Abstract
Purpose
Many studies have shown that obstructive sleep apnea (OSA) is related to reduced left ventricular diastolic function. Continuous positive airway pressure (CPAP) is generally recognized as the preferred therapy for OSA. Yet, the effect of CPAP on left ventricular diastolic function in patients with OSA is inconclusive. In order to assess the influence of CPAP on left ventricular diastolic function in patients with OSA, we performed this meta-analysis of clinical experiments.
Methods
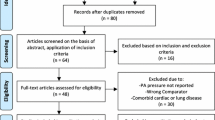
PubMed, Web of Science, OVID, Embase, and Cochrane Library from the establishment of the database to July 6, 2022, were searched for clinical trial data. Inclusion criteria for this meta-analysis were: (1) Patients in the experimental group were diagnosed with OSA by polysomnography; (2) CPAP treatment course ≥ 4 weeks; (3) baseline and follow-up data of the diastolic function parameter E/A ratio were reported in the literature. Exclusion criteria were: (1) Central sleep apnea (CSA); (2) comorbid organic heart diseases such as coronary heart disease; (3) age < 18 years old; (4) conference abstracts or duplicate publications.
Results
After exclusions, 7 studies (2 RCTs and 5 prospective studies) with 473 subjects (225 in the treatment group and 248 in the matched control group) were included in the meta-analysis. Subgroup analysis indicated that after CPAP therapy, the left ventricular (LV) E/A ratio was significantly increased in patients with OSA (weighted mean difference (WMD) = 0.22, 95% CI = − 0.06–0.38; P = 0.007). Sensitivity analyses showed that the combined results were not influenced by single studies. Publication bias was not significant (Egger’s test, P = 0.813).
Conclusions
The results of this meta-analysis suggest that CPAP may improve the E/A ratio in patients with OSA patients. However, the small number of studies (n = 7) decreases confidence in the findings. Thus, carefully designed randomized controlled trials are needed to confirm the findings.
Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
References
Patel SR (2019) Obstructive sleep apnea. Ann Intern Med 171:ITC81-ITC96. https://doi.org/10.7326/AITC201912030
Heinzer R et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318. https://doi.org/10.1016/s2213-2600(15)00043-0
Peppard PE et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. https://doi.org/10.1093/aje/kws342
Javaheri S et al (2017) Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 69:841–858. https://doi.org/10.1016/j.jacc.2016.11.069
Bauters FA et al (2019) Phenotype and risk burden of sleep apnea: a population-based cohort study. Hypertension 74:1052–1062. https://doi.org/10.1161/HYPERTENSIONAHA.119.13452
Akyol S et al (2016) Biventricular myocardial performance is impaired in proportion to severity of obstructive sleep apnea. Tex Heart Inst J 43:119–125. https://doi.org/10.14503/THIJ-14-4868
D’Andrea A et al (2020) Subclinical impairment of dynamic left ventricular systolic and diastolic function in patients with obstructive sleep apnea and preserved left ventricular ejection fraction. BMC Pulm Med 20:76. https://doi.org/10.1186/s12890-020-1099-9
Peker Y, Thunström E, Glantz H, Eulenburg C (2020) Effect of obstructive sleep apnea and CPAP treatment on cardiovascular outcomes in acute coronary syndrome in the RICCADSA trial. J Clin Med 9:1–12. https://doi.org/10.3390/jcm9124051
Yeghiazarians Y et al (2021) Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 144:e56–e67. https://doi.org/10.1161/CIR.0000000000000988
Silbiger JJ (2019) Pathophysiology and echocardiographic diagnosