Abstract
The study aims to investigate associations between cardiovascular health (CVH) metrics and retinal ageing indexed by retinal age gap. A total of 26,354 participants from the UK Biobank study with available CVH metrics and qualified retinal imaging were included in the present analysis. CVH included 7 metrics (smoking, physical activity, diet, body mass index [BMI], total cholesterol, blood pressure [BP], blood glucose). These were summarized to classify the overall CVH as poor (0–7), intermediate (8–10) or ideal (11–14). Retinal age gap was defined as the difference between biological age predicted by fundus images and chronological age. Accelerated and non-accelerated retinal ageing was defined if retinal age gap was in the upper or lower 50% quantiles of the study population, respectively. Linear and logistic regression models estimated the association of overall CVH and each metric of CVH with retinal age gap respectively. Our results showed that in the fully adjusted model, each one-unit score increase in overall CVH was negatively associated with retinal age gap (odds ratio [OR] = 0.89, 95% confidence interval [CI]: 0.87-0.92, P < 0.001). Compared with poor overall CVH, people with intermediate and ideal overall CVH had significantly lower retinal age gap (OR = 0.76, 95%CI: 0.67–0.85, P < 0.001; OR = 0.58, 95%CI: 0.50–0.67, P < 0.001). Similar associations were found between overall CVH and accelerated retinal ageing. CVH metrics including smoking, BMI, BP, and blood glucose were also significantly associated with higher retinal age gap. Taken together, we found a significant and inverse dose-response association between CVH metrics and retinal age gap, indicating that maintaining healthy metrics especially smoking, BMI, BP, and blood glucose may be crucial to slow down biological ageing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ageing has become an urgent problem worldwide, with the proportion of people over 60 years projected to rise from 12 to 20% between 2015 and 2050. This is expected to inflate rates of morbidity and mortality worldwide [1]. Heterogeneous ageing pace has been noted in various population, which leads to different health outcomes among same age populations [2]. This highlights the need for accurately quantifying ageing process.
Vascular ageing is an important paradigm of the ageing process which contributes to the development of cardiovascular diseases (CVD) which precipitate morbidity and mortality [3, 4]. The retina uniquely visualizes the microvasculature of the body and acts as a representative window of the microcirculation [5]. Our research group previously leveraged deep learning (DL) to accurately predict chronological age based on retinal fundus images in a healthy population [6]. We verified the retinal age gap, defined as the difference between retina-predicted age and chronological age, could independently predict mortality and age-related diseases [7,8,9,10] . We also found retinal age gap was significantly associated with arterial stiffness index and future risk of cardiovascular events [
Identifying variables which influence the rate of vascular ageing is important for public health campaigns and population modelling. Cardiovascular health (CVH) is a concept introduced by the American Heart Association (AHA) in 2010 to bring about awareness and attention to the effects of CVD. Overall CVH can be classified as poor (scores 0–7), intermediate (8–10), and ideal (11–14) based on smoking, physical activity, diet, body mass index (BMI), total cholesterol, blood pressure (BP), and blood glucose. Each metric is also classified as poor, intermediate, and ideal [11]. Previously, ideal overall CVH has been associated with a lower risk of cardiovascular events and CVD-related mortality [12, 13]. Therefore, these variables are considered modifiable risk factors for CVH which may assist the prevention of vascular ageing.
To the best of our knowledge, few studies have explored associations between CVH metrics and retinal ageing. Establishing an association between these may provide an opportunity for population-based retinal screening to identify individuals at-risk of accelerated ageing, and implement strategies which inhibit the precipitation of further vascular dysfunction. Therefore, we aimed to investigate the association of CVH metrics with retinal age gap, the reliable biomarker of vascular ageing, in a large-scale, population-based cohort.
