Abstract
Cemetery leachate generated by the process of cadaveric decomposition is a significant contaminant of several matrices in the cemetery environment (soil, groundwater, and surface water). The biogenic amines cadaverine and putrescine stand out among the cemetery leachate contaminants, since they are potentially carcinogenic compounds. This review article presents a discussion of possible environmental impacts caused by the increase in deaths resulting from COVID-19 as its central theme. The study also aims to demonstrate the importance of considering, in this context, some climatic factors that can alter both the time of bodily decomposition and the longevity of the virus in the environment. Additionally, some evidence for the transmission of the virus to health professionals and family members after the patient’s death and environmental contamination after the burial of the bodies will also be presented. Several sources were consulted, such as scientific electronic databases (NCBI), publications by government agencies (e.g., ARPEN, Brazil) and internationally recognized health and environmental agencies (e.g., WHO, OurWorldInData.org), as well as information published on reliable websites available for free (e.g., CNN) and scientific journals related to the topic. The data from this study sounds the alarm on the fact that an increase in the number of deaths from the complications of COVID-19 has generated serious environmental problems, resulting from Cemetery leachate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main anthropic sources of environmental contamination are agriculture, industry, and urban activities, such as sanitary landfills, effluents from the Water and Wastewater Treatment Plants, and, more recently included in this last group, cemetery environments (Jonker and Olivier 2012). Necropolises, as cemeteries are also called (Campos 2007), receive constant and intense additions of chemical compounds of high toxic potential, which have serious impacts on the environment and the surrounding biota, in addition to harmful effects on human health (Łukaszuk et al. 2015).
The cadaveric decomposition process generates a liquid called cemetery leachate (Dent et al. 2004), which is rich in mineral salts and organic substances called biogenic amines, such as cadaverine and putrescine. These biogenic amines, in addition to being highly toxic to living beings, may also be associated with diseases such as cancer (Pegg 2013; Thomas and Thomas 2001). Although the contamination caused by the disposal of corpses in cemeteries presents risks to human health, this type of environment has attracted little attention from civil communities and government institutions regarding their polluting potential.
The overflow of cemetery leachate, which occurs during the cadaveric putrefaction process, allows the cemetery leachate to percolate in the soil and transmit contaminants from the body’s own decomposition; chemical compounds used during the life of the buried person, such as medicines for daily use and chemotherapy; substances used in the body’s preservation and preparation processes, such as preservatives and makeup; as well as compounds derived from additional items, such as pacemakers, personal jewelry, paints, varnishes, and metallic elements from the mortuary urn (Zychowski and Bryndal 2015). In addition to the chemical compounds mentioned, biological materials may also be transmitted, such as bacteria and viruses, related to the individual’s cause of death which puts the environment and public health at risk (Anjos 2013).
The cemetery leachate and all the aforementioned compounds can be characterized as a polluting load that can reach and contaminate the soil and surface and underground water resources near the cemetery (Zychowski and Bryndal 2015). The problem can be further aggravated when the surrounding population makes direct use of water resources that are under the influence of cemeteries, as they will be predisposed to waterborne diseases (Kemerich et al. 2012).
The COVID-19 pandemic, caused by the new coronavirus or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), began in late 2019 in China’s Wuhan city. Since then, an overwhelming and deadly scenario has taken over the world (CarodArtal 2020; Madabhavi et al. 2020). According to data from the Center for Systems Science and Engineering (October 1, 2020) and WHO (2020a), the number of deaths registered in the world due to COVID-19 has already passed 900,000, data that only confirm the enormous impact of this pandemic on human health. In the same context, the World Health Organization (2020a) also disclosed that, by the end of September 2020, more than 900,000 deaths caused by COVID-19 had been registered worldwide. The two countries that have been most affected by the pandemic are the USA, with more than 190,000 deaths, and Brazil, with more than 125,000 deaths.
In view of the environmental problems related to cadaveric putrefaction and the increase in deaths registered in the world due to the pandemic, a concern has been established regarding the intensified impacts on cemetery environments. An important aspect to be considered, in addition to the presence of chemical compounds from the cemetery leachate, is the fact that the etiological agents SARS-CoV (Qu et al. 2020) and SARS-CoV-2 (Wang et al. 2020; Wu et al. 2020) have the ability to remain in the environment for long periods. Although all post-mortem activities (transportation, autopsies, delivery to families, burial, and exhumation) are supposed to be conducted in a way that avoids procedures that generate aerosols and release contaminated fluids after burial (Finegan et al. 2020), today there is an additional and serious concern about the spread of these viruses by bodies that were buried without undergoing appropriate decontamination treatments.
Due to the general dynamics of cadaveric decomposition, which produce potentially toxic compounds, it is clear that contamination in cemeteries correlates to the number of buried bodies, as well as site-specific climatic and geological characteristics (Zychowski and Bryndal 2015). Thus, it is possible to infer that the high number of human losses caused by the COVID-19 pandemic may also raise the level of contamination in cemetery environments and, consequently, in the surrounding urban environment, especially for medium to large cities. The abrupt increase in the number of deaths that have been recorded during the pandemic period, which has occurred throughout the entire planet, has caused many to worry about the possible environmental impacts resulting from the pandemic. In this review article, data already described in the scientific literature regarding the contamination of necropolis will be presented, which will serve as a basis for a more in-depth discussion on the real environmental impact caused by the COVID-19 pandemic. Although cemetery environments are places that pose high risks to human health, they are either discussed very little or not at all as places of high contamination. However, the increase in death rates registered since March 2020 as a result of the pandemic highlights the need to consider, in a more punctual and emphatic way, the negative aspects that the pandemic has caused in cemetery environments, especially regarding the ecotoxicity of these areas. Since this contamination is not only restricted to cemetery environments it can affect a large surrounding area the aforementioned effect on the environment ends up impacting human health, a fact that considerably accentuates the need to discuss the contamination of cemeteries after the COVID-19 pandemic. The approach of this study includes not only the description of the possible environmental and human health impacts resulting from the pandemic but also calls for the need for health and environmental government agencies to pay more attention to cemeterial contamination.
Cadaverous decomposition processes
The main environmental impact of cemeteries is caused by the cadaverous decomposition process (Pacheco and Matos 2000). The nomenclature and the stages of the body putrefaction process can vary from four to six stages (Carter and Tibbett 2008). In the so-called fresh or initial stage of decomposition, there is no overflow of cemetery leachate; the emphysematous phase (or putrefaction stage) is marked by the production of organic acids, gases, and biogenic amines, but without being released into the external environment; in the colliquative (or black putrefaction) stage, cemetery leachate is released due to the rupture of the skin; saponification (or butyl fermentation) is characterized by the formation of fatty acids in the regions with the highest accumulation of triglycerides in the decomposing body; in skeletonization (or dry decomposition), there is no production of cemetery leachate, however, there is the degradation of bone structures; the release of minerals is the last phase, where the remains start to release minerals previously present in the tissues (Bornemissza 1957; Carter and Tibbett 2008; Christensen et al. 2014). The last phase of the putrefaction process is skeletonizing. This phase takes days or even years to be achieved, while the complete disappearance of the corpse can take hundreds of years (Rodriguez and Bass 1983).
It is worth noting that the entire decomposition process follows the same stages for corpses, but there are specific characteristics of both the buried body and the environment that can interfere with the duration of time between one phase and another (Ioan et al. 2017). Among these particularities are clothing, age, body mass, gastric content, nutritional and hydration status, as well as the cause of death. The environmental characteristics involve pH, temperature, humidity, type, and composition of the soil where the corpse was buried (Vass et al. 2002; Pinheiro 2006; Carter and Tibbett 2008; Ioan et al. 2017; Antonio et al. 2018).
Increased burials cause greater cemetery leachate contamination
The main cause of contamination from cemeteries is the liquid continuously released by putrefying corpses, called cemetery leachate (Silva and Malagutti Filho 2008). Cemetery leachate is a more viscous liquid than water, rich in mineral salts and degradable organic substances, of grayish-brown color, with an acrid and fetid smell, polymerizable, with high biochemical oxygen demand (BOD), and varying degrees of pathogenicity (Matos and Pacheco 2001; Silva 1995). The cemetery leachate has an average density of 1.23 g/cm3, high values of conductivity, a pH ranging from 5 to 9, and temperatures from 23 to 28 °C. For every 1 kg of body weight, about 400 to 600 mL of cemetery leachate are produced. Its composition is 60% water, 30% mineralized substances, 10% organic substances, and various metals (Oliveira et al. 2013; Zychowski and Bryndal 2015).
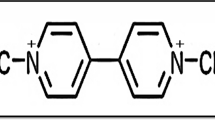
Among the organic compounds present in the cemetery leachate are the biogenic amines cadaverine (1,5-pentanediamine) and putrescine (1,4-butanediamine), which are small molecules, produced by the decarboxylation of amino acids through biosynthesis and enzymatic processes (Bachrach 2004). These amines are soluble in water, generate, when degraded, ammonium ions (NH4+), and are potentially highly toxic (Almeida and Macêdo 2005; Melo et al. 2010).
