Abstract
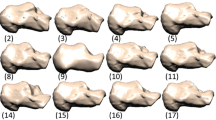
Pressure-related deep tissue injury is the term recommended by the United States National Pressure Ulcer Advisory Panel to describe a potentially life-threatening form of pressure ulcers, characterized by the presence of necrotic tissue under intact skin, and associated with prolonged compression of muscle tissue under bony prominences. In this study, a theoretical model was used to determine the relative contributions of the backrest inclination angle during prolonged wheelchair sitting, the muscle tissue stiffness and curvature of the ischial tuberosities (ITs) to the risk for injury in the gluteus muscles that pad the IT bones during sitting. The model is based on Hertz’s theory for analysis of contact pressures between a rigid half-sphere (bone) and an elastic half-space (muscle). Hertz’s theory is coupled with an injury threshold and damage law for muscle—both obtained in previous studies in rats. The simulation outputs the time-dependent bone–muscle contact pressures and the injured area in the gluteus. We calculated the full-size (asymptotic) injured area in the gluteus and the time for injury onset for different sitting angles α( (90–150°), muscle tissue long-term shear moduli G (250–1,200 Pa) and bone diameters D (8–18 mm). We then evaluated the sensitivity of model results to variations in these parameters, in order to determine how injury predictions are affected. In reclined sitting (α = 150°) the full-size injured area was ∼2.1-fold smaller and the time for injury onset was ∼1.3-fold longer compared with erect sitting (α = 90°). For greater G the full-size injured area was smaller but the time for injury onset was shorter, e.g., increasing G from 250 to 1200 Pa decreased the full-size injured area ∼2.5-fold, but shortened the time for injury onset 6.2-fold. For smaller D the time for injury onset dropped, e.g., decreased ∼1.5-fold when D decreased from 18 to 8 mm. Interestingly, the full-size injured area maximized at D of about 12 mm but decreased for smaller or larger D. The susceptibility to sitting-acquired deep tissue injury strongly depends on the geometrical and biomechanical characteristics of the bone–muscle interface, and, particularly, on the radius of curvature of the IT which mostly influenced the size of the wound, and on the muscle stiffness which dominantly affected the time for injury onset.




Similar content being viewed by others
References
Agency for Health Care Policy and Research (AHCPR) (1994) Treatment of pressure ulcers. Clinical practice guideline no. 15. Publication no. 95-0652. US Department of Health and Human Services, Rockville
Ankrom MA, Bennett RG, Sprigle S, Langemo D, Black JM, Berlowitz DR, Lyder CH, National Pressure Ulcer Advisory Panel (2005) Pressure-related deep tissue injury under intact skin and the current pressure ulcer staging systems. Adv Skin Wound Care 18:35–42
Bansal C, Scott R, Stewart D, Cockerell CJ (2005) Decubitus ulcers: a review of the literature. Int J Dermatol 44:805–810
Barbenel J (1984) The prevalence of pressure sores. National symposium on the care, treatment, and prevention of decubitus ulcers. Conference proceedings, 1–9
Black JM (2005) National Pressure Ulcer Advisory Panel. Moving toward consensus on deep tissue injury and pressure ulcer staging. Adv Skin Wound Care 18:415–421
Bouten CV, Oomens CW, Baaijens FP, Bader DL (2003) The etiology of pressure ulcers: skin deep or muscle bound? Arch Phys Med Rehabil 84:616–619
Choi APC, Zheng YP (2005) Estimation of Young’s modulus and Poisson’s ratio of soft tissue from indentation using two different-sized indentors: finite element analysis of the finite deformation effect. Med Biol Eng Comput 43:258–264
Daniel RK, Priest DL, Wheatley DC (1981) Etiologic factors in pressure sores: an experimental model. Arch Phys Med Rehabil 62:492–498
Doughty D, Ramundom J, Bonham P, Beitz J, Erwin-Toth P, Anderson R, Rolstad BS (2006) Issues and challenges in staging of pressure ulcers. J Wound Ostomy Continence Nurs 33:125–130