Methods
Study design and population
This study retrieved data from the UK Biobank study, a large, prospective, population-based cohort study comprising over 500,000 adults aged 40–69 years enrolled between 2006 and 2010. Study design and protocols have been described elsewhere [14], but in brief, baseline assessments including questionnaires and physical measurements were completed at 22 assessment centers across England, Scotland, and Wales. Biological samples of blood, urine, and saliva were also collected. Information about medical events were identified through hospital admission records and death registers.
The UK Biobank was reviewed and approved by the National Information Governance Board for Health and Social Care and the National Health Service North West Multicenter Research Ethics Committee (11/NW/0382). Data used in the present study was accessed through the Biobank consortium (Application No: 62489). Since this is a publicly identified dataset, the Guangdong Provincial People’s Medical Research Ethics Committee waived the ethical requirement. This study was carried out in accordance with the Helsinki declaration, and informed consent was provided from all participants.
Measurement and definition of CVH
According to AHA guidelines, overall CVH is based on 7 behavioral and biological metrics, including smoking, physical activity, diet, BMI, total cholesterol, BP, and blood glucose. Each metric was categorized as poor (scored as 0), intermediate (scored as 1), and ideal (scored as 2) according to the modified AHA criteria (Supplemental Table 1). We summarized the seven metrics as a CVH score ranging from 0 to 14. The overall CVH was divided into poor (0–7), intermediate (8–10), and ideal (11–14) with higher scores corresponding to better CVH.
For smoking status, current smokers were assigned to poor, past smokers to intermediate, and ideal as never having smoked. Status of physical activity was defined as poor if physical activity was <3 metabolic equivalent tasks (MET) min/week, intermediate if activity was 3–449 MET min/week, and ideal if activity was >450 MET min/week consistent to previous studies [11, 15]. For diet, poor status was defined as <1 portion per day of fresh fruit, raw vegetables, cooked fruit/vegetables, and <2 portions per week of fish; intermediate status was defined as >1 portion per day of fresh fruit, raw vegetables, cooked fruit/vegetables, or >2 portions per week of fish; ideal health was defined as >1 portion per day of each of fresh fruit, raw vegetables, cooked fruit/vegetables, and >2 portions per week of fish [16]. Body mass index was calculated as the weight of an individual in kilograms divided by their height in meters squared. Poor status was defined as BMI >30 kg/m [2]; intermediate status was defined as BMI 25–29.9 kg/m [2]; ideal health was defined as BMI <25 kg/m [2]. For total cholesterol, poor status was defined as cholesterol >6.21 mmol/L (240 mg/dL); intermediate status was defined as cholesterol 5.18–6.18 mmol/L (200–239 mg/dL), or treated cholesterol <5.18 mmol/L (200 mg/dL); ideal status was defined as untreated and <5.18 mmol/L. Blood pressure was classified as poor (BP >140/90 mmHg), intermediate (systolic BP 120-139 mmHg or diastolic BP 80–89 mmHg or treated BP <120/80 mmHg), and ideal (untreated BP <120/80 mmHg), respectively. For blood glucose, ideal health was defined as untreated fasting plasma glucose (FPG) <100 mg/dL, intermediate health as treated FPG <100 mg/dL or FPG 100–125 mg/dL, and poor health was defined as ≥126 mg/dL.
Fundus images
Paired retinal fundus and optical coherence tomography imaging (Topcon 3D OCT 1000 Mk2, Topcon Corp, Tokyo, Japan) data were collected. A 45-degree non-mydriatic and non-stereo fundus image centered on the macular and including the optic disc was taken for each eye. The quality check process was based on a previously developed algorithm [17]. The ground truth was the manual three-level grading system labelled by two ophthalmologists (good, usable, and reject). Fundus images with good or usable quality was considered to pass the quality check. In the baseline examination from the UK Biobank study, 80,169 images of 46,969 participants from the total obtained 131,238 images of 66,500 participants passed the image quality check.