Toxicity of biogenic amines present in cemetery leachate
Toxicity of cadaverine and putrescine
Cadaverine (Cad) and putrescine (Put) biogenic amines are diamines that, in low concentrations, play important roles in organisms (Bach et al. 2012; Křížek et al. 2002; Ramani et al. 2014). They are involved in various natural biological processes such as brain activity, temperature and pH regulation, immune responses, cell growth, and differentiation in different organisms. However, biogenic amines, in general, can also be considered carcinogenic due to their ability to react with nitrites to form potentially carcinogenic nitrosamines (Shalaby 1996). Cad and Put are amines that have nucleophilic sites, which give them an easy connection with nucleic acids, lipids, and proteins. When these amines are in high concentrations, they can be toxic (Bach et al. 2012; Ladero et al. 2010) by altering the stability of these molecules (Bloomfield and Wilson 1981; Brysont and Greenall 2000; Hussain et al. 2011; Schuber 1989).
The toxicity of Cad and Put causes the activation of catabolic processes, which can generate an excessive increase in hydrogen peroxide (Pegg 2013; Thomas and Thomas 2001). In general, biogenic amines, when undergoing oxidation processes, generate unstable and potentially toxic compounds, such as aldehydes and hydrogen peroxide. Hydrogen peroxide is generated in the outer mitochondrial membranes, causing oxidative damage to mitochondrial DNA and other biomolecules, in addition to promoting neurodegenerative damage (Hauptmann et al. 1996; Pegg 2013).
Studies carried out where Wistar rats ingested Cad and Put indicated that the consumption of Put may be related to acute harmful effects, such as dilation of the vascular system, hypotension, and bradycardia (del Rio et al. 2019; Ladero et al. 2010; Shalaby 1996). In addition, both have indirect toxic effects that enhance the toxicity of other biogenic amines, such as histamine (del Rio et al. 2019; Til et al. 1997), by facilitating the passage of histamine into the small intestine, increasing its rate of absorption into the bloodstream. This is due to the inhibition of detoxifying enzymes (diaminaoxidase and histamine N-methyltransferase) involved in the oxidative catabolism of histamine (Al Bulushi et al. 2009; del Rio et al. 2019; Lyons et al. 1983; Paik Jung and Bieldanes 1979).
A study by Rauscher-Gabernig et al. (2012), on food contaminated by putrescine and cadaverine diamines, showed that these amines can potentiate the effects of histamine if ingested simultaneously. Although formed endogenously and essential for some metabolic pathways, these diamines are known as precursors of carcinogenic nitrosamines. Putrescine is a diamine that may also be involved in tumor growth. However, because there are few published studies on the toxicological levels of these substances, the authors claim that the tolerable levels disclosed for these amines may be underestimated and are characterized with some uncertainty.
Association of cadaverine and putrescine amines with carcinogenic processes in humans
The association of increased synthesis of biogenic amines with cell proliferation and cancer was first reported in the late 1960s (Andersson and Heby 1972; Gerner and Meyskens 2004). The cadaverine and putrescine diamines present in organisms can be nitrosated or they can act as precursors to other compounds capable of forming nitrosamines. Cadaverine produces nitrosopiperidine, and putrescine produces nitrosopyrrolidine. These compounds are considered carcinogenic to several animal species and represent a potential risk to human health (De Mey et al. 2014; del Rio et al. 2019; Ladero et al. 2010; Rauscher-Gabernig et al. 2012; Shalaby 1996).
Cadaverine is involved in several critical cellular processes in living organisms, including the induction of inflammation and necrosis in living tissues. In high doses, this diamine is considered a biochemical marker for some diseases, such as cancer, diabetes, arthritis, and cystic fibrosis (Jancewicz et al. 2016; Teti et al. 2002). Fusi et al. (2008) evaluated the effects of various concentrations of cadaverine on bovine mammary epithelial cells (BME-UV1) and in three-dimensional primary cultures (3D culture) of mammary parenchyma, also in bovine. The authors observed that, in both cultures, the lowest concentration of the diamine (10 mM) induced cell proliferation, while the highest (50 mM) inhibited proliferation.
Studies by Chen et al. (2015), in human skin fibroblasts, showed that low concentrations of putrescine (0, 5, 1.0, 5.0, and 10 μg/mL) induced cell proliferation, while higher concentrations (100, 500, and 1000 µg/mL) inhibited cell migration and proliferation, leading fibroblasts to apoptosis.
The putrescine polyamine is synthesized through ornithine decarboxylation and the action of the ornithine decarboxylase enzyme (ODC). Because this diamine has several cellular functions and is regulated at various times during cellular activity (during its synthesis, degradation, absorption, and efflux), it is very difficult to find consistent evidence about the cellular functions of these diamines. Studies carried out with this putrescine have turned up controversial results on the role of ODC in carcinogenesis and apoptosis (Thomas and Thomas 2001). Based on this information, these same authors have suggested that the different actions of putrescine may be related to the differences inherent to the cell type involved in the putrescine uptake, thus characterizing differences in cellular sensitivity to apoptosis (Thomas and Thomas 2001).
Cemetery leachate chemicals
After burial, chemical, and biological agents are released from the body caused by chemical substances applied in the individual’s life, such as chemotherapy, dental implants, metallic prostheses, among other materials, which end up contaminating the environment. In addition to these materials for human use, there is also the supply of metallic contaminants and coatings used in the manufacture of mortuary urns. Metallic compounds can corrode and infiltrate the soil and be carried to underground bodies of water near the burial site (van Allemann et al. 2019). These same authors also warn that cemeteries are characterized by environments potentially contaminated by dangerous metals, such as aluminum, iron, copper, and zinc. The environment contamination of cemetery by metals is also described by Aruomero and Afolabi (2014), who cites the presence of lead, arsenic, mercury, nickel, copper, cadmium, zinc, silver, bronze, and chromium. In addition to these metals, most coffins are made of wood that undergoes a treatment process with preservatives and are subsequently painted and/or varnished for a longer duration (Gondal et al. 2011). All these components are easily associated with cemetery leachate, which optimizes its percolation in the soil, its flow into surface waters, or its leaching into groundwater (van Allemann et al. 2019).
Several factors contribute to the mobility and corrosion rate of metals related to burials. The most studied factors are the following: the type of metal present in bodies and urns; the edaphic conditions in which the body is buried; and climatic factors, such as temperature and precipitation in the region. These variables play an important role in relation to the accumulation, transmission, and corrosion of materials in cemetery environments (Silva et al. 2020).
According to Jonker and Oliver (2012), a South African cemetery in Tshwane contains more than 60,000 tombs, which can release about 108,000 kg of metals from the constituent parts of the coffins into the environment. From the moment these metals suffer corrosion and are introduced into the environment, they can accumulate in the short and/or long-term, and characterize a serious risk to public health (Bianchi et al. 2011; Dourado et al. 2017; Matsumoto and Marin-Morales 2004) mainly because their adverse effects may not be immediately observable and can compromise the following generations (Paíga and Delerue-Matos 2016).
Another worrying factor, in addition to the release of metals into the environment, is the embalming process of the body (thanatopraxy), a practice commonly undertaken since Ancient Egypt. In this process, fluid substances that do not degrade easily are applied (Nogueira et al. 2013). The thanatopraxy aims to maintain the color, conservation, and asepsis of the corpse. In this process, fluids are injected, such as formaldehyde, acetate and potassium nitrate, glycerin, and chrome paint (Souza and Botelho 1999), which are not degraded in the cadaveric decomposition process and, therefore, easily pass into the soil and groundwater (Matos and Pacheco 2001).
During the cadaveric decomposition process, large quantities of substances with a high degree of toxicity are released, such as hydrogen sulfide, carbon dioxide, methane, ammonia, cadaverine, and putrescine. These substances, in addition to contaminating the soil, can also reach the groundwater through a leaching process, thus increasing the potential for environmental impact (da Kemerich et al. 2014; Neckel et al. 2017; Dalmora et al. 2020).
The cadaverous decomposition process and contamination by pathogens
After death, the human body becomes the substrate of an ecosystem composed of several saprophytic microorganisms (Antonio et al. 2018). The microorganisms involved in the cadaveric decomposition, according to Całkosiński et al. (2015), can impact the environment and also pose a risk to human health.
The decomposition process is initiated by enterobacteria from the body itself, which overtake the intestinal epithelium and invade adjacent tissues (Carneiro 2008). Gram-negative enterobacteria present in the decomposition process have also been found in the cemetery leachate (Antonio et al. 2018). Among the bacteria of the cemetery leachate are the genera Clostridium and Salmonella, in addition to E. coli, bacteria that are involved with diseases such as tetanus, typhoid fever, gas gangrene, and dysentery.
Studies by several authors (Kandoli et al. 2019; Rodrigues and Pacheco 2003) show that there is a high level of microbial contamination in groundwater samples collected in the vicinity of cemeteries (Kandoli et al. 2019; Rodrigues and Pacheco 2003; Zychowski and Bryndal 2015). It was also observed that the survival of these pathogens can vary in the soil. Specific characteristics of the soil, such as permeability, aeration, humidity, and nutrition factors, alter the effectiveness of microorganism retention (Silva and Malagutti Filho 2008). Some more resistant microorganisms can survive for more than 5 years in the soil, under favorable environmental conditions, and, during this period, they can mobilize and reach and contaminate aquifers (Zychowski and Bryndal 2015). Research carried out in tropical countries shows an influence of climatic and edaphic conditions on the biological contamination of the environment (Ourives et al. 2017). An example of this is that environmental samples collected in Brazilian and South African cemeteries showed higher levels of pathogens than samples collected in colder environments (Zychowski and Bryndal 2015).
