Abstract
Background
The viscoelastic properties of aortic tissue dictate vessel behavior in certain disease states, injury modalities, and during some endovascular procedures.
Objective
We characterized the viscoelastic response of porcine abdominal aortic tissue via test and simulation to demonstrate the utility of a viscoelastic anisotropic (VA) constitutive model.
Methods
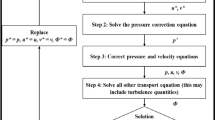
In this study, the measured stress relaxation response for five samples and uniaxial tensile testing for one sample measured with the digital image correlation (DIC) technique were used to identify material parameters for the VA model using an inverse method through finite element analysis (FEA).
Results
Based on the stress relaxation test, the values of the stress-like parameter \(\mu\), relative stiffness of the fibers \({k}_{1}\), dimensionless parameter \({k}_{2}\), angle of fibers \(\gamma\), dispersion parameter \(\kappa\), relaxation times for the ground matrix \({\mathsf{T}}_{g1}\) and collagen fibers \({\mathsf{T}}_{f1}\) and the dimensionless parameters for the ground matrix \({\beta }_{g1}\) and collagen fibers \({\beta }_{f1}\) for 0 degree specimen orientation were 12.1 ± 8.96 kPa, 77.3 ± 46.4 kPa, 0.032 ± 0.043, 30.25 ± 6.81°, 0.19 ± 0.06, 0.028 ± 0.016 s, 92.76 ± 26.51 s, 3.46 ± 3.78, 0.24 ± 0.08 and for 90 degree specimen orientation were 13.7 ± 7.7 kPa, 72.6 ± 35.4 kPa, 2.18 ± 4.12, 55.35 ± 7.12°, 0.22 ± 0.06, 23.51 ± 38.90 s, 81.52 ± 29.16 s, 5.14 ± 8.72, 0.21 ± 0.05, respectively. The validation revealed an overall good agreement from cycles 2 and 3 based on uniaxial tensile tests and surface strains data from DIC measurements with the material parameters from inverse analysis using FEA for the response in cycle 1.
Conclusions
The identified material model and numerical simulations provide a comprehensive description of the viscoelastic behavior of the aortic wall tissue and a quantitative understanding of the spatial and directional variability underlying aortic tissue mechanical behavior.







Similar content being viewed by others
References
Salunke NV, Topoleski LDT, Humphrey JD, Mergner WJ (2001) Compressive stress-relaxation of human atherosclerotic plaque. J Biomed Mater Res 55(2):236–241
Antonova ML, Antonov PS, Marinov GR, Vlaskovska MV, Kasakov LN (2008) Viscoelastic characteristics of in vitro vital and devitalized rat aorta and human arterial prostheses. Ann Biomed Eng 36(6):947–957
Holzapfel GA, Gasser TC (2007) Computational stress-deformation analysis of arterial walls including high-pressure response. Int J Cardiol 116(1):78–85
Zareh M, Fradet G, Naser G, Mohammadi H (2015) Are two-dimensional images sufficient to assess the atherosclerotic plaque vulnerability: a viscoelastic and anisotropic finite element model. Cardiovasc Syst 3(1):3
Hemmasizadeh A, Autieri M, Darvish K (2012) Multilayer material properties of aorta determined from nanoindentation tests. J Mech Behav Biomed Mater 15:199–207
Screen HRC (2008) Investigating load relaxation mechanics in tendon. J Mech Behav Biomed Mater 1(1):51–58
Shen ZL, Kahn H, Ballarini R, Eppell SJ (2011) Viscoelastic properties of isolated collagen fibrils. Biophys J 100(12):3008–3015
Yang C, Huang X, Zheng J, Woodard PK, Tang D (2006) Quantifying vessel material properties using mri under pressure condition and mri-based fsi mechanical analysis for human atherosclerotic plaques. In: 2006 ASME International Mechanical Engineering Congress and Exposition, IMECE2006, November 5, 2006 - November 10, 2006. American Society of Mechanical Engineers (ASME), Chicago, IL, United States