Deep learning model for age prediction
Details on the development and validation of the DL model have been described in detail elsewhere [6]. Briefly, a total of 19,200 retinal fundus images from 11,052 healthy participants trained and validated the DL model for chronological age prediction. If available, images from both eyes were used to maximize data volume. Mean absolute error (MAE) and correlation coefficients between retina-predicted age and chronological age assessed DL model performance in the testing dataset. The retinal age predicted by the DL model accurately quantified chronological age with a correlation coefficient of 0.80 (P < 0.001) and MAE of 3.55 years.
Retinal age gap
Retinal age gap was defined as the difference between the retinal age, derived from fundus images, and the chronological age. We then transformed the retinal age gap to a binary variable where the upper 50% quantile was considered to be accelerated retinal ageing, and the lower 50% quantile was considered to be non-accelerated retinal ageing.
Covariates
Covariates in the present study included age (continuous, years), sex (male/female), ethnicity (white/others), Townsend Deprivation Index (continuous), education attainment (college or university degree/others), C-reactive protein (continuous, mg/dL), consumption of alcohol intaking status (never or ex/current drinker), history of CVD (yes/no), and diabetes (yes/no). History of CVD was determined via data linkage to hospital admission and death registry records according to the International Classification of Diseases edition 10 (ICD-10) and the International Classification of Diseases edition 9 (ICD-9). Participants with any records of self-reported or doctor-diagnosed diabetes, history of taking anti-hyperglycemic medications, use of insulin, or HbA1C ≥48 mmol/L were considered to have diabetes mellitus.
Statistical analysis
We summarized baseline characteristics by overall CVH and retinal ageing using descriptive statistics. We reported mean and standard deviation (SD) for continuous variables or numbers and proportions for categorical variables, respectively. We compared the baseline characteristics by overall CVH using chi-square test for categorical or one-way ANOVA for continuous variables. Age, sex, and ethnicity-adjusted logistic regression models estimated odds ratio (OR) and 95% confidence interval (CI) to determine baseline characteristics that were significantly associated with retinal ageing. Covariates significantly associated with overall CVH and/or retinal age gap were added into final regression models to calculate OR. We used linear regression and logistic regression models to investigate the association between overall CVH (independent variable) and retinal age gap. Model I adjusted for age, sex, and ethnicity; Model II additionally adjusted for educational attainment, socioeconomic status and alcohol intake, C-reactive protein (CRP), history of CVD, and diabetes. We also performed analysis to investigate the associations between each CVH metric and retinal age gap. Odds ratio with their 95% CI were reported. A two-sided P-value of <0.05 indicated statistical significance. All analyses were performed using Stata (version 13, StataCorp, Texas, USA).
Results
Study sample
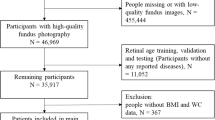
After excluding participants whose fundus images were used for age prediction model training and validation (N = 11,052), and those without sufficient CVH data (N = 9,563), 26,354 participants (mean age 56.5 ± 8.07 years, 53.7% females) were included in the final analysis. Fundus images of the right eye estimated retinal age gap, and images of the left eye were used if images of the right eye were not available. Figure 1 shows the flow chart distribution of study population numbers. Table 1 depicts the baseline characteristics of participants stratified by overall CVH. Populations with ideal overall CVH tended to be younger, female, with better socioeconomic status, of white ethnicity, higher education level, no history of drinking alcohol, lower CRP, and no history of diabetes or CVD (P < 0.05).
Baseline characteristics associated with retinal ageing
Table 2 shows the baseline characteristics of participants stratified by classification of accelerated or non-accelerated retinal ageing. After adjusting for age, sex, and ethnicity, only socioeconomic status (OR = 1.02; 95%CI: 1.01–1.03), CRP (OR = 1.02; 95%CI: 1.01–1.02), and history of diabetes (OR = 1.58; 95%CI:1.40–1.78) were significantly associated with accelerated retinal ageing (P < 0.05).