Studies on the migration potential of bacteria and viruses, carried out by Pacheco and Matos (2000) on samples collected in cemetery environments, show that viruses have a greater capacity for mobility in the soil when compared to bacteria. Few studies have analyzed virus contamination in necropolises; however, the presence of adenoviruses and enteroviruses has already been detected in water samples collected in these environments. It is worth mentioning that, in the places where the graves were closer to the water table, the level of contamination was higher (Zychowski and Bryndal 2015).
Prescott et al. (2015) carried out a relevant study on the stability of the Ebola virus, after the outbreak that started in 2014 in West Africa. In this study, the authors evaluated tissue samples from five monkeys that died from being infected by the virus, to ascertain the stability and transmissibility of the virus, as well as the presence of viral RNA in these samples. It was possible to detect, using the RT-PCR technique, the presence of the virus in the different samples, for up to 3 weeks after the death of the primates. They detected the virus was viable and replicating within a cell culture, demonstrating its viability for up to 7 days after the euthanasia of the animals (Prescott et al. 2015).
Currently, the outbreak of infection of the new coronavirus has become a risk on a global level, due to its speed in both contamination and spread throughout the world. The survival time of this virus in the corpse, after burial, is still uncertain (Calmon 2020), which makes this scenario more worrying, because, in cities whose water and wastewater treatment plants are flawed, the population can be directly exposed to the biological material leached from the cemetery leachate, increasing the risk of contamination (Nascimento 2020).
Although an improvement in the US and Chinese air quality was reported during the COVID-19 pandemic (Shakoor et al. 2020), an increase in the mortality rate, and hence the number of burials, is most likely negatively altering the quality of other environmental matrices, such as soil and groundwater. Thus, the need to assess the impact of cemetery environments and the impairment of this type of contamination on human health is pertinent.
SARS-CoV-2 survival time in different environments
While some researchers related the transmissibility of the virus to meteorological factors, such as temperature and humidity (Doğan et al. 2020; Shahzad et al., 2020a, b; Sarwar et al. 2021), others have already estimated the survival time of SARS-CoV-2 in different environments and environmental conditions. Seetulsingh et al. (m2020) reported a case of a patient who died on suspicion of COVID-19 and, due to an administrative delay, the autopsy was performed 27 days after his death. During this period, the body was kept at a temperature of 4 to 6 °C. After that period, PCR analysis for COVID-19 and histological analysis of lung tissue were performed. Since these analyses confirmed that the patient’s cause of death was from COVID-19, it was not necessary to carry out other internal studies. This case was the first study to detect the virus in lung tissue, carried out well after the patient’s death. Thus, from this study, it was possible to infer that the virus can persist and remain viable in cadavers, which alerted the medical-scientific community to the need for the proper use of personal protective equipment (PPE), for handling bodies affected by COVID-19 or when conducting postmortem examinations.
Some studies carried out with the aim of mitigating the COVID-19 pandemic have shown that the survival of SARS-CoV-2 is dependent on the type of surface it is attached to. Hirose et al. (2020) evaluated the stability of SARS-CoV-2 on human skin obtained from forensic autopsies and identified that the SARS-CoV-2 strain can remain alive for up to 9 h on human skin. This extended permanence on the skin allows for an increased risk of self-contamination and transmission to other surfaces and even to other people. In that same study, the difficulty in carrying out the same type of study on the skin of living people, as it is a highly infectious agent, was highlighted. However, some authors (Hirel et al. 1996; Boekema et al. 2015; Akutsu et al. 2019) cite that autopsy performed on the skin of individuals 24 h after their death can serve as a model for a better understanding of the viability of the virus in humans.
van Doremalen et al. (2020) analyzed the stability of SARS-CoV-2 in aerosol, plastic, stainless steel, copper, and cardboard, at temperatures ranging from 21 to 23 °C and 40% humidity. SARS-CoV-2 remained viable in aerosols for 3 h, on plastic for up to 72 h, and on stainless steel for 8 h. On copper, SARS-CoV-2 was no longer detected after 4 h of contamination, and on cardboard, no viable SARS-CoV-2 was observed after 24 h. With these data, it is possible to affirm that the transmission of SARS-CoV-2 can happen through aerosol and by human contact with contaminated surfaces because the virus can remain viable and infectious for hours in aerosols and for days on solid surfaces.
Temperature is one of the main factors that influence the survival of the virus. High temperatures can cause protein denaturation and increase the activity of extracellular enzymes. Temperature can be a denaturant factor for proteins since it can break hydrogen bonds leading to an alteration in the sites for these macromolecules. As described by Wang et al. (2004), viral proteins can be denatured by heat. Both the N-proteins (nucleocapsids) and the viral S proteins (membrane proteins), when in a phosphate-buffered saline buffer, begin to unfold at 35 °C, and exhibit complete denaturation at 55 °C. The author also mentions that these SARS-Cov-2 proteins are irreversibly denatured by heat. This denaturation begins when the medium reaches 35 °C and is completed in 10 min at 55 °C. In addition to this factor, exposure to light, the presence of organic matter, and other microorganisms can also interfere with coronavirus survival (Gundy et al. 2009; Naddeo and Liu 2020).
SARS-CoV-2 is composed of a protein capsid, genetic material, and an enveloping lipid membrane, derived from the host cell. This virus infects animal cells and replicates in the cytoplasm of those cells (Spriggs et al. 2019) . Although the membrane gives this virus greater ease of entry into host cells (endocytosis) (Spriggs et al. 2019), this envelope is fragile and, in general, is less stable in an environment contaminated by oxidizing agents, such as chlorine. Studies have shown that this pathogen survives 2 days (20 °C) in water not treated with chlorine and in untreated hospital sewage. Thus, the characteristics of the effluents from water treatment facilities influence the survival time of the virus (Rolemberg et al. 2020; WHO 2020a). Medema et al. (2020) analyzed the sewage networks of two hospitals in the Netherlands and, in both sewers, the presence of SARS-CoV-2 was detected. Wu et al. (2020) observed, in March 2020, a high concentration of the virus in wastewater from a Massachusetts wastewater treatment plant. Therefore, the efficiency of the disinfection process used in water and wastewater treatment plants is of crucial importance for the inactivation and, consequently, the removal of this pathogen from the effluents of the treatment plants (Rollemberg et al. 2020). This concern is supported by Fareed et al. (2020), who mention that the countries with the greatest environmental quality problems are listed as the ones with the highest number of deaths from COVID-19.
The studies discussed above reinforce that water transmission in environments contaminated by SARS-CoV-2 can aggravate transmission potential. The evaluations performed up until now are still insufficient in elucidating the extent of this type of contamination, since little research has been carried out on the survival time of this virus in a post-mortem situation and on the risks of human exposure during that period. Considering the increase in the mortality rate, as a result of the increase in the number of people contaminated by SARS-CoV-2, the need to discuss and evaluate the environmental and public health impacts of environments potentially contaminated by SARS-CoV-2 is evident, including in cemetery environments.
Contamination of soils, groundwater, and surface waters by cemeteries
The overflow of cemetery leachate, the main pollutant in cemeteries, resulting from the decomposition of corpses, reaches the soil and causes, in addition to an increase in microbial activity, an increase in the levels of nitrogen, phosphorus, mineral salts, and electrical conductivity (Kemerich et al. 2012; Silva and Malagutti Filho 2008; Zychowski and Bryndal 2015).
Soil contamination is dangerous to human health and environmental quality and, because it is often visually imperceptible, can be characterized as a hidden danger (Rodrígues-Eugenio et al. 2018). A type of mechanical filtration can occur in the soil, which retains larger particles, such as bacteria and viruses. Viruses can attach themselves to the soil due to the electrical charges of mineral particles. Although this fixation may not be permanent, it can result in significant health problems (Nascimento 2020; Pacheco 2017).
As already mentioned, another alarming and high-risk factor is the contamination of groundwater, which occurs through the percolation of the cemetery leachate into the unsaturated area of the soil. The contamination dynamics, which can be initiated, for example, by graves that have cracks, depends on the type of soil where the cemeteries are installed. Cemeteries with more sandy substrates have a greater potential for contamination, as they have more porous and permeable soils, while soils classified as clayey have a greater capacity for cemetery leachate retention, as they are more compact and impermeable (Campos 2007; Silva and Malagutti Filho 2008).
When the leachate of cemeteries reaches the aquifers, these groundwaters become vehicles of contamination, and its spreads to external areas as the vicinity of the cemeteries (Pacheco 2017). Such contamination poses risks to the environment since groundwater is important for the balance of the planet. As these waters flow slowly to lakes, rivers, and oceans, it is extremely difficult to recover a contaminated aquifer (Giampá and Gonçalves 2005). Another complication is the fact that groundwater can often be used to supply the population, putting people’s health at risk, as is the case with residents in the vicinity of cemeteries, who end up consuming polluted water, resulting in negative consequences on their health (Pacheco 2017).
Surface waters can also be impacted by necropolises. In cemeteries that do not have an efficient drainage system, where the land is waterproofed by tombs and by paving the streets, there is an impediment to draining rainwater, which can accumulate on the site. These waters can then flood tombs, drain, and reach areas outside the cemetery, transporting contaminants to the urban rainwater network and, consequently, to water bodies in the region (Silva and Malagutti Filho 2008). Due to these contamination possibilities, there is a need to adequately structure the cemeteries, so that these environments are prepared to receive the corpses, without causing impacts on water resources and the surrounding urban areas (Neckel et al. 2017).