Lei F, Szeri AZ (2007) Inverse analysis of constitutive models: Biological soft tissues. J Biomech 40(4):936–940
Barrett SR, Sutcliffe MP, Howarth S, Li ZY, Gillard JH (2009) Experimental measurement of the mechanical properties of carotid atherothrombotic plaque fibrous cap. J Biomech 42(11):1650–1655
Holzapfel GA, Gasser TC, Ogden RW (2000) A new constitutive framework for arterial wall mechanics and a comparative study of material models. J Elast 61(1):1–48
Holzapfel G (2003) Structural and Numerical Models for the (Visco)elastic Response of Arterial Walls with Residual Stresses. In: Holzapfel G, Ogden R (eds) Biomechanics of Soft Tissue in Cardiovascular Systems. Springer, Vienna, pp 109–184
Holzapfel GA (2000) Nonlinear Solid Mechanics: A Continuum Approach for Engineering. John Wiley & Sons, Chichester
Gasser TC, Ogden RW, Holzapfel GA (2006) Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J R Soc Interface 3(6):15–35
Holzapfel GA, Gasser TC (2001) A viscoelastic model for fiber-reinforced composites at finite strains: Continuum basis, computational aspects and applications. Comput Methods Appl Mech Eng 190(34):4379–4403
Weiss JA, Maker BN, Govindjee S (1996) Finite element implementation of incompressible, transversely isotropic hyperelasticity. Comput Methods Appl Mech Eng 135(1–2):107–128
Peña E, Calvo B, Martínez MA, Doblaré M (2007) An anisotropic visco-hyperelastic model for ligaments at finite strains. Formulation and computational aspects. Int J Solids Struct 44(3–4):760–778
Leng X, Zhou B, Deng X, Davis L, Lessner SM, Sutton MA, Shazly T (2018) Experimental and numerical studies of two arterial wall delamination modes. J Mech Behav Biomed Mater 77:321–330
Unterberger MJ, Schmoller KM, Wurm C, Bausch AR, Holzapfel GA (2013) Viscoelasticity of cross-linked actin networks: experimental tests, mechanical modeling and finite-element analysis. Acta Biomater 9(7):7343–7353
Xu B, Li H, Zhang Y (2013) Understanding the viscoelastic behavior of collagen matrices through relaxation time distribution spectrum. Biomatter 3(3):e24651
Twal W, Klatt S, Harikrishnan K, Gerges E, Cooley M, Trusk T, Zhou B, Gabr M, Shazly T Lessner, S, Markwald R, Argraves WS (2013) Cellularized Microcarriers as Adhesive Building Blocks for Fabrication of Tubular Tissue Constructs. Ann Biomed Eng 1–12
Shazly T, Rachev A, Lessner S, Argraves W, Ferdous J, Zhou B, Moreira A, Sutton M (2014) On the Uniaxial Ring Test of Tissue Engineered Constructs. Exp Mech 55(1):41–51
Prim DA, Zhou B, Hartstone-Rose A, Uline MJ, Shazly T, Eberth JF (2016) A mechanical argument for the differential performance of coronary artery grafts. J Mech Behav Biomed Mater 54:93–105
Leng X, Wang Y, Xu J, Jiang Y, Zhang X, Xiang J (2018) Numerical simulation of patient-specific endovascular stenting and coiling for intracranial aneurysm surgical planning. J Transl Med 16(1):208
Wang Y, Leng X, Zhou X, Li W, Siddiqui AH, Xiang J (2018) Hemodynamics in a Middle Cerebral Artery Aneurysm prior to its Growth and Fatal Rupture: a Case Study and a Review of the Literature. World Neurosurg
Sutton MA (2008) Digital image correlation for shape and deformation measurements. In: Sharpe WN (ed) Springer handbook of experimental solid mechanics. Springer, pp 565–600
Holzapfel GA, Gasser TC, Stadler M (2002) A structural model for the viscoelastic behavior of arterial walls: Continuum formulation and finite element analysis. Eur J Mech A Solids 21(3):441–463
Rajesh R (2000) Coupled Thermomechanical Analysis of Viscoelastic Dampers. State University of New York, Buffalo
ABAQUS (2013) Analysis user’s manual version 6.12. Dassault Systemes Corp
