Abstract
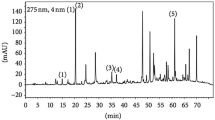
Sepsis remains the leading cause of death in intensive care units. Uncontrolled systemic inflammation and an impaired protein C pathway are two important contributors to sepsis pathophysiology. Based on the beneficial effects of the saponin fraction from Astragalus membranaceus roots (SAM) against inflammation, liver dysfunction, and endothelium injury, we investigated the potential protective roles and underlying mechanisms of SAM on polymicrobial sepsis induced by cecal ligation and puncture (CLP) in mice. SAM, orally administered 1 h before and after CLP, significantly elevated the survival rate of mice. At 96 h after CLP operation, all mice in the model group died, whereas 33.3% of mice in the SAM (400 mg/kg)-treated group survived. SAM attenuated both inflammatory factors and their abilities to induce tissue dysfunction, which was mainly evidenced by decreased infiltration of polymorphonuclear leukocytes, tissue edema, and lung wet-to-dry weight ratio, lowered levels of myeloperoxidase (MPO), nitric oxide (NO), lactate dehydrogenase (LDH), alanine aminotransferase (ALT), and aspartate aminotransferase (AST) in serum, as well as downregulated expressions of iNOS and IL-1β mRNA in livers. Furthermore, we addressed the effects of SAM on the protein C (PC) pathway, closely linked with sepsis. In CLP-induced septic mice, SAM elevated the impaired expression of PC mRNA in livers. In vitro, SAM reversed the decreased expressions of thrombomodulin (TM) and endothelial PC receptor (EPCR) mRNA induced by lipopolysaccharide (LPS) in endothelial cells. These findings suggest that SAM is able to restore the impaired protein C pathway. Taken together, the current study demonstrates that SAM has protective effects on polymicrobial sepsis in mice. The mechanisms of action involve anti-inflammation and upregulation of the PC pathway.







Similar content being viewed by others
References
Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through 2000. Engl J Med 348:1546–1554
Seam N, Suffredini AF (2007) Mechanisms of sepsis and insights from clinical trials. Drug Discov Today Dis Mech 4:83–93
Aird WC (2003) The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood 101:3765–3777
Esmon CT (2005) The interactions between inflammation and coagulation. Br J Haemat 131:417–430
Daniel G, Remick MD (2007) Pathophysiology of sepsis. Am J Pathol 170:1435–1444
Dhainaut JF, Marin N, Mignon A, Vinsonneau C (2001) Hepatic response to sepsis: interaction between coagulation and inflammatory processes. Critical Care Med 29:S42–S47
Yan SB, Helterbrand JD, Hartman DL, Wright TJ, Bernard GR (2001) Low levels of protein C are associated with poor outcome in severe sepsis. Chest 120:915–922
Esmon CT (2003) The protein C pathway. Chest 124:S26–S32
Eichacker PQ, Natanson C (2007) Increasing evidence that the risks of rhAPC may outweigh its benefits. Intensive Care Med 33:396–399
Jin R, Kurashige S (1996) Effect of shi-ka-ron on cytokine production of lymphocytes in mice treated with cyclophosphamide. Am J Chinese Med 24:37–44
Li HB, Ge YK, Zhang L, Zheng XX (2006) Astragaloside IV improved barrier dysfunction induced by acute high glucose in human umbilical vein endothelial cells. Life Sci 79:1186–1193
Cui R, He J, Wang B, Zhang F, Chen G, Yin S, Shen H (2003) Suppressive effect of Astragalus membranaceus Bunge on chemical hepatocarcinogenesis in rats. Cancer Chemother Pharmacol 51:75–80
Minsook R, Eun HK, Mison C (2008) Astragali Radix elicits anti-inflammation via activation of MKP-1, concomitant with attenuation of p38 and Erk. J Ethnopharm 115:184–193
Zhang WJ, Hufnagl P, Binder BR, Wojta J (2003) Antiinflammatory activity of astragaloside IV is mediated by inhibition of NF-κB activation and adhesion molecule expression. Thromb Haemost 90:904–914