Overall CVH and retinal age gap
After adjusting for age, gender, and ethnicity, each one-unit score increases in overall CVH was independently associated with a 13% decrease in retinal age gap (OR = 0.87, 95% CI: 0.85–0.90, P < 0.001) (Table 3). This finding remained significant after adjusted for further confounders (OR = 0.89, 95% CI: 0.87–0.92, P < 0.001). Participants with an intermediate and ideal overall CVH had significantly lower retinal age gap compared to those with a poor overall CVH (OR = 0.76, 95%CI: 0.67–0.85, P < 0.001; OR = 0.58, 95%CI: 0.50–0.67, P < 0.001; respectively). The trend between overall CVH and retinal age gap was significant (P < 0.001).
Similar associations were identified for participants with accelerated retinal ageing, as shown in Table 4. The age, sex, and ethnicity-adjusted model showed that each one-unit increase of overall CVH was associated with a lower risk of having an accelerated retinal ageing (OR = 0.93, 95%CI: 0.92–0.95, P < 0.001). Participants with an intermediate and ideal overall CVH had a significantly reduced risk of accelerated retinal age compared to those with a poor overall CVH (OR = 0.79, 95%CI: 0.73–0.85, P < 0.001; OR = 0.72, 95%CI: 0.66–0.79, P < 0.001; respectively). The associations remained significant in the fully adjusted model (OR = 0.83, 95%CI: 0.77–0.90, P < 0.001; OR = 0.78, 95%CI: 0.71–0.86, P < 0.001; respectively).
CVH components and their risk with retinal ageing
The seven components which make up overall CVH were individually analyzed for their association with the retinal age gap as continuous (retinal age gap) and categorical outcomes (accelerated or non-accelerated retinal ageing) as shown in Supplementary Table 2. Compared with the poor status, ideal status of four components significantly associated with lower retinal age gap included smoking (OR = 0.73, 95%CI: 0.62–0.87), BMI (OR = 0.80, 95%CI: 0.71–0.91), BP (OR = 0.77, 95%CI: 0.66–0.89), and blood glucose (OR = 0.66, 95%CI: 0.55–0.80) (all P < 0.001). Similar associations were identified between ideal status of smoking (OR = 0.80, 95%CI: 0.72–0.90, P < 0.001), BMI (OR = 0.90, 95%CI: 0.82–0.97, P = 0.010), BP (OR = 0.88, 95%CI: 0.80–0.96, P = 0.007), and blood glucose (OR = 0.85, 95%CI: 0.75–0.95, P = 0.006) and accelerated retinal ageing.
Discussion
Using the UK Biobank data, we firstly reported a significant and inverse dose-response association between CVH metrics and retinal age gap. Additionally, better CVH was associated with a lower risk of accelerated retinal ageing, and smoking, BMI, BP, and blood glucose also had significant independent associations with retinal ageing. These findings highlight the potential for retinal age gap to be used as a surrogate biomarker of vascular ageing.
Our study provides novel insights into the association between CVH metrics and currently established vascular ageing biomarkers. Several previous studies have demonstrated CVH is negatively associated with vascular biomarkers including arterial stiffness [18,19,20], intracranial carotid artery stenosis [21], carotid intima-media thickness [22], and carotid plaque [23, 24]. However, these studies concentrate on macrovascular dysfunction. Considering microvascular dysfunction precedes macrovascular pathology in response to cardiovascular risk factors [25,26,27] and retinal age is a direct output of the retinal microvasculature, our research suggests retinal age gap is likely more sensitive at tracking vascular changes allowing for earlier detection of vascular dysfunction.
Our study reveals retinal age gap could be a fast and cost-effective method to screen for premature vascular ageing in a population-based manner. In the past, poorer CVH and cardiovascular events have repeatedly been significantly associated with wider retinal venules and narrower retinal arterioles [28]. A multicenter study has demonstrated positive association between ideal CVH and retinal microvasculature measured by vessel diameters, lengths, length diameter ratio, and tortuosity [29]. Although automated segmentation exists, the interpretation of these vasculature still requires unrealistic levels of manual work. Such pitfalls inhibit the fundus images from being used widely, which highlights the advantage of retinal age as a simple and accessible solution [30].