Water is an indispensable natural resource for the survival of life on the planet. Its quality is closely related to environmental quality and public health (Westall and Brack 2018). As evidenced by Pacheco (2017), the lack of sanitation and the consequent contamination of water results in high rates of hospitalizations and deaths as is seen in developing countries.
Among anthropic sources, cemeteries are the most asymptomatic, silent, and continuous sources of water contamination (Pacheco 2017). This is extremely concerning, due to the fact that the population is unaware of the polluting potential of the by-products of cadaverous decomposition happening in these environments (Anjos 2013). Due to this lack of knowledge, there may be negligence in relation to the necessary care when handling soils in these places or when using groundwater, which is influenced by this type of contamination, for supply (wells). In addition to these public health problems, the contamination of natural resources, such as soil and water, is also extremely harmful to the environment, since, with population growth, these resources are already scarce and more degraded (Tormen et al. 2016). Fagundes et al. (2020) points out that water is a resource that is becoming increasingly scarce, both in quantity and quality. The author mentions that a good part of the water available for consumption is extracted from groundwater and that these waters correspond to about 30% of all freshwater on the planet, reinforcing the need for its conservation.
Cemeteries are a significant global source of pollution since they contribute to the introduction of physical, chemical, and biological agents exogenous to the environment, which, consequently, compromises the health of both the population living in proximity to them (Nogueira et al. 2013; Neckel et al. 2016, 2017) and the use of the water contaminated with its by-products.
Increase in mortality
The number of deaths from the COVID-19 pandemic is being considered a negative and frightening milestone in human history. Due to the lack of efficient treatment, and the delay in large-scale vaccinations, protective measures such as social distancing, strict personal, and object hygiene, as well as the use of personal protection equipment (PPE), have been adopted and recommended worldwide. As can be seen in Tables 1 and 2, the deaths registered for COVID-19 vary considerably according to the country or region considered. This variation is related to the speed with which strategies are implemented in mitigating the spread of the disease, such as carrying out diagnostic tests in the population and the determination and encouragement of effective social isolation.
According to the data, the American continent has the majority of COVID-19 confirmed deaths, corresponding to 47.46% of the total global value. A few American countries (USA, Brazil, and Mexico) lead the world numerical ranking for cases of death by COVID-19, as can be seen in Table 2.
According to current data on the mortality rate of the SARS-CoV-2 infection, the country that draws the most attention is the United States of America (USA), which leads in deaths (407,565) and confirmed cases (27,690,000), despite the low mortality rate (1.7%) compared to the world average (2.1%). The cases of deaths from COVID-19 in this country correspond to 19.57% of the total deaths worldwide (Table 2). Brazil ranks second in the number of dead (212,831) and third in confirmed cases (9,870,000), behind the USA and India (10,930,000). The Brazilian mortality rate is 2.5%, slightly above the world average. Mexico’s situation is concerning since they reached a total of 144,000 deaths in January 2021 and a mortality rate of 8.5%, much higher than the global rate (Table 2).
Considering Latin America, the numbers show more virus dissemination and deaths in the South (Table 3).
Regarding the data from Latin America, it is possible to observe that in several countries, the mortality rates are above the world rate, registered as 2.1%. Among the countries listed in Table 3, Mexico, Ecuador, and Bolivia are those with the highest mortality rate (8.5%, 6.2%, and 5.0%, respectively). However, as the largest and most populous country in this region, Brazil leads the number of deaths and cases confirmed by COVID-19 (212,831 and more than 8.5 million, respectively).
Pandemic data from Brazil
According to Roser et al. (2021), Brazil has approximately 8.64 million COVID-19 confirmed cases. Comparing this data with the total population (approx. 212.56 million), 4.0% of the population was contaminated by the coronavirus. However, compared with the total number of contaminated people around the world (96.86 million), this rate rises to 8.92%. Comparing the numbers of cumulative confirmed COVID-19 deaths, Brazil registered 212,831 among 2.07 million deaths around the world, resulting in 10.28% of the death toll. It is important to note that the Brazilian population comprises only 2.72% of the world population.
In order to estimate the increase in the number of deaths in Brazil, the records from March 16 to December 31, 2020, were compared with the same time interval as in the year 2019. To assess the effects of COVID-19, in relation to the possible worsening of more specific symptoms, data on deaths from respiratory causes and heart disease was collected, as shown in Tables 3 and 4, respectively.
From the analysis carried out between the values of the two tables (4 and 5), it is possible to observe an increase of approximately 18.44% in the number of deaths from 2019 to 2020, for the same period. However, there are several variations regarding the registered causes. Table 4 shows a significant decrease in the number of deaths caused by respiratory insufficiency, pneumonia, and septicemia. On the other hand, there was a considerable increase in deaths from undetermined causes and severe acute respiratory syndrome, in addition to deaths from COVID-19. Table 5 also shows a decrease in the number of deaths for specific heart diseases, such as stroke and heart attack, while the values for other unspecific cardiovascular diseases have increased. In the database used (Arpen 2021), unspecific cardiovascular diseases were considered: sudden death or cardiorespiratory arrest, arterial hypertension, heart failure, dilated cardiomyopathy, atrioventricular block, cardiac arrhythmia, supraventricular tachycardia, ventricular tachycardia, atrial fibrillation, bradyarrhythmia, and cardiogenic shock associated with ischemic disease.
These observations may be due to insufficient testing for COVID-19, which must be masking the real effects of the pandemic on the Brazilian population, in terms of the number of infected and consequently of deaths. This situation is probably happening in other developing countries around the world. For the analysis of the effects of the pandemic on the Brazilian states (Table 6) and the geographic regions of Brazil (Table 7), several factors should be considered.
While the Southern region has had little change in the number of deaths recorded for 2019 and 2020, the other regions showed significant increases for the same period considered. Comparing the data, it is possible to highlight that the increases for the North, Midwest, and Northeast regions (31.36%, 26.21%, and 21.23%, respectively) were the most expressive recorded in Brazil (Table 7).
The increase recorded in the North of Brazil was due to the variations observed for the states of Amazonas (43.37%), Pará (33.38%), and Roraima (25.40%). With the exception of the states of Acre, Amapá, Rondônia, and Tocantins, the others increased more than 25.00% (Table 6). The capital of Amazonas, Manaus, already at the beginning of April, had declared the collapse of the healthcare system, where 95% of the 293 ICU beds were occupied (Calmon 2020). Recently, this Brazilian state faced an even worse scenario of health system collapse. After increasing the number of beds, 100% of the ICU beds in the state were occupied, and there was a depletion in the number of oxygen tanks, which is necessary to ventilate patients (MSF 2021).
In relation to the Northeast region of Brazil, the states of Alagoas (14.96%), Ceará (38.25%), Maranhão (36.98%), Pernambuco (19.48%), and Bahia (19.92%) reported the highest increase in the number of deaths (Table 6). According to Fiocruz Pernambuco (2020), there is a higher incidence of deaths in the North and Northeastern Brazilian states and, as regions of low socioeconomic development, the effects of the disease were more devastating.
A history of the spread of COVID-19 in Brazil considers that the disease reached the country in more developed areas, due to the fact that SARS-CoV-2 was introduced by travelers who circulated in China, Europe, and the US. As the disease progressed to the interior of the states and reached poorer regions, the impact of the disease on the population increased (Fiocruz Pernambuco 2020). Also, according to data from this Brazilian health institution (Fiocruz Pernambuco), the Northern and Northeastern regions of Brazil, which have the lowest socioeconomic development in the country, were the most negatively impacted by the disease and saw the greatest socioeconomic problems. These data are corroborated by Iqbal et al. (2020), where the authors state that the most important factor to be considered in containing the spread of the disease in the Wuhan region (China) was the socioeconomic factor.
The Southeast is the region with the highest number of deaths (Table 6) and the highest population density in the country. The state of São Paulo and its capital were already considered the epicenter of the disease in Brazil (Calmon 2020; El País, 2020). However, Manaus, the capital of the state of Amazonas, is now considered the main region of COVID-19 in Brazil (MSF 2021).
The concern over the increase in the number of COVID-19 cases identified in Manaus (Amazonas state—Brazil), until November 2020, intensified even more after the emergence in the region of a new variant, called VOCP.1 (Variant Of Concern P.1). This new variant, which appeared at the end of December 2020 (identified in January 2021), was responsible for the second wave of cases of the disease, causing collapse both to the healthcare system and hospitals in the region of Manaus. This new SARS-CoV-2 variant presents important mutations that make the virus more transmissible (superior to other strains, with higher risks of reinfection) and more aggressive, as the worsening in patients’ symptoms is faster (Singanayagam et al. 2020; Faria et al. 2021). For this reason, Brazil today stands out on the world stage as being the new worldwide epicenter of the dissemination of SARS-CoV-2 VOCP.1.
The SARS-CoV-2 VOCP.1 variant spread rapidly throughout Brazil, reaching 17 of the 27 Brazilian states (CNN 2021). The World Health Organization (WHO 2021) stated in its epidemiological report on COVID-19 that the Manaus variant has already reached eight countries (Brazil, Japan, United States, United Kingdom, Italy, Germany, South Korea, and Ireland). Thus, SARS-CoV-2 VOCP.1 is today one of the biggest global concerns in relation to COVID-19.