Fischer-Cripps AC (1999) The Hertzian contact surface. J Mater Sci 34:129–137
Gefen A, Gefen N, Linder-Ganz E, Margulies SS (2005). In vivo muscle stiffening under bone compression promotes deep pressure sores. J Biomech Eng 127:512–524
Gennisson JL, Cornu C, Catheline S, Fink M, Portero P (2005) Human muscle hardness assessment during incremental isometric contraction using transient elastography. J Biomech 38: 1543–1550
Griffith BH (1963) Advances in the treatment of decubitus ulcers. Surg Clin North Am 43:245–260
Hess CT (2004) Care tips for chronic wounds: pressure ulcers. Adv Skin Wound Care 17:477–479
Kosiak M (1961) Etiology of decubitus ulcers. Arch Phys Med Rehabil 42:19–29
Lee EH, Radok JRM (1960) The contact problem for viscoelastic bodies. J Appl Mech 27E: 438–444
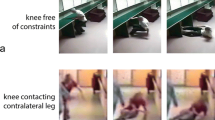
Linder-Ganz E, Gefen A (2004) Mechanical compression-induced pressure sores in rat hindlimb: muscle stiffness, histology, and computational models. J Appl Physiol 96:2034–2049
Linder-Ganz E, Engelberg S, Scheinowitz M, Gefen A (2006) Pressure-time cell death threshold for albino rat skeletal muscles as related to pressure sore biomechanics. J Biomech 39:2725–2732
Linder-Ganz E, Shabshin N, Itzchak Y, Gefen A (2007) Assessment of mechanical conditions in sub-dermal tissues during sitting: a combined experimental-MRI and finite element approach. J Biomech 40:1443–1454. doi:10.1016/j.jbiomech.2006.06.020
Meehan M (1994) National pressure ulcer prevalence survey. Adv Wound Care 7:27–37
Niezgoda JA, Mendez-Eastman S (2006) The effective management of pressure ulcers. Adv Skin Wound Care 19(Suppl):3–15
Palevski A, Glaich I, Portnoy S, Linder-Ganz E, Gefen A (2006) Stress relaxation of porcine gluteus muscle subjected to sudden transverse deformation as related to pressure sore modeling. J Biomech Eng 128:782–787
Salcido R (2006) What is the “purple heel”? Adv Skin Wound Care 19:11
Shea JD (1975) Pressure sores: classification and management. Clin Orthop 112:89–100
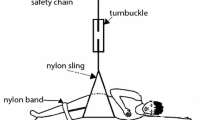
Stekelenburg A, Oomens CW, Strijkers GJ, de Graaf L, Bader DL, Nicolay K. (2006) A new MR-compatible loading device to study in vivo muscle damage development in rats due to compressive loading. Med Eng Phys 28:331–338
Stekelenburg A, Oomens CW, Strijkers GJ, Nicolay K, Bader DL (2006) Compression-induced deep tissue injury examined with magnetic resonance imaging and histology. J Appl Physiol 100: 1946–1954
Stockton L, Parker D (2002) Pressure relief behaviour and the prevention of pressure ulcers in wheelchair users in the community. J Tissue Viability 12:84–92
Thomas DR (2001) Prevention and treatment of pressure ulcers. What works? What doesn’t? Cleve Clin J Med 68:704–722
Vasconez LO, Schneider WJ, Jurkiewicz MJ (1977) Pressure sores. Curr Prob Surg 62:1–62
Winter DA (1990) Biomechanics and motor control of human movement, 2nd edn. Wiley, New York
Zheng M, Zheng YP, Mak AFT (1997) Estimating the effective Young’s modulus of soft tissues from indentation tests—nonlinear finite element analysis of effects of friction and large deformation. Med Eng Phys 19:512–517
Zheng Y, Mak AF, Lue B (1999) Objective assessment of limb tissue elasticity: development of a manual indentation procedure. J Rehabil Res Dev 36:71–85
Acknowledgments
My students Ms Ayelet Glass and Mr Eran Atlas are thanked for running the Matlab simulations. This study was partially supported by research grants from the Israeli Association for the Study of Diabetes, from the Chief Scientist’s Office of the Ministry of Health, Israel, and from the Nicholas and Elizabeth Slezak Super Center for Cardiac Research and Biomedical Engineering.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gefen, A. Risk factors for a pressure-related deep tissue injury: a theoretical model. Med Bio Eng Comput 45, 563–573 (2007). https://doi.org/10.1007/s11517-007-0187-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-007-0187-9