CVH metrics including smoking, BMI, BP, and blood glucose all demonstrated significant associations with retinal ageing. Several underlying pathophysiological mechanisms may explain the associations between CVH metrics and retinal ageing. Smoking may cause microvascular dysfunction through reducing nitrogen oxide (NO) bioavailability, activation of inflammatory cascades, and tissue remodeling [31, 32]. These contribute to retinal arteriolar constriction and venular dilation [33]. Overnutrition and obesity status measured by BMI are thought to induce arteriolar and venular changes via the presence of adipokines, vasoconstrictor molecules, and decreased NO [33,34,35,36], and hypertensive states may cause vasospasm and ischemia, leading to chronic auto-regulatory vascular dysfunction and arteriosclerotic change [33, 37, 38]. Lastly, chronic hyperglycemia would trigger the activation of protein kinase C and advanced glycation end products, causing abnormal leukocyte-endothelial interactions and ultimately vascular damage in the retina [39,40,41,42]. Therefore, our findings are aligned with the current literature, which suggests retinal age gap could be a reliable indicator of vascular changes.
Our findings have several important clinical implications. First, our study explored the association between retinal age gap, a biomarker of biological age, with CVH metrics, and identified modifiable CVH metrics including smoking, BMI, BP, and blood glucose that may accelerate ageing. This highlights the promising potential of biological age for ageing research revolution and healthy ageing promotion [43]. Given the modifiable nature of CVH components, our findings emphasize the benefits of healthy lifestyles and interventions on ageing process. Second, the fast and cost-effective nature of retinal age makes it easy to implement in large-scale populations, which enables dynamic tracking and monitoring across time. This allows for the participants to have the opportunity of multiple scans, thereby facilitating individualized and real-time feedback for their proactive actions. Taken together, retinal age can be used as an accessible biological age biomarker to inform individuals about their ageing risks and important benefits of interventions for vascular health, thus reducing the overall burden of cardiovascular disease.
Strengths and limitations
Strengths of the present study included its relatively large sample size, standardized protocol for data collection, and comprehensive adjustment of confounding factors. Despite this, some limitations should be acknowledged. Firstly, the cross-sectional nature of our study cannot infer causal relationship between CVH metrics and retinal age gap which may limit the reliability of these results to real-life circumstances. Secondly, the UK Biobank study enrolled mainly healthy and young participants which, given the geographical location, were more likely to be white ethnicity and of higher socioeconomic status. This may affect the generalizability of our results to more diverse populations [44]. However, the association between CVH metrics and retinal age gap would not be affected by the representativeness of the sample [44, 45]. Third, among the components which made up CVH, factors including physical activity and diet were subjectively measured by self-reported questionnaires, which would be subject to recall bias This may partly explain the lack of significant associations of physical activity and diet with retinal age gap in our component analyses. Finally, we were unable to fully exclude the possibility of residual confounders.
Conclusion
In conclusion, our findings suggested a significant and inverse dose-response association between CVH metrics and retinal age gap. Maintaining health behaviors especially no smoking, good BMI, BP, and blood glucose may be crucial to reduce risk of retinal ageing. Further studies are needed to validate our findings.
References
World Health Organization. World report on ageing and health: World Health Organization; 2015.
Lowsky DJ, Olshansky SJ, Bhattacharya J, Goldman DP. Heterogeneity in healthy aging. J Gerontol A Biol Sci Med Sci. 2014;69(6):640–9.