Management of bodies and transmission of SARS-CoV-2 after death
Transmission of infectious diseases can occur during the handling of bodies and also through contact with contaminated hospital equipment, especially when there are no properly trained personnel or personal protective equipment (PPE) is absent or inadequate (Calmon 2020).
Although the lethality of SARS-CoV-2 is low (on average 3.0 to 4.0%) (Fineschi et al. 2020; WHO 2020a) for doctors and other health professionals, since they are exposed to a higher viral load, they are more subject to the risks associated with this etiologic agent. For this reason, these professionals must strictly follow self-protection recommendations to avoid contamination. Due to the ease with which the disease spreads, the World Health Organization (WHO 2020a) released basic guidelines for the proper management of those who died from COVID-19.
The WHO document provides instructions for handling the bodies of COVID-19 victims in order to prevent leakage of body fluids and the spread of the virus. In Brazil, the bodies that will be transported for burial or cremation must have all orifices sealed, must be covered with fabric (sheets), and be placed in an appropriate waterproof bag. Then, a second bag must be used after be cleaned with 70% ethanol, a chlorinated solution (0.5 to 1.0%), or with some other sanitizer authorized by ANVISA, the Brazilian health surveillance agency (Brasil 2020) . The WHO guidelines do not require the use of impervious bags for the corpses of COVID-19 but recommend them only in cases of excessive leakage of bodily fluids or in the absence of refrigerated morgues, and especially in countries with hot weather. A second bag is only recommended if burial exceeds 24 h after death or if burial or cremation cannot occur within the next 24 to 48 h (WHO 2020b). Even with all the added precautions for the proper transport of the dead by SARS-CoV-2, another problem that can aggravate the spread of the disease occurs when the cause of death is documented with unknown origin, due to the delay in testing to confirm the infection. This lack of information compromises the performance of adequate body management procedures and increases the risk of contamination of personnel who manage these deaths (Calmon 2020).
Other publications have released relevant policies and some suggestions for safety protocols involving Covid-19, with information and detailed guidelines for professionals involved in handling the bodies of people with suspected or proven cause of death as COVID-19 (Finegan et al. 2020; Fineschi et al. 2020). However, in addition to the concern for the health of these people, the increase in the number of deaths and, consequently, burials, is concerning for public and environmental health.
In Brazil, more specifically in the state of Amazonas, 6,268 deaths were recorded between April, May, and June 2020, whose bodies were either buried or cremated. Of the 5,246 burials (83.6% of those killed), 2,435 occurred in April, 1,899 in May, and 912 in June. The number of burials recorded for the same period in 2019 was 871 for April, 860 for May, and 842 for June, totaling 2,573 deaths for the same period. Comparing the data from these two years, it can be seen that, in 2020, there was an increase of 179.5%, 120.8%, and 8.31%, for the months of April, May, and June, respectively (D24AM 2020). In Cuiabá, the Brazilian state of Mato Grosso, a daily average of 20 burials was recorded in 2020, an increase of 300.0% when compared to the values recorded in the same period of 2019 (Garcia 2020).
As previously mentioned, viruses have a high capacity for survival, mobility, and contamination. In the case of SARS-CoV-2, professionals working in cemeteries must follow the same biosafety rules against infectious diseases adopted in hospital environments (Nascimento 2020). Since the time that the virus can remain in the corpse is uncertain, there is a potential risk of contamination for both the family of the deceased and for the agents of the funeral services (Neckel et al. 2017).
According to Finegan et al. (2020), burial in individual graves is the best strategy to be adopted for the disposal of the bodies affected by COVID-19, taking into account the care described above to avoid carrying remnants of decomposition of the bodies to groundwater. In addition, if the family opts for the exhumation process, the professionals involved in this process must follow the necessary care, from the preparation of the body to the correct disposal of waste (Neckel et al. 2017). Many other guidelines exist for the transport, handling, and preparation of bodies, as well as the use of PPE that enhance the protection of professionals and can be found in the manual prepared by the Pan American Health Organization, in collaboration with the International Committee of the Red Cross (Cordner et al. 2016).
Due to the high number of deaths by COVID-19 in the world, it is necessary to pay more attention to the correct handling and disposal of the bodies affected by the virus, as well as to ensure the adequacy of cemetery facilities, so that these environments are in compliance with public health and environmental quality laws.
Final considerations
The cadaveric decomposition generates a liquid with toxic potential, called the “colliquation” or cemetery leachate product, which impacts both human health and the environment.
Cemetery leachate is a viscous liquid with a brownish-gray color and a strong odor, composed of 60% water, 30% mineral salts, and 10% organic substances. Among the inorganic compounds of the cemetery leachate are ions of nitrogen, phosphorus, Cl, HCO3−, Ca2+, Na+ and metallic compounds of Ti, Cr, Cd, Pb, Fe, Mn, Ni. Among the organic compounds are biogenic amines, such as cadaverine and putrescine, which are toxic substances and potentially carcinogenic. The cemetery leachate still contains a range of microorganisms and viruses, which gives this liquid a worrying pathogenic potential.
Due to the liquid characteristic of the cemetery leachate, it can seep into the soil and carry with it both its chemical compounds and the biological agents present, thus contaminating, in addition to the soil, the ground and surface waters of the region impacted by its presence.
Environmental contamination resulting from the cadaverous decomposition that takes place in cemeteries can lead to considerable impacts in the most diverse environmental networks, and also to serious risks to human health.
Due to the high number of deaths resulting from the negative effects of the COVID-19 pandemic; the dangers that decomposing bodies pose to the contamination of soils and water resources; and the possible transfer of pathogens from cadavers, such as viruses and bacteria, to the environment, the importance of strictly following the pre-established protocols and procedures for the burial of bodies contaminated with COVID- 19, and to assess the infrastructural conditions of the cemetery environments that are receiving this large number of victims of this pandemic. These precautions are essential to prevent contamination in the work environment and ensure the health of employees, visitors, and the population residing in the vicinity of these environments, or even people who make use of groundwater for subsistence, with the possibility of contamination resulting from leaching that occurs in cemeteries.
References
Akutsu T, Ikegaya H, Watanabe K, Miyasaka S (2019) Immunohistochemical staining of skin-expressed proteins to identify exfoliated epidermal cells for forensic purposes. Forensic Sci Int 303:109940. https://doi.org/10.1016/J.FORSCIINT.2019.109940
Al Bulushi I, Poole S, Deeth HC, Dykes GA (2009) Biogenic amines in fish: Roles in intoxication, spoilage, and nitrosamine formation-a review. Crit Rev Food Sci Nutr 49:369–377. https://doi.org/10.1080/10408390802067514
Almeida AM de, Macêdo JAB de (2005) Parâmetros Físico-Químicos De Caracterização Da Contaminação Do Lençol Freático Por Necrochorume. Semin. Gestão Ambient. – Um convite a Interdiscip. Inst. Vianna Júnior – 31/05 a 04/06/2005 1–12
Andersson G, Heby O (1972) Polyamine and nucleic acid concentrations in Ehrlich ascites carcinoma cells and liver of tumor-bearing mice at various stages of tumor growth. JNCI J Natl Cancer Inst 48:165–172. https://doi.org/10.1093/jnci/48.1.165
