Abstract
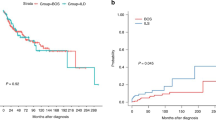
To explore the effect and pathogenssis of acute graft-versus-host disease (aGVHD) on early diffuse lung injury in allogeneic hematopoietic stem cell transplantation (allo-HSCT), we established an aGVHD model of C57BL/6→BALB/c mice. Chest computed tomography (CT) scans, histopathology and the levels of cytokines including tumor necrosis factor α (TNFα) and Interferon (IFNγ) in lungs were dynamically detected in recipient mice after transplantation. The incidence of aGVHD was respectively 0%, 0% and 100% in simple irradiation group (A), syngeneic transplant group(B) and allogeneic transplant group (C). Chest CT scans of recipient mice were normal in 3 groups on days +3 and +7 after transplantation. CT showed that two of ten mice had bilateral lung diffuse infiltrate on day +12 (on the brink of death) in group A and 6 of 10 mice had bilateral lung diffuse infiltrate on day +14 (3 d after aGVHD occurring) in group C, and were normal on days +12 and +14 in group B after transplantation. Histopathology of lungs in the 3 groups was similar, consisting of minor interstitial pneumonitis on day +3. Group A showed edema, hyperplasia of epithelial cells and widened alveolar interval on day +7, and epithelial cell necrosis, lymphocyte infiltration, hemorrhage, protein leakage, and local consolidation on day +12. The histopathology of group B showed slight edema of epithelial cells on +7 day, which were slighter than that on day +3, and virtually normal on day +14. The histopathology in group C was characterized by the significant expansion and congestion of capillaries, and lymphocyte infiltration on day +7, the acute pneumonitis was present involving tissue edema, lymphocyte and macrophage infiltration, protein leakage and perivascular inflammation on day +14. In group A, the levels of TNFα were lower on day +7 than on day +3. In group B, the levels of TNFα attained a peak on day +3, which decreased on days +7 and +14. In group C, the levels of TNFα were highest on day +7 and there was a significant difference between those on days +7 and +14 (P=0.816). In group A, the levels of IFNγ on day +7 were higher than on day +3. In group B, the levels of IFNγ increased progressively, but the comparison of IFNγ levels in different times had no statistical significance (P=0.521, 0.118, 0.340). In group C, the levels of IFNγ attained a peak by day +7 and decreased on day +14. aGVHD is the main cause of early non-infectious lung injury. T lymphocytes and TNFα are possibly implicated in the pathogenesis of acute GVHD-induced lung injury. The decreased levels of IFNγ in lung tissues following transplantation might be associated with pulmonary fibrosis in late non-infectious pulmonary complications.
Similar content being viewed by others
References
Yanik G, Cooke K R. The lung as a target organ of graft-versus-host disease. Semin Hematol, 2006, 43: 42–52, 10.1053/j.seminhematol.2005.09.004, 16412788
Afessa B, Peters S G. Noninfectious pneumonitis after blood and marrow transplant. Curr Opin Oncol, 2008, 20: 227–233, 10.1097/CCO.0b013e3282f50ff5, 18300774
Yoshihara S, Yanik G, Cooke K R, et al. Bronchiolitis obliterans syndrome( BOS), bronchiolitis obliterans organizing pneumonia(BOOP), and other late-onset noninfectious pulmonary complications following allogeneic hematopoieticstem cell transplantation. Biol Blood Marrow Transplant, 2007, 13: 749–759, 10.1016/j.bbmt.2007.05.001, 17580252
Afessa B, Litzow M R, Tefferi A, et al. Bronchiolitis obliterans and other late onset non-infeftious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplant, 2001, 28: 425–434, 10.1038/sj.bmt.1703142, 1:STN:280:DC%2BD3MrksFaquw%3D%3D, 11593314
Sakaida E, Nakaseko C, Harima A, et al. Late-onset noninfectious pulmonary complications after allogeneic stem cell transplantation are significantly associated with chronic graft-versus-host disease and with the graft-versus-leukemia effect. Blood, 2003, 102: 4236–4242, 10.1182/blood-2002-10-3289, 1:CAS:528:DC%2BD3sXpsFalsb8%3D, 12907447
Duncker C, Dohr D, Harsdorf S, et al. Non-infectious lung complications are closely associated with chronic graft-versus-host disease: a single center study of incidence, risk factors and outcome. Bone Marrow Transplant, 2000, 25: 1263–1268, 10.1038/sj.bmt.1702429, 1:STN:280:DC%2BD3cvgtFGktw%3D%3D, 10871731