Izzo C, Carrizzo A, Alfano A, Virtuoso N, Capunzo M, Calabrese M, De Simone E, Sciarretta S, Frati G, Oliveti M, Damato A, Ambrosio M, De Caro F, Remondelli P, Vecchione C. The impact of aging on cardio and cerebrovascular diseases. Int J Mol Sci. 2018;19(2):481.
Ghebre YT, Yakubov E, Wong WT, Krishnamurthy P, Sayed N, Sikora AG, Bonnen MD. Vascular aging: implications for cardiovascular disease and therapy. Transl Med (Sunnyvale). 2016;6(4):183.
Liew G, Wang JJ, Mitchell P, Wong TY. Retinal vascular imaging: a new tool in microvascular disease research. Circ Cardiovasc Imaging. 2008;1(2):156–61.
Zhu Z, Shi D, Guankai P, Tan Z, Shang X, Hu W, Liao H, Zhang X, Huang Y, Yu H, Meng W, Wang W, Ge Z, Yang X, He M. Retinal age gap as a predictive biomarker for mortality risk. Br J Ophthalmol. 2022.
Hu W, Wang W, Wang Y, Chen Y, Shang X, Liao H, Huang Y, Bulloch G, Zhang S, Kiburg K, Zhang X, Tang S, Yu H, Yang X, He M, Zhu Z. Retinal age gap as a predictive biomarker of future risk of Parkinson's disease. Age Ageing 2022;51(3):afac062
Zhu Z, Hu W, Chen R, Xiong R, Wang W, Shang X, Chen Y, Kiburg K, Shi D, He S, Huang Y, Zhang X, Tang S, Zeng J, Yu H, Yang X, He M. Retinal age gap as a predictive biomarker of stroke risk. BMC Med. 2022;20(1):466.
Zhang S, Chen R, Wang Y, Hu W, Kiburg KV, Zhang J, Yang X, Yu H, He M, Wang W, Zhu Z. Association of retinal age gap and risk of kidney failure: A UK biobank study. Am J Kidney Dis. 2022;S0272–6386(22):01047–2.
Zhu Z, Chen Y, Wang W, Wang Y, Hu W, Shang X, Liao H, Shi D, Huang Y, Ha J, Tan Z, Kiburg KV, Zhang X, Tang S, Yu H, Yang X, He M. Association of retinal age gap with arterial stiffness and incident cardiovascular disease. Stroke. 2022;53(11):3320–8.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613.
Bundy JD, Ning H, Zhong VW, Paluch AE, Lloyd-Jones DM, Wilkins JT, Allen NB. Cardiovascular health score and lifetime risk of cardiovascular disease: the cardiovascular lifetime risk pooling project. Circ Cardiovasc Qual Outcomes. 2020; Circoutcomes119006450.
Younus A, Aneni EC, Spatz ES, Osondu CU, Roberson L, Ogunmoroti O, Malik R, Ali SS, Aziz M, Feldman T, Virani SS, Maziak W, Agatston AS, Veledar E, Nasir K. A systematic review of the prevalence and outcomes of ideal cardiovascular health in US and non-US populations. Mayo Clin Proc. 2016;91(5):649–70.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779.
Joseph JJ, Echouffo-Tcheugui JB, Carnethon MR, Bertoni AG, Shay CM, Ahmed HM, Blumenthal RS, Cushman M, Golden SH. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Diabetologia. 2016;59(9):1893–903.
Xu C, Zhang P, Cao Z. Cardiovascular health and healthy longevity in people with and without cardiometabolic disease: A prospective cohort study. E Clin Med. 2022;45:101329.
Fu H, et al. Evaluation of retinal image quality assessment networks in different color-spaces. et al. In: Medical Image Computing and Computer Assisted Intervention – MICCAI 2019. MICCAI 2019. Lecture Notes in Computer Science(), vol 11764. Cham: Springer; 2019. https://doi.org/10.1007/978-3-030-32239-7_6.