Zhou B, Ravindran S, Ferdous J, Kidane A, Sutton MA, Shazly T (2016) Using Digital Image Correlation to Characterize Local Strains on Vascular Tissue Specimens. J Vis Exp 107:e53625
International Digital Image Correlation Society, Jones EMC, Iadicola MA (eds) (2018) A Good practices guide for digital image correlation
Zhou B, Rachev A, Shazly T (2015) The biaxial active mechanical properties of the porcine primary renal artery. J Mech Behav Biomed Mater 48:28–37
Walsh MT, Cunnane EM, Mulvihill JJ, Akyildiz AC, Gijsen FJH, Holzapfel GA (2014) Uniaxial tensile testing approaches for characterisation of atherosclerotic plaques. J Biomech 47(4):793–804
Zhou B, Wolf L, Rachev A, Shazly T (2014) A structure-motivated model of the passive mechanical response of the primary porcine renal artery. J Mech Med Biol 14(03):1450033
Wang Y, Ning J, Johnson JA, Sutton MA, Lessner SM (2011) Development of a quantitative mechanical test of atherosclerotic plaque stability. J Biomech 44(13):2439–2445
Wang Y, Johnson JA, Spinale FG, Sutton MA, Lessner SM (2014) Quantitative Measurement of Dissection Resistance in Intimal and Medial Layers of Human Coronary Arteries. Exp Mech 54(4):677–683
Leng X, Chen X, Deng X, Sutton M, Lessner S (2015) Modeling of Experimental Atherosclerotic Plaque Delamination. Ann Biomed Eng 43(12):2838–2851
Leng X, Davis LA, Deng X, Sutton MA, Lessner SM (2016) Numerical modeling of experimental human fibrous cap delamination. J Mech Behav Biomed Mater 59:322–336
Mohan D, Melvin JW (1982) Failure properties of passive human aortic tissue. I-Uniaxial tension tests, Journal of Biomechanics 15(11):887–902
Craiem D, Rojo FJ, Atienza JM, Armentano RL, Guinea GV (2008) Fractional-order viscoelasticity applied to describe uniaxial stress relaxation of human arteries. Phys Med Biol 53(17):4543–4554
Zou Y, Zhang Y (2011) The orthotropic viscoelastic behavior of aortic elastin. Biomech Model Mechanobiol 10(5):613–625
Gupta HS, Seto J, Krauss S, Boesecke P, Screen HRC (2010) In situ multi-level analysis of viscoelastic deformation mechanisms in tendon collagen. J Struct Biol 169(2):183–191
Zhou B, Alshareef M, Prim D, Collins M, Kempner M, Hartstone-Rose A, Eberth JF, Rachev A, Shazly T (2016) The perivascular environment along the vertebral artery governs segment-specific structural and mechanical properties. Acta Biomater 45:286–295
Yang L, van der Werf KO, Dijkstra PJ, Feijen J, Bennink ML (2012) Micromechanical analysis of native and cross-linked collagen type I fibrils supports the existence of microfibrils. J Mech Behav Biomed Mater 6:148–158
Díaz C, Peña JA, Martínez MA, Peña E (2021) Unraveling the multilayer mechanical response of aorta using layer-specific residual stresses and experimental properties. J Mech Behav Biomed Mater 113:104070
Franchini G, Breslavsky ID, Holzapfel GA, Amabili M (2021) Viscoelastic characterization of human descending thoracic aortas under cyclic load. Acta Biomater 130:291–307
Peña JA, Martínez MA, Peña E (2019) Failure damage mechanical properties of thoracic and abdominal porcine aorta layers and related constitutive modeling: phenomenological and microstructural approach. Biomech Model Mechanobiol 18(6):1709–1730
Deplano V, Boufi M, Gariboldi V, Loundou AD, D’Journo XB, Cautela J, Djemli A, Alimi YS (2019) Mechanical characterisation of human ascending aorta dissection. J Biomech 94:138–146
Leng X, Zhou B, Deng X, Davis L, Sutton MA, Shazly T, Lessner SM (2018) Determination of Viscoelastic Properties of human Carotid Atherosclerotic Plaque by Inverse Boundary Value Analysis. IOP Conf Ser Mater Sci Eng 381