Patriarca F, Skert C, Sperotto A, et al. Incidence, outcome, and risk factors of late-onset noninfectious pulmonary complications after unrelated donor stem cell transplantation. Bone Marrow Transplant, 2004, 33: 751–758, 10.1038/sj.bmt.1704426, 1:STN:280:DC%2BD2c7ktVenug%3D%3D, 14755316
Beschorner W E, Saral R, Hutchins G M, et al. Lymphocytic bronchitis associated with graft-versus-host disease in recipients of bone-marrow transplants. N Engl J Med, 1978, 299: 1030–1036, 1:STN:280:DyaE1M%2Fjt1Slsw%3D%3D, 30044, 10.1056/NEJM197811092991902
Cooke K R, Kobzik L, Martin T R, et al. An experimental model of idiopathic pneumonia syndrome after bone marrow transplantation: I. The roles of minor H antigens and endotoxin. Blood, 1996, 88: 3230–3239, 1:CAS:528:DyaK28XmtlWju7w%3D, 8963063
Cooke K R, Krenger W, Hill G, et al. Host reactive donor T Cells are associated with lung injury after experimental allogeneic bone marrow transplantation. Blood, 1998, 92: 2571–2580, 1:CAS:528:DyaK1cXmsVKnsb8%3D, 9746799
Hildebrandt G C, Oikiewicz K M, Corrion L A, et al. Donor-derived TNF-alpha regulates pulmonary chemokine expression and the developmeng of idiopathic pneumonia syndrome after allogeneic bone marrow transplantation. Blood, 2004, 104: 586–593, 10.1182/blood-2003-12-4259, 1:CAS:528:DC%2BD2cXlvFSmsL0%3D, 15069018
Ewing P, Miklos S, Olkiewicz K M, et al. Donor CD4+ T-cell pro duction of tumor necrosis factor alpha significantly contributes to the early proinflammatory events of graft-versus-host disease. Exp Hematol, 2007, 35: 155–163, 10.1016/j.exphem.2006.09.012, 1:CAS:528:DC%2BD2sXhsFKguw%3D%3D, 17198884
Bolanos-Meade J, Ioffe O, Hey J C, et al. Lymphocytic pneumonitis as the manifestation of acute graft-versus-host disease of the lung. Am J Hematol, 2005, 79: 132–135, 10.1002/ajh.20315, 15929116
Knox K S, Behnia M, Smith L R, et al. Acute graft-versus-host disease of the lung after liver transplantation. Liver Transpl, 2002, 8: 968–971, 10.1053/jlts.2002.35552, 12360443
Hakim F T, Mackall C L. The immune system: Effector and target of graft-versus-host disease. In: Ferrara J L M, Deeg H J, Burakoff S J eds. Graft-vs.-Host Disease Second Edition. New York: Marcel Dekker, Inc. 1997. 257
Hildebrandt G C, Olkiewicz K M, Corrion L, et al. A role for TNF receptor type II in leukocyte infiltration into the lung during experimental idiopathic pneumonia syndrome. Biol Blood Marrow Transplant, 2008, 14: 385–396, 10.1016/j.bbmt.2008.01.004, 1:CAS:528:DC%2BD1cXkslOrs74%3D, 18342780
Laster S M, Wood J G, Gooding L R. Tumor necrosis factor can induce both apoptic and necrotic forms of cell lysis. J Immunol. 1988, 141: 2629–2634, 1:CAS:528:DyaL1cXmtV2ntrs%3D, 3171180
Reddy P. Pathophysiology of acute graft-versus-host disease. Hematol Oncol, 2003, 21: 149–161, 10.1002/hon.716, 14735553
Shankar G, Cohen D A. Idiopathic pneumonia syndrome after bone marrow transplantation: The role of pre-transplant radiation conditioning and local cytokine dysregulation in promoting lung inflammation and fibrosis. Int J Exp Pathol, 2001, 82: 101–113, 10.1111/j.1365-2613.2001.iep182.x, 1:CAS:528:DC%2BD3MXmtVymu7g%3D, 11454101
Hildebrandt G C, Corrion L A, Olkiewicz K M, et al. Blockade of CXCR3 receptor: ligand interactions reduces leukocyte recruitment to the lung and the severity of experimental idiopathic pneumonia syndrome. J Immunol, 2004, 173: 2050–2059, 1:CAS:528:DC%2BD2cXlvVajt7o%3D, 15265940
Refaeli Y, Van Parijs L, Alexander S I, et al. Interferon-gamma is required for activation induced death of T lymphocytes. J Exp Med, 2002, 196: 999–1005, 10.1084/jem.20020666, 1:CAS:528:DC%2BD38Xnsl2rtb0%3D, 12370261
Badovinac V P, Tvinnereim A R, Harty J T. Regulation of antigen-specific CD8(+) T cell homeostasis by perforin and interferon-gamma. Science, 2000, 290: 1354–1358, 10.1126/science.290.5495.1354, 1:CAS:528:DC%2BD3cXotlemu74%3D, 11082062
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the National Natural Science Foundation of China (Grant No. 30971300)
Rights and permissions
About this article
Cite this article
Ning, J., Liu, Q.F., Luo, X.D. et al. Effect and mechanism of acute graft versus host disease on early diffuse murine lung injury following allogeneic stem cell transplantation. SCI CHINA SER C 52, 1016–1022 (2009). https://doi.org/10.1007/s11427-009-0139-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11427-009-0139-8