Wichterman KA, Baue AE, Chaudry IH (1980) Sepsis and septic shock—a review of laboratory models and a proposal. J Surg Res 29:189–201
Ma XQ, Shi Q, Duan JA, Dong TTX, Tsim KWK (2002) Chemical analysis of Radix Astragali (Huangqi) in China: a comparison with its adulterants and seasonal variations. J Agric Food Chem 50:4861–4866
Huang CR, Wang GJ, Li H, Xie HT, Sun JG, Lv H, Lv T (2006) Sensitive and selective liquid chromatography–electrospray ionization–mass spectrometry analysis of astragaloside-IV in rat plasma. J Pharm Biomed Anal 40:788–793
Wang SG, Li JY, Huang H, Gao W, Zhuang CL, Li B, Zhou P, Kong DY (2009) Anti-hepatitis B virus activities of astragaloside IV isolated from Radix Astragali. Biol Pharm Bull 32:132–135
Xu XX, Zhang R, Xia LZ (2008) Effects of three saponin extracting methods on content of astragaloside IV. Chin J Vet Drug 42:12–14
Yang J, Dai Y, Xia YF (2009) Alpinia katsumadai Hayata prevents mouse sepsis induced by cecal ligation and puncture through promoting bacterial clearance and downregulating systemic inflammation. Phytother Res 23:267–273
Hotchkiss KA, Ashton AW, Mahmood R, Russell RG, Sparano JA, Schwartz EL (2002) Inhibition of endothelial cell function in vitro and angiogenesis in vivo by docetaxel (Taxotere): association with impaired repositioning of the microtubule organizing center. Mol Cancer Ther 1:1191–1200
Deitch EA (1998) Animal models of sepsis and shock: a review and lessons learned. Shock 9:1–11
Bochud PY, Calandra T (2003) Pathogenesis of sepsis: new concepts and implications for future treatment. BMJ 326:262–266
Vincent JL, Zhang H, Szabo C, Preiser JC (2000) Effects of nitric oxide in septic shock. Am J Respir Crit Care Med 161:1781–1785
Bultinck J, Sips P, Vakaet L, Brouckaert P, Cauwels A (2006) Systemic NO production during (septic) shock depends on parenchymal and not on hematopoietic cells: in vivo iNOS expression pattern in (septic) shock. FASEB J 20:2363–2365
Pinsky MR, Vincent JL, Deviere J, Alegre M, Kahn RJ, Dupont E (1993) Serum cytokine levels in human spetic shock: relation to multiple system organ failure and mortality. Chest 103:562–575
Fisher CJ, Yan SB (2000) Protein C levels as a prognostic indicator of outcome in sepsis and related diseases. Crit Care Med 28:S49
Mesters RM, Helterbrand J, Utterback BG, Yan B, Chao YB, Fernandez JA, Griffin JH, Hartman DL (2000) Prognostic value of protein C concentrations in neutropenic patients at high risk of severe septic complications. Crit Care Med 28:2209
Esmon CT (2003) The protein C pathway. Chest 124:26S–32S
Dahlback B, Villoutreix BO (2005) The anticoagulant protein C pathway. FEBS Lett 579:3310–3316
Joyce DE, Grinnell BW (2002) Recombinant human activated protein C attenuates the inflammatory response in endothelium and monocytes by modulating nuclear factor-kappaB. Crit Care Med 30:S288–S293
Joyce DE, Gelbert L, Ciaccia A, DeHoff B, Grinnell BW (2001) Gene expression profile of antithrombotic protein C defines new mechanisms modulating inflammation and apoptosis. J Biol Chem 276:11199–11203
Riewald M, Petrovan R, Donner A, Mueller BM, Ruf W (2002) Activation of endothelial cell protease activated receptor 1 by the protein C pathway. Science 296:1880–1882
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 30600821), the Natural Science Foundation of Anhui Province (No. 050431004), the postgraduate innovation project of Jiangsu Province.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gao, Xh., Xu, Xx., Pan, R. et al. Saponin fraction from Astragalus membranaceus roots protects mice against polymicrobial sepsis induced by cecal ligation and puncture by inhibiting inflammation and upregulating protein C pathway. J Nat Med 63, 421–429 (2009). https://doi.org/10.1007/s11418-009-0348-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-009-0348-2