Anjos 2013: Anjos RM (2013) Cemitérios: uma ameaça à saúde humana? http://www.crea-sc.org.br/portal/index.php?cmd=artigos-detalhe&id=2635#.YW823xrMLIU. Accessed 13 May 2017
Antonio AS, De Da Costa LCA, Paula ARU, Aguiar ATC, Keppler RLF, Bentes KRS, Wiedemann LSM (2018) Evaluation of soil chemical properties during cadaveric decomposition and its applications to forensic chemistry. Rev Virtual Quim 10:574–599. https://doi.org/10.21577/1984-6835.20180043
ARPEN (2021) Associação Nacional dos Registradores de Pessoas Naturais do Brasil - Portal da Transparência [WWW Document]. https://transparencia.registrocivil.org.br/especial-covid. Accessed 28 Sep 2020
Aruomero AS, Afolabi O (2014) Comparative assessment of trace metals in soils associated with casket burials: towards implementing green burials. Eurasian J Soil Sci 3:65. https://doi.org/10.18393/ejss.66428
Bach B, Le Quere S, Vuchot P, Grinbaum M, Barnavon L (2012) Validation of a method for the analysis of biogenic amines: histamine instability during wine sample storage. Anal Chim Acta 732:114–119. https://doi.org/10.1016/j.aca.2011.12.036
Bachrach U (2004) Polyamines and cancer: Minireview article. Amino Acids 26:307–309. https://doi.org/10.1007/s00726-004-0076-6
Bianchi J, Espindola ELG, Marin-Morales MA (2011) Genotoxicity and mutagenicity of water samples from the Monjolinho River (Brazil) after receiving untreated effluents. Ecotoxicol Environ Saf 74:826–833. https://doi.org/10.1016/j.ecoenv.2010.11.006
Bloomfield VA, Wilson RW (1981) Polyamines in Medicine and Biology. Marcel Dekker, New York
Boekema BKHL, Boekestijn B, Breederveld RS (2015) Evaluation of saline, RPMI and DMEM/F12 for storage of split-thickness skin grafts. Burns 41:848–852. https://doi.org/10.1016/j.burns.2014.10.016
Bornemissza G (1957) An analysis of Arthropod succession in Carrion and the effect of its decomposiion on the soil fauna. Aust J Zool 5:1–12. https://doi.org/10.1071/ZO9570001
BRASIL (2020) Dead body management in the context of coronavirus disease Sars-CoV-2 (Covid-19), 1st edn. Ministério da Saúde, Brasília/DF. http://bvsms.saude.gov.br/bvs/publicacoes/manejo_corpos_coronavirus_covid19.pdf. Accessed 14 Jul 2020
Brysont K, Greenall RJ (2000) Binding sites of the polyamines putrescine, cadaverine, spermidine and spermine on A- and B-DNA located by simulated annealing. J Biomol Struct Dyn 18:393–412. https://doi.org/10.1080/07391102.2000.10506676
Całkosiński I, Płoneczka-Janeczko K, Ostapska M, Dudek K, Gamian A, Rypuła K (2015) Microbiological analysis of necrosols collected from urban cemeteries in Poland. Biomed Res Int Hindawi 2015:1–7. https://doi.org/10.1155/2015/169573
Calmon M (2020) Considerations of coronavirus (COVID-19) impact and the management of the dead in Brazil. Forensic Sci. Int. Reports 100110. https://doi.org/10.1016/j.fsir.2020.100110. [WWW Document]. URL https://www.sciencedirect.com/science/article/pii/S2665910720300591?via%3Dihub. Accessed 05 Mar 21
Campos APS (2007) Avaliação do potencial de poluição no solo e nas águas subterrâneas decorrente da atividade cemiterial. Dissertação, Universidade de São Paulo
Carneiro VS (2008) Impactos causados por necrochorume de cemitérios: meio ambiente e saúde pública. Águas Subterrâneas 1: 1–18
CarodArtal FJ (2020) Complicaciones neurológicas por coronavirus y COVID-19. Rev Neurol 70: 311. https://doi.org/10.33588/rn.7009.2020179
Carter DO, Tibbett M (2008) Cadaver decomposition and soil: process. Soil Analysis in Forensic Taphonomy: Chemicas and Biological Effects of Buried Human Remains. CRC Press, Boca Raton, pp 29–52
Chen J, Rong X, Fan G, Li S, Li Q (2015) Effects of different concentrations of putrescine on proliferation, migration and apoptosis of human skin fibroblasts. NanFang Yi Ke Da XueXueBao 35:758–762. https://doi.org/10.3969/j.issn.1673-4254.2015.05.27
Christensen AM, Passalacqua NV, Bartelink EJ (2014) Forensic Anthropology: Current Methods and Practice, 1a edn. Acadeic Press, Amsterdam
CNN (2021) Covid-19: Variante de Manaus já está em pelo menos 12 estados brasileiros, https://www.cnnbrasil.com.br/saude/2021/02/16/covid-19-variante-de-manaus-ja-esta-em-pelo-menos-12-estados-brasileiros. Accessed 1 May 2021
Cordner S, Coninx R, Kim H-J et al (2016) Gestão de cadáveres após desastres: Manual para as equipes de primeira resposta no terreno, 2nd edn. OPAS, Washington
da Kemerich PD, C, Bianchini DC, Fank JC, et al (2014) A questão ambiental envolvendo os cemitérios no Brasil. Rev Monogr Ambient 13:3777–3785. https://doi.org/10.5902/2236130814506
Dalmora AC, Ramos CG, Oliveira MLS, Oliveira LFS, Schneider IAH, Kautzmann, RM (2020) Application of andesite rock as a clean source of fertilizer for eucalyptus crop: evidence of sustainability. J Clean Prod 256:120432. https://doi.org/10.1016/j.jclepro.2020.120432
D24AM - Rede Diário de Comunicação (2020) Manaus tem índice de sepultamentos em junho semelhante a período anterior à pandemia. https://d24am.com/amazonas/manaus-tem-indice-de-sepultamentos-emjunho-semelhante-a-periodo-anterior-a-pandemia/. Accessed 3 Jul 2020
De Mey E, De Klerck K, De Maere H, Dewulf L, Derdelinckx G, Peeters MC, Fraeye I, Vander Heyden Y, Paelinck H (2014) The occurrence of N-nitrosamines, residual nitrite and biogenic amines in commercial dry fermented sausages and evaluation of their occasional relation. MeatSci 96:821–828. https://doi.org/10.1016/j.meatsci.2013.09.010
del Rio B, Redruello B, Linares DM, Ladero V, Ruas-Madiedo P, Fernandez M, Martin MC, Alvarez MA (2019) The biogenic amines putrescine and cadaverine show in vitro cytotoxicity at concentrations that can be found in foods. Sci Rep 9:1–7. https://doi.org/10.1038/s41598-018-36239-w
Dent BB, Forbes SL, Stuart BH (2004) Review of human decomposition processes in soil. Environ Geol 45:576–585. https://doi.org/10.1007/s00254-003-0913-z
Doğan B, Jebli MB, Shahzad K, Farooq TH, Shahzad U (2020) Investigating the effects of meteorological parameters on COVID-19: case study of New Jersey. United States Environ Res 191(110148):1–9. https://doi.org/10.1016/j.envres.2020.110148
Dourado PLR, da Rocha MP, Roveda LM, Junior JLR, Cândido LS, Cardoso CAL, Morales MAM, de Oliveira KMP, Grisolia AB (2017) Genotoxic and mutagenic effects of polluted surface water in the midwestern region of Brazil using animal and plant bioassays. Genet Mol Biol 40:123–133. https://doi.org/10.1590/1678-4685-GMB-2015-0223
El País, 2020. A crise do coronavírus - As últimas notícias sobre o coronavírus e a crise política no Brasil [WWW Document]. URL https://brasil.elpais.com/brasil/2020-07-13/ao-vivo-as-ultimas-noticias-sobre-o-coronavirus-e-a-crise-politica-no-brasil.html. Accessed 14 July 2020
Fagundes OS, Oliveira LCA, Yamashita OM, Silva IV, Carvalho MAC, Rodrigues DV (2020) The water crisis and its implications in Brazilian agribusiness: A bibliographic review. Sci Electron Arch 13:42. https://doi.org/10.36560/1312020801
Fareed Z, Iqbal N, Shahzad F et al (2020) Co-variance nexus between COVID-19 mortality, humidity, and air quality index in Wuhan, China: New insights from partial and multiple wavelet coherence. Air Qual Atmos Heal 13:673–682. https://doi.org/10.1007/s11869-020-00847-1
Faria NR, Claro MI, Candido D et al (2021) Genomic characterization of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings. [WWW Document]. URL https://virological.org/t/genomic-characterisation-of-an-emergent-sars-cov-2-lineage-in-manaus-preliminary-findings/586. Accessed 05 Mar 21
Finegan O, Fonseca S, Guyomarc’h P, Morcillo Mendez MD, Rodriguez Gonzalez J, Tidball-Binz M, Winter KA (2020) International Committee of the Red Cross (ICRC): general guidance for the management of the dead related to COVID-19. Forensic Sci Int Synerg 2:129–137. https://doi.org/10.1016/j.fsisyn.2020.03.007
Fineschi V, Aprile A, Aquila I, Arcangeli M, Asmundo A, Bacci M, Cingolani M, Cipolloni L, D’Errico S, de Casamassimi I, Di Mizio G, Di Paolo M, Focardi M, Frati P, Gabbrielli M, La Russa R, Maiese A, Manetti F, Martelloni M, Mazzeo E, Montana A, Neri M, Padovano M, Pinchi V, Pomara C, Ricci P, Salerno M, Santurro A, Scopetti M, Testi R, Turillazzi E, Vacchiano G, Crivelli F, Bonoldi E, Facchetti F, Nebuloni M, Sapino A (2020) Management of the corpse with suspect, probable or confirmed COVID-19 respiratory infection – Italian interim recommendations for personnel potentially exposed to material from corpses, including body fluids, in morgue structures and during autopsy practi. Pathologica 112:64–77. https://doi.org/10.32074/1591-951X-13-20