Jia Y, Argueta-Morales IR, Liu M, Bai Y, Divo E, Kassab AJ, DeCampli WM (2015) Experimental Study of Anisotropic Stress/Strain Relationships of the Piglet Great Vessels and Relevance to Pediatric Congenital Heart Disease. Ann Thorac Surg 99(4):1399–1407
Garcia-Herrera CM, Celentano DJ, Cruchaga MA, Rojo FJ, Atienza JM, Guinea GV, Goicolea JM (2012) Mechanical characterisation of the human thoracic descending aorta: experiments and modelling. Comput Methods Biomech Biomed Engin 15(2):185–193
Sommer G, Holzapfel GA (2012) 3D constitutive modeling of the biaxial mechanical response of intact and layer-dissected human carotid arteries. J Mech Behav Biomed Mater 5(1):116–128
Ahuja A, Noblet JN, Trudnowski T, Patel B, Krieger JF, Chambers S, Kassab GS (2018) Biomechanical Material Characterization of Stanford Type-B Dissected Porcine Aortas. Front Physiol 9:1317
Weisbecker H, Pierce DM, Regitnig P, Holzapfel GA (2012) Layer-specific damage experiments and modeling of human thoracic and abdominal aortas with non-atherosclerotic intimal thickening. J Mech Behav Biomed Mater 12:93–106
Holzapfel GA, Sommer G, Gasser CT, Regitnig P (2005) Determination of layer-specific mechanical properties of human coronary arteries with nonatherosclerotic intimal thickening and related constitutive modeling. Am J Physiol Heart Circ Physiol 289(5):H2048–H2058
Funding
The authors gratefully acknowledge the sponsorship of the National Natural Science Foundation of China (No.11802113), NSF (award # CMMI-1200358) and partial support by a SPARC Graduate Research Grant from the Office of the Vice President for Research at the University of South Carolina.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Xiaochang Leng and Suraj Ravindran. The first draft of the manuscript was written by Xiaochang Leng and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors confirm there are not conflict of interest associated with this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Verification of Viscoelastic Anisotropic (VA) Model
Appendix: Verification of Viscoelastic Anisotropic (VA) Model
The VA model is verified by comparing numerical and analytical results under the assumption that the material is under plane strain deformation. A unit-cubic model of fiber-reinforced material was implemented with two families of fibers distributed 47° with respect to the circumferential direction (Fig. 2(a)). The surfaces at the x-axis and z-axis are fixed along the x and z directions, respectively. The assumption of material incompressibility, implying that \({\uplambda }_{\mathrm{x}}{\uplambda }_{\mathrm{y}}{\uplambda }_{\mathrm{z}}=1\). When the cubic model was stretched along the x-axis with a stretch ratio \({\lambda }_{x}\), the deformation gradient was calculated as follows:
Substituting equation (9) into equation (21), the Cauchy stress was calculated,
For the volumetric component of the Cauchy stress tensor,
Since the surfaces perpendicular to the y-axis are traction free,
where \(p={\left({{\sigma }_{ }}_{g}^{\infty }+{{+\sigma }_{ }}_{f}^{\infty }+{\sigma }_{visf1 }+{\sigma }_{visg1 }\right)}_{m+1 (\mathrm{yy})}\).
With the material parameters of specimen #6–0 from Table 3, the comparison of Cauchy stresses in x direction between analytical and numerical results is shown in Fig. 8. The results show that the numerical predictions of stress vs. stretch ratio curves match the analytic outputs.
Rights and permissions
About this article
Cite this article
Leng, X., Deng, X., Ravindran, S. et al. Viscoelastic Behavior of Porcine Arterial Tissue: Experimental and Numerical Study. Exp Mech 62, 953–967 (2022). https://doi.org/10.1007/s11340-022-00852-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11340-022-00852-8