Zheng X, Zhang R, Liu X, Zhao H, Liu H, Gao J, Wu Y, Wu S. Association between cumulative exposure to ideal cardiovascular health and arterial stiffness. Atherosclerosis. 2017;260:56–62.
Sang Y, Mao K, Cao M, Wu X, Ruan L, Zhang C. Longitudinal association between cardiovascular health and arterial stiffness in the Chinese adult population. J Int Med Res. 2021;49(3):300060521998889.
Wang A, Tian X, Zuo Y, Chen S, Wu S, Wang Y. Mediation effect of arterial stiffness on ideal cardiovascular health and stroke. Nutr Metab Cardiovasc Dis. 2021;31(8):2382–90.
Zhang Q, Zhang S, Wang C, Gao X, Zhou Y, Zhou H, Wang A, Wu J, Bian L, Wu S, Zhao X. Ideal cardiovascular health metrics on the prevalence of asymptomatic intracranial artery stenosis: a cross-sectional study. PLoS One. 2013;8(3):e58923.
Shpilsky D, Bambs C, Kip K, Patel S, Aiyer A, Olafiranye O, Reis SE, Erqou S. Association between ideal cardiovascular health and markers of subclinical cardiovascular disease. Clin Cardiol. 2018;41(12):1593–9.
Sturlaugsdottir R, Aspelund T, Bjornsdottir G, Sigurdsson S, Eiriksdottir G, Imai CM, Garcia M, Launer LJ, Harris TB, Gudnason V. Carotid atherosclerosis and cardiovascular health metrics in old subjects from the AGES-Reykjavik study. Atherosclerosis. 2015;242(1):65–70.
Guo L, Cheng L, He W, Ju Y, Zhao X. Ideal cardiovascular health and incidence of carotid plaque among middle-aged and elderly adults. J Stroke Cerebrovasc Dis. 2018;27(2):391–6.
Bordy R, Totoson P, Prati C, Marie C, Wendling D, Demougeot C. Microvascular endothelial dysfunction in rheumatoid arthritis. Nat Rev Rheumatol. 2018;14(7):404–20.
Padro T, Manfrini O, Bugiardini R, Canty J, Cenko E, De Luca G, Duncker DJ, Eringa EC, Koller A, Tousoulis D, Trifunovic D, Vavlukis M, de Wit C, Badimon L. ESC Working Group on Coronary Pathophysiology and Microcirculation position paper on 'coronary microvascular dysfunction in cardiovascular disease'. Cardiovasc Res. 2020;116(4):741–55.
D'Agata MN, Hoopes EK, Berube FR, Hirt AE, Witman MA. Young black women demonstrate impaired microvascular but preserved macrovascular function compared to white women. Exp Physiol. 2021;106(10):2031–7.
Ogagarue ER, Lutsey PL, Klein R, Klein BE, Folsom AR. Association of ideal cardiovascular health metrics and retinal microvascular findings: the Atherosclerosis Risk in Communities Study. J Am Heart Assoc. 2013;2(6):e000430.
Campbell MD, Laitinen TT, Hughes A, Pahkala K, Juonala M, Kähönen M, Wong TY, Lehtimäki T, Hutri-Kähönen N, Raitakari OT, Tapp RJ. Impact of ideal cardiovascular health in childhood on the retinal microvasculature in midadulthood: cardiovascular risk in young Finns study. J Am Heart Assoc. 2018;7(20):e009487.
Strain WD, Adingupu DD, Shore AC. Microcirculation on a large scale: techniques, tactics and relevance of studying the microcirculation in larger population samples. Microcirculation. 2012;19(1):37–46.
Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004;43(10):1731–7.
Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34(3):509–15.
Sun C, Wang JJ, Mackey DA, Wong TY. Retinal vascular caliber: systemic, environmental, and genetic associations. Surv Ophthalmol. 2009;54(1):74–95.
