Abstract
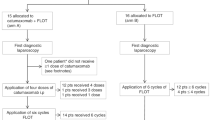
Malignant ascites is quite rare in breast cancer and is mainly associated with a lobular histology. To date, no studies have evaluated locoregional therapy for malignant ascites in breast cancer. The anti-epithelial cell adhesion molecule (EpCAM), trifunctional antibody catumaxomab was approved in the European Union for the intraperitoneal (i.p.) treatment of malignant ascites in patients with EpCAM-positive carcinomas where standard therapy is not available or no longer feasible. We report the case of a 69-year-old female with pretreated breast cancer who received i.p. catumaxomab for the treatment of malignant ascites and showed a regression of liver metastases. The patient originally underwent a left mastectomy and ipsilateral axillary lymph node dissection for an invasive ductal carcinoma in 1995. Following several lines of treatment, she was enrolled in February 2010 in a phase IIIb study (CASIMAS) investigating the safety of a 3-h i.p. catumaxomab infusion. In addition to a local benefit, as shown by an improvement in malignant ascites and a prolongation of the paracentesis-free interval with i.p. catumaxomab, a computed tomography scan, performed some weeks after catumaxomab administration, showed a regression of liver metastases. In addition to a locoregional effect on EpCAM-positive disease, i.p. catumaxomab may also show systemic effects. The use of i.p. catumaxomab for the treatment of malignant ascites due to breast cancer should be explored further in appropriate clinical studies and its possible systemic effects should also be further investigated.


Similar content being viewed by others
References
Ayantunde AA, Parsons S (2007) Pattern and prognostic factors in patients with malignant ascites: a retrospective study. Ann Oncol 18:945–949
Tamsma J (2007) The pathogenesis of malignant ascites. Cancer Treat Res 134:109–118
Smith EM, Jayson GC (2003) The current and future management of malignant ascites. Clin Oncol (R Coll Radiol) 15:59–72
Woopen H, Sehouli J (2009) Current and future options in the treatment of malignant ascites in ovarian cancer. Anticancer Res 29:3353–3359
Becker G, Galandi D, Blum HE (2006) Malignant ascites: systematic review and guideline for treatment. Eur J Cancer 42:589–597
Alt-Epping B, Nauck F (2010) Palliativmedizinische Behandlungsoptionen. In: Kiewe P, Thiel E (eds) Peritonealkarzinose und maligner aszites. UNI-MED Verlag, Berlin, pp 87–90
Heiss MM, Murawa P, Koralewski P, Kutarska E, Kolesnik OO, Ivanchenko VV, Dudnichenko AS, Aleknaviciene B, Razbadauskas A, Gore M, Ganea-Motan E, Ciuleanu T, Wimberger P, Schmittel A, Schmalfeldt B, Burges A, Bokemeyer C, Lindhofer H, Lahr A, Parsons SL (2010) The trifunctional antibody catumaxomab for the treatment of malignant ascites due to epithelial cancer: results of a prospective randomized phase II/III trial. Int J Cancer 127:2209–2221
Seimetz D, Lindhofer H, Bokemeyer C (2010) Development and approval of the trifunctional antibody catumaxomab (anti-EpCAMxanti-CD3) as a targeted cancer immunotherapy. Cancer Treat Rev 36:458–467
Went PT, Lugli A, Meier S, Bundi M, Mirlacher M, Sauter G, Dirnhofer S (2004) Frequent EpCAM protein expression in human carcinomas. Hum Pathol 35:122–128
Schmidt M, Hasenclever D, Schaeffer M, Boehm D, Cotarelo C, Steiner E, Lebrecht A, Siggelkow W, Weikel W, Schiffer-Petry I, Gebhard S, Pilch H, Gehrmann M, Lehr HA, Koelbl H, Hengstler JG, Schuler M (2008) Prognostic effect of epithelial cell adhesion molecule overexpression in untreated node-negative breast cancer. Clin Cancer Res 14:5849–5855
Spizzo G, Went P, Dirnhofer S, Obrist P, Simon R, Spichtin H, Maurer R, Metzger U, von Castelberg B, Bart R, Stopatschinskaya S, Köchli OR, Haas P, Mross F, Zuber M, Dietrich H, Bischoff S, Mirlacher M, Sauter G, Gastl G (2004) High Ep-CAM expression is associated with poor prognosis in node-positive breast cancer. Breast Cancer Res Treat 86:207–213
Ruf P, Kluge M, Jäger M, Burges A, Volovat C, Heiss MM, Hess J, Wimberger P, Brandt B, Lindhofer H (2010) Pharmacokinetics, immunogenicity and bioactivity of the therapeutic antibody catumaxomab intraperitoneally administered to cancer patients. Br J Clin Pharmacol 69:617–625
Wimberger P, Heubner M, Lindhofer H, Jäger M, Kimmig R, Kasimir-Bauer S (2009) Influence of catumaxomab on tumor cells in bone marrow and blood in ovarian cancer. Anticancer Res 29:1787–1791
Woopen H, Pietzner K, Darb-Esfahani S, Oskay-Oezcelik G, Sehouli J (2012) Extraperitoneal response to intraperitoneal immunotherapy with catumaxomab in a patient with cutaneous lymphangiosis carcinomatosa from ovarian cancer: a case report and review of the literature. Med Oncol. doi:10.1007/s12032-012-0285-x
Acknowledgments
The CASIMAS phase IIIb study, in which this patient was enrolled and treated with catumaxomab, was funded by Fresenius Biotech GmbH, Munich, Germany.
Conflict of interest
Neither the authors nor our institutions at any time receive payment or services from a third party for any aspect of the submitted work (including but not limited to grants, data monitoring board, study design, manuscript preparation, statistical analysis, etc.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petrelli, F., Borgonovo, K., Lonati, V. et al. Regression of liver metastases after treatment with intraperitoneal catumaxomab for malignant ascites due to breast cancer. Targ Oncol 8, 291–294 (2013). https://doi.org/10.1007/s11523-012-0240-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-012-0240-y