Fiocruz Pernambuco (2020) Estudo aponta maior aceleração da Covid-19 no Norte e Nordeste [WWW Document]. URL https://agencia.fiocruz.br/estudo-aponta-maior-aceleracao-da-covid-19-no-norte-e-nordeste. Accessed 14 July 2020
Fusi E, Baldi A, Cheli F, Rebucci R, Ayuso E, Sejrsen K, Purup S (2008) Effects of putrescine, cadaverine, spermine, spermidine and β-phenylethylamine on cultured bovine mammary epithelial cells. Ital J Anim Sci 7:131–140. https://doi.org/10.4081/ijas.2008.131
Garcia I (2020) Sepultamentos aumentam 300% em cemitério em Cuiabá; maioria de vítimas da Covid-19 [WWW Document]. TV Cent. América/G1. URL https://g1.globo.com/mt/mato-grosso/noticia/2020/07/02/sepultamentos-aumentam-300percent-em-cemiterio-em-cuiaba-maioria-sao-de-vitimas-da-covid-19.ghtml. Accessed 13 July 2020
Gerner EW, Meyskens FL (2004) Polyamines and cancer: Old molecules, new understanding. Nat Rev Cancer 4:781–792. https://doi.org/10.1038/nrc1454
Giampá CEQ, Gonçalves VG (2005) Orientações para a utilização de águas subterrâneas no Estado de São Paulo. J. Vis. Lang. Comput. [WWW Document]. https://sigrh.sp.gov.br/public/uploads/documents/9301/revista_aguas_subterraneas.pdf. Accessed 05 Mar 21
Gondal MA, Nasr MM, Ahmed MM, Yamani ZH, Alsalhi MS (2011) Detection of lead in paint samples synthesized locally using-laser-induced breakdown spectroscopy. J Environ Sci Heal - Part A Toxic/Hazardous Subst Environ Eng 46: 42–49. https://doi.org/10.1080/10934529.2011.526082. [WWW Document]. https://www.tandfonline.com/doi/abs/10.1080/10934529.2011.526082. Accessed 05 Mar 2021
Gundy PM, Gerba CP, Pepper IL (2009) Survival of Coronaviruses in Water and Wastewater. Food Environ Virol 1:10–14. https://doi.org/10.1007/s12560-008-9001-6
Hauptmann N, Grimsby J, Shih JC, Cadenas E (1996) The metabolism of tyramine by monoamine oxidase A/B causes oxidative damage to mitochondrial DNA. Arch Biochem Biophys 335:295–304. https://doi.org/10.1006/abbi.1996.0510
Hirel B, Watier E, Chesne C et al (1996) Culture and drug biotransformation capacity of adult human keratinocytes from post-mortem skin. Br J Dermatol 134:831–836. https://doi.org/10.1046/j.1365-2133.1996.113848.x
Hirose R, Ikegaya H, Naito Y, et al (2020) Survival of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Influenza Virus on Human Skin: Importance of Hand Hygiene in Coronavirus Disease 2019 (COVID-19). Clin Infect Dis ciaa1517. https://doi.org/10.1093/cid/ciaa151
Hussain SS, Ali M, Ahmad M, Siddique KHM (2011) Polyamines: Natural and engineered abiotic and biotic stress tolerance in plants. Biotechnol Adv 29:300–311. https://doi.org/10.1016/j.biotechadv.2011.01.003
Ioan BG, Manea C, Hanganu B, Statescu L, Solovastru LG, Manoilescu I (2017) The chemistry decomposition in human corpses. Rev Chim 68:1450–1454. https://doi.org/10.37358/rc.17.6.5672
Iqbal N, Fareed Z, Shahzad F, He X, Shahzad U, Lina M (2020) The nexus between COVID-19, temperature and exchange rate in Wuhan city: new findings from partial and multiple wavelet coherence. Sci Total Environ 729:138916. https://doi.org/10.1016/j.scitotenv.2020.138916
Jancewicz AL, Gibbs NM, Masson PH (2016) Cadaverine’s functional role in plant development and environmental response. Front Plant Sci 7:1–8. https://doi.org/10.3389/fpls.2016.00870
Jonker C, Olivier J (2012) Mineral contamination from cemetery soils: case study of Zandfontein Cemetery, South Africa. Int J Environ Res Public Health 9:511–520. https://doi.org/10.3390/ijerph9020511
Kandoli SJ, Alidadi H, Najafpoor AA, Mehrabpour M, Hosseinzadeh A, Momeni F (2019) Assessment of cemetery effects on groundwater quality using GIS. Desalin WaterTreat 168: 235–242. https://doi.org/10.5004/dwt.2019.24622. [WWW. Document]. https://www.deswater.com/DWT_abstracts/vol_168/168_2019_235.pdf. Accessed 05 Mar 2021
Kemerich PD da C, Borba WF de, Silva RF da, Barros G, Gerhardt AE, Flores CEB (2012) Valores anômalos de metais pesados em solo de cemitério (doi:https://doi.org/10.4136/ambi-agua.838). Ambient. e Agua - AnInterdiscip J Appl Sci 7: 140–156. https://doi.org/10.4136/ambi-agua.838
Křížek M, Pavlíček T, Vácha F (2002) Formation of selected biogenic amines in carp meat. J Sci Food Agric 82:1088–1093. https://doi.org/10.1002/jsfa.1154
Ladero V, Calles-Enriquez M, Fernandez M, Alvarez MA (2010) Toxicological Effects of Dietary Biogenic Amines. Curr Nutr Food Sci 6:145–156. https://doi.org/10.2174/157340110791233256
Łukaszuk C, Krajewska-Kułak E, Guzowski A, Kraszyńska B, Grassmann M, Dobrowolski R (2015) Analysis of the incidence of fungi in a crypt cemetery. J Air Waste Manag Assoc 65:1141–1147. https://doi.org/10.1080/10962247.2015.1068884
Lyons DE, Beery JT, Lyons SA, Taylor SL (1983) Cadaverine and aminoguanidine potentiate the uptake of histamine in vitro in perfused intestinal segments of rats. Toxicol Appl Pharmacol 70:445–458. https://doi.org/10.1016/0041-008X(83)90162-X
Madabhavi I, Sarkar M, Kadakol N (2020) CoviD-19: A review. Monaldi Arch Chest Dis 90:248–258. https://doi.org/10.4081/monaldi.2020.1298
Matos B, Pacheco A (2001) Avaliação da ocorrência e do transporte de microrganismos no aqüífero freático do cemitério de Vila Nova Cachoeirinha, município de São Paulo. Águas Subterrâneas 172. https://aguassubterraneas.abas.org/asubterraneas/article/view/22635
Matsumoto ST, Marin-Morales MA (2004) Mutagenic potential evaluation of the water of a river that receives tannery effluent using the Allium cepa test system. Cytologia (Tokyo) 69:399–408. https://doi.org/10.1508/cytologia.69.399
Medema G, Heijnen L, Elsinga G et al (2020) Presence of SARS-Coronavirus-2 RNA inSewage and Correlation with Reported COVID-19 Prevalence in the Early Stage of the Epidemic in the Netherlands. Environ Sci Technol Lett 7:511–516. https://doi.org/10.1021/acs.estlett.0c00357
Melo DBG, Tudor F, Bernardino VN (2010) Cemitérios Sustentáveis, in: Feira Tecnológica do Centro Paula Souza – FETEPS. Campinas
MSF – Medecins Sans Frontieres (2021) COVID-19 leaves Amazonas health system saturated, overloaded and struggling (Brazil) [WWW Document]. URL https://www.msf.org/coronavirus-covid-19-collapses-health-system-manaus-brazil. Accessed 22 Jan 2021
Naddeo V, Liu H (2020) Editorial Perspectives: 2019 novel coronavirus (SARS-CoV-2): What is its fate in urban water cycle and how can the water research community respond? Environ Sci Water Res Technol 6:1213–1216. https://doi.org/10.1039/d0ew90015j
Nascimento FL (2020) Cemitério X Novo Coronavírus: Impactos da COVID-19 na Saúde Pública e Coletiva dos Mortos e dos Vivos. Rev. UFRR, Boletim de Conjuntura 2(4):1–11
Neckel A, Costa C, Mario DN, Sabadin CES, Bodah ET (2017) Environmental damage and public health threat caused by cemeteries: A proposal of ideal cemeteries for the growing urban sprawl. Urbe 9:216–230. https://doi.org/10.1590/2175-3369.009.002.AO05
Nogueira C de OG, Costa Júnior JEV, Coimbra LAB (2013) Cemitérios E Seus Impactos Socioambientais No Brasil. Periódico Eletrônico Fórum Ambient. da Alta Paul 9 (11): 331–344. https://doi.org/10.17271/198008279112013681
Oliveira B, Quinteiro P, Caetano C, Nadais H, Arroja L, Ferreira da Silva E, Senos Matias M (2013) Burial grounds’ impact on groundwater and public health: An overview. Water Environ J 27:99–106. https://doi.org/10.1111/j.1747-6593.2012.00330.x
WHO W.H.O. (2021) COVID-19 Weekly Epidemiological Update. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20210127_weekly_epi_update_24.pdf. Accessed 20 Sep 2021
Ourives EM, Carvalho PDS, De Oliveira BM, Ferreira AM (2017) Analysis of Environmental Impact of Cemetery in the Town of Três Pontas - MG. Rev Bras Gestão Ambient 11(1):109–111
Pacheco A (2017) Meio Ambiente e Cemitérios. Editora Senac, São Paulo
Pacheco A, Matos BA (2000) Cemitérios e meio ambiente: critérios para a implantação e norma técnica.Rev. Tecnologias do Ambiente [S.l.] 7(33): 13–15
Paíga P, Delerue-Matos C (2016) Determination of pharmaceuticals in groundwater collected in five cemeteries’ areas (Portugal). Sci Total Environ 569–570:16–22. https://doi.org/10.1016/j.scitotenv.2016.06.090
Paik Jung H-Y, Bieldanes LF (1979) Effects of cadaverine on histamine transport and metabolism in isolated gut sections of the guinea-pig. Food Cosmet Toxicol 17:629–632. https://doi.org/10.1016/0015-6264(79)90123-8
Pegg AE (2013) Toxicity of polyamines and their metabolic products. Chem Res Toxicol 26:1782–1800. https://doi.org/10.1021/tx400316s