Stepp DW, Boesen EI, Sullivan JC, Mintz JD, Hair CD, Pollock DM. Obesity augments vasoconstrictor reactivity to angiotensin II in the renal circulation of the Zucker rat. Am J Physiol Heart Circ Physiol. 2007;293(4):H2537–42.
Stapleton PA, James ME, Goodwill AG, Frisbee JC. Obesity and vascular dysfunction. Pathophysiology. 2008;15(2):79–89.
Liu M, Lycett K, Moreno-Betancur M, Wong TY, He M, Saffery R, Juonala M, Kerr JA, Wake M, Burgner DP. Inflammation mediates the relationship between obesity and retinal vascular calibre in 11-12 year-olds children and mid-life adults. Sci Rep. 2020;10(1):5006.
Li LJ, Ikram MK, Wong TY. Retinal vascular imaging in early life: insights into processes and risk of cardiovascular disease. J Physiol. 2016;594(8):2175–203.
Wong TY, Mitchell P. The eye in hypertension. Lancet. 2007;369(9559):425–35.
Grunwald JE, Brucker AJ, Schwartz SS, Braunstein SN, Baker L, Petrig BL, Riva CE. Diabetic glycemic control and retinal blood flow. Diabetes. 1990;39(5):602–7.
Saldívar E, Cabrales P, Tsai AG, Intaglietta M. Microcirculatory changes during chronic adaptation to hypoxia. Am J Physiol Heart Circ Physiol. 2003;285(5):H2064–71.
Wong TY, Islam FM, Klein R, Klein BE, Cotch MF, Castro C, Sharrett AR, Shahar E. Retinal vascular caliber, cardiovascular risk factors, and inflammation: the multi-ethnic study of atherosclerosis (MESA). Invest Ophthalmol Vis Sci. 2006;47(6):2341–50.
Kifley A, Wang JJ, Cugati S, Wong TY, Mitchell P. Retinal vascular caliber and the long-term risk of diabetes and impaired fasting glucose: the Blue Mountains Eye Study. Microcirculation. 2008;15(5):373–7.
Brinkley TE, Justice JN, Basu S, Bauer SR, Loh KP, Mukli P, Ng TKS, Turney IC, Ferrucci L, Cummings SR, Kritchevsky SB. Research priorities for measuring biologic age: summary and future directions from the Research Centers Collaborative Network Workshop. Geroscience. 2022;44(6):2573–83.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, Collins R, Allen NE. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186(9):1026–34.
Batty GD, Gale CR, Kivimäki M, Deary IJ, Bell S. Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. BMJ. 2020;368:m131.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This present work was supported by the NHMRC Investigator Grant (APP1175405); high-level Talent Flexible Introduction Fund of Guangdong Provincial People’s Hospital (No. KJ012019530); Fundamental Research Funds of the State Key Laboratory of Ophthalmology, National Natural Science Foundation of China (82000901); Project of Investigation on Health Status of Employees in Financial Industry in Guangzhou, China (Z012014075); and Science and Technology Program of Guangzhou, China (202002020049). Professor Mingguang He receives support from the University of Melbourne through its Research Accelerator Program and the CERA Foundation. The Centre for Eye Research Australia (CERA) receives Operational Infrastructure Support from the Victorian State Government.
Author information
Authors and Affiliations
Contributions
Study concept and design: Zhu ZT, Chen RY; acquisition, analysis, or interpretation: all authors; drafting of the manuscript: Chen RY, Xu JY, Zhu ZT, Wang W; critical revision of the manuscript for important intellectual content: Zhu ZT, He MG; statistical analysis: Chen RY; obtained funding: He MG, Zhu ZT, Wang W; administrative, technical, or material support: Zhu ZT, Wang W, He MG; study supervision: Zhu ZT, He MG.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 29 kb)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chen, R., Xu, J., Shang, X. et al. Association between cardiovascular health metrics and retinal ageing. GeroScience 45, 1511–1521 (2023). https://doi.org/10.1007/s11357-023-00743-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-023-00743-3