referral population: distribution of specific diagnoses by age, sex, and localisation. Am J Roentgenol 164:395–402
Som PM, Scherl MP, Rao VM, Biller HF (1986) Presentation of ordinary lipomas of the head and neck: a review. Am J Neuroradiol 7:657–664
Abdullah BJJ, Liam CK, Kaur H, Mathew KM (1997) Parapharyngeal space lipoma causing sleep apnoea. BJR 70:1063–1065
Ghandour K, Issa M (1992) Lipoma of the floor of the mouth. Oral Surg Oral Med Oral Pathol 73:59–60
Yoskovitch A, Cambronero E, Said S et al (1999) Giant lipoma of the larynx: a case report and literature review. Ear Nose Throat J 78:122–125
Canchois R, Laccourreye O, Rotenberg M et al (1995) Intrinsic infiltrating intramuscular laryngeal lipoma. Otolaryngol Head Neck Surg 112:777–779
Benson-Mitchell R, Tolley N, Croft CB, Roberts D (1994) Lipoma of the left tonsillar fossa. J Laryngol Otol 108:507–508
Fasig JH, Robinson RA, McMulloch TM et al (2001) Spindle cell lipoma of the parotid. Fine-needle aspiration and histologic findings. Arch Pathol Lab Med 125:820–821
Eckel HE, Jungehulsing O (1994) Lipoma of the hypopharynx. Preoperative diagnosis and transoral resection. J Laryngol Otol 108:174–177
Chaudhhry S, Sirpal YM (1997) Lipoma, a rare tumour of nasopharynx. Indian J Cancer 34:177–178
Yoshihara T, Kawano K, Mita N (1998) Retropharyngeal lipoma causing severe dysphagia and dyspnea. J Otolaryngol 27:363–366
Chikui T, Yonetsu K, Yoshiura K et al. (1997) Imaging findings of lipomas in the orofacial region with CY, US and MRI. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 84:88–95
Gopinath SP (1992) Intraosseous lipoma of the skull. J Neurosurg 77:976
Arslan G, Karaali K, Cubuk M et al (2000) Intraosseous lipoma of the frontal bone. Acta Radiologica 41:320–321
Sakashita H, Miyata M, Okabe K (1998) Intraosseous lipoma of the maxilla. A case report. Int J Oral Maxillofac Surg 27:63–64
Buriç N, Krasiç D, Vi‰njiç M, Katiç V (2001) Intraosseous mandibolar lipoma: a case report and review of the literature. J Oral Maxillofac Surg 59:1367–1371
Milgram JW (1988) Intraosseous lipomas. Radiologic and pathologic manifestations. Radiology 167:155
Milgram JW (1990) Malignant transformation in bone lipomas. Skel Radiol 19:347
Ayasaka N, Chino Jr T, Chino T et al (1993) Infiltrating lipoma of the mental region: report of a case. Br J Oral and Maxillofac Surg 31:388–390
Piattelli A, Fioroni M, Rubini C (2000) Intramuscular lipoma of the cheek: a case report. J Oral Maxillofac Surg 58:817–819
Dionne GP, Seemayer TA (1974) Infiltrating lipomas and angiolipoma rivisited. Cancer 33:732–738
Sugiura J, Fujiwara K, Kurahashi I, Kimura Y (1999) Infiltrating angiolipoma of the mucolabial fold: a case report and review of the literature. J Oral Maxillofac Surg 57:446–448
Bennhoff DF, Wood JW (1978) Infiltrating lipomata of the head and neck. Laryngoscope 88:839–848
Garavaglia J, Gnepp DR (1987) Intramuscular (infiltrating) lipoma of the tongue. Oral Surg Oral Med Oral Pathol 63:348–350
Takeda Y (1989) Intramuscular lipoma of the tongue. Ann Dent 48:22–24
Shirasuna k, Saka M, Watatani K, Kogo M, Matsuya T (1989) Intramuscular lipoma of the tongue. Int J Oral Maxillofac Surg 18:68–69
Bataineh AB, Mansour MJ, Abalkhail A (1996) Oral infiltrating lipomas. Br J Oral Maxillofac Surg 31:520–523
Epivatianos A, Markopoulos AK, Papanayotou P (2000) Benign tumors of adipose tissue of the oral cavity: a clinicopathologic study of 13 cases. J Oral Maxillofac Surg 58:1113–1117
Ergün SS, Kurul S, Ulay M, BilgiÇ B (2001) Infiltrating lipomatosis of the face. Ann Plast Surg 47:346–348
Cappabianca S, De Luca AM, Iscaro FM et al (1999) The identification of the criteria of malignancy and the tissue characterization of expansive processes in periskeletal soft tissues. The current role of magnetic resonance. Radiol Med 98:127–132
Munk PL, Lee MJ, Janzen DJ et al. (1997) Lipoma and liposarcoma: evaluation using CT and MR imaging. Am J Roentgenol 169:589–594
Moore PL, Goede A, Phillips DE (2001) Atypical lipoma of the tongue. J Laryngol Otol 11:859–861
Abenavoli FM, Corelli R, D’Erme G (2002) Madelung’s disease: which surgical treatment? Br J Plast Surg 55:536–537
Crim JR, Seeger LL, Yao L et al. (1992) Diagnosis of soft-tissue masses with MR Imaging: can benign masses be differentiated from malignant ones? Radiology 185:581–586
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cappabianca, S., Colella, G., Pezzullo, M.G. et al. Lipomatous lesions of the head and neck region: imaging findings in comparison with histological type. Radiol med 113, 758–770 (2008). https://doi.org/10.1007/s11547-008-0258-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-008-0258-5