Pinheiro J (2006) Decay process of cadaver. In: Schmitt A, Cunha E, Pinheiro J (eds) Forensic Anthropology and Medicine. Humana Press, Totowa, pp 85–116
Prescott J, Bushmaker T, Fischer R, Miazgowicz K, Judson S, Munster VJ (2015) Postmortem stability of Ebola virus. Emerg Infect Dis 21:856–859. https://doi.org/10.3201/eid2105.150041
Qu G, Li X, Hu L, Jiang G (2020) An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19). Environ Sci Technol. https://doi.org/10.1021/acs.est.0c01102
Ramani D, De Bandt JP, Cynober L (2014) Aliphatic polyamines in physiology and diseases. Clin Nutr 33:14–22. https://doi.org/10.1016/j.clnu.2013.09.019
Rauscher-Gabernig E, Gabernig R, Brueller W, Grossgut R, Bauer F, Paulsen P (2012) Dietary exposure assessment of putrescine and cadaverine and derivation of tolerable levels in selected foods consumed in Austria. Eur Food Res Technol 235:209–220. https://doi.org/10.1007/s00217-012-1748-1
Rodríguez-Eugenio N, McLaughlin M, Pennock D (2018) Soil pollution: a hidden reality. FAO, Rome
Rodrigues L, Pacheco A (2003) Groundwater contamination from cemeteries cases of study. Environ 2010 Situat Perspect Eur Union 6(10): 1–6
Rodriguez W, Bass WM (1983) Insect activity and its relationship to decay rates of human cadavers in east Tennessee. J Forensic Sci 28:423–432
Rollemberg S, de Barros AN, de Lima JPM (2020) Avaliação da contaminação, sobrevivência e remoção do coronavírus em sistemas de tratamento de esgoto sanitário. Rev Tecnol 41:1–15. https://doi.org/10.5020/23180730.2020.10849
Roser M, Ritchile H, Ortiz-Ospina E, Hasell J (2021) Coronavirus Pandemic (COVID-19) [WWW Document]. Publ. online OurWorldInData.org. URL https://ourworldindata.org/coronavirus. Accessed 22 Jan 2021
Sarwar S, Shahzad K, Fareed Z, Shahzad U (2021) A study on the effects of meteorological and climatic factors on the COVID-19 spread in Canada during 2020. J Environ Health Sci Engineer. https://doi.org/10.1007/s40201-021-00707-9
Schuber F (1989) Influence of polyamines on membrane functions. Biochem J 260:1–10. https://doi.org/10.1042/bj2600001
Seetulsingh P, Kannangara CI, Richman P (2020) Undetectable SARS-CoV-2 in anasopharyngeal swab but persistent viral RNA from deep lung swabs: findings from an autopsy. BMJ Case Rep 13. https://doi.org/10.1136/bcr-2020-237446
Shalaby AR (1996) Significance of biogenic amines to food safety and human health. Food Res Int 29:675–690. https://doi.org/10.1016/S0963-9969(96)00066-X
Shahzad K, Shahzad U, Iqbal N, Shahzad F, Fareed Z (2020a) Effects of climatological parameters on the outbreak spread of COVID-19 in highly affected regions of Spain. Environ Sci Pollut Res 27(31):39657–39666. https://doi.org/10.1007/s11356-020-10551-3
Shahzad F, Shahzad U, Fareed Z, Iqbal N, Hashmi SH, Ahmad F (2020b) Asymmetric nexus between temperature and COVID-19 in the top ten affected provinces of China: a current application of quantile-on-quantile approach. Sci Total Environ 736:139115. https://doi.org/10.1016/j.scitotenv.2020.139115
Shakoor A, Chen X, Farooq TH, Shahzad U, Ashraf F, Rehman A, Sahar N, Yan W (2020) Fluctuations in environmental pollutants and air quality during the lockdown in the USA and China: two sides of COVID-19 pandemic. Air Qual Atmos Health 13:1335–1342. https://doi.org/10.1007/s11869-020-00888-6
Silva LM (1995) Os cemitérios na problemática ambiental. In: I Seminário Nacional "Cemitérios e Meio Ambiente.” SINCESP & ACEMBRA, São Paulo
Silva RBP da, Campos MCC, Silva LS, Filho EG. de B, Lima AFL de, Pinheiro EN, Cunha JM (2020) Concentration of heavy metals in soils under cemetery occupation in Amazonas, Brazil. SoilSediment Contam. An Int J 29: 192–208. https://doi.org/10.1080/15320383.2019.1696280 [WWW. Document]: https://www.tandfonline.com/doi/full/10.1080/15320383.2019.1696280. Accessed 03 05 21
Silva RW da C, Malagutti Filho W (2008) Cemitérios como áreas potencialmente contaminadas. Ver. Brazilian Journal of Environmental Sciences (Online), (09): 26–35. [WWW Document]. http://rbciamb.com.br/index.php/Publicacoes_RBCIAMB/article/view/423. Accessed 20.05.21
Singanayagam A, Patel M, Charlett A et al (2020) Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill. 25(32):2001483. https://doi.org/10.2807/1560-7917.ES.2020.25.32.2001483
Souza M, Botelho RA (1999) Métodos Artificiais De Tanatoconservação. Saúde, Ética & Justiça 4: 33–47. https://doi.org/10.11606/issn.2317-2770.v4i1-2p33-47 [WWW Document]. https://www.revistas.usp.br/sej/article/view/40826. Accessed 20.05.21
Spriggs CC, Harwood MC, Tsai B (2019) How non-enveloped viruses hijack host machineries to cause infection. In: Kielian M, Mettenleiter TC, Roossinck MJ (eds) Advances in Virus Research. Academic Press, pp 97–122
Teti D, Visalli M, McNair H (2002) Analysis of polyamines as markers of (patho)physiological conditions. J Chromatogr B 781:107–149. https://doi.org/10.1016/S1570-0232(02)00669-4
Thomas T, Thomas TJ (2001) Polyamines in cell growth and cell death: Molecular mechanisms and therapeutic applications. Cell Mol Life Sci 58:244–258. https://doi.org/10.1007/PL00000852
Til HP, Falke HE, Prinsen MK, Willems MI (1997) Acute and subacute toxicity of tyramine, spermidine, spermine, putrescine and cadaverine in rats. Food Chem Toxicol 35:337–348. https://doi.org/10.1016/S0278-6915(97)00121-X
Tormen AF, Tasso CA, Korf EP (2016) Estudo da contaminação de águas subterrâneas por cemitérios. Perspect Online Ciências Exatas e Eng 16: 50–57. https://doi.org/10.25242/885X6162016902
van Allemann S, Dippenaar MA, Olivier J (2019) A laboratory study of the leachate composition of selected metals in cemeteries (South Africa). Environ Earth Sci 78:1–9. https://doi.org/10.1007/s12665-019-8521-8
Vass A, Barshick S, Sega G, Caton J, Skeen J, Love J (2002) Decomposition chemistry of human remains: a new methodology for determining the postmortem interval. J Forensic Sci 47:542–553
van Doremalen N, Bushmaker T, Morris DH et al (2020) Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 382:1564–1567. https://doi.org/10.1056/nejmc200497
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA - J Am Med Assoc 323:1061–1069. https://doi.org/10.1001/jama.2020.1585
Wang Y, Wu X, Wang Y et al (2004) Low stability of nucleocapsid protein in SARS virus. Biochemistry 43:11103–11108. https://doi.org/10.1021/bi049194b
Westall F, Brack A (2018) The Importance of Water for Life. Space Sci Rev 214:1–23. https://doi.org/10.1007/s11214-018-0476-7
WHO, W.H.O (2020a) WHO Coronavirus Disease (COVID-19) Dashboard [WWW Document]. URL https://covid19.who.int. Accessed 7 Oct 2020
WHO, W.H.O (2020b) Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed [WWW Document]. URL https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2020.4. Accessed 6.19.20
Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, Yin H, Xiao Q, Tang Y, Qu X, Kuang L, Fang X, Mishra N, Lu J, Shan H, Jiang G, Huang X (2020) Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol 5:434–435. https://doi.org/10.1016/S2468-1253(20)30083-2
Zychowski J, Bryndal T (2015) Impact of cemeteries on groundwater contamination by bacteria and viruses - a review. J Water Health 13:285–301. https://doi.org/10.2166/wh.2014.119
Author information
Authors and Affiliations
Contributions
LRG was responsible for reviewing environmental contamination in cemeteries, but also for writing, editing, and translating the manuscript. MMR acted in the conceptualization and was the major collaborator to review the COVID-19 pandemic data and in writing the manuscript. APAB collaborated in reviewing and writing about cemetery leachate chemicals and contamination by pathogens. GSC and GBB were contributors in review and writing about contamination of soils, groundwater, and surface waters by cemeteries. LSG made the review about cadaverous decomposition processes, wrote this section, and corrected the manuscript layout. LRS contributed to review and writing about the toxicity of biogenic amines present in cemetery leachate. MAMM acted in the supervision, conceptualization, writing, and revision of the entire manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This contribution is a review and does not warrant an ethical statement.
Consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gonçalves, L.R., Roberto, M.M., Braga, A.P.A. et al. Another casualty of the SARS-CoV-2 pandemic—the environmental impact. Environ Sci Pollut Res 29, 1696–1711 (2022). https://doi.org/10.1007/s11356-021-17098-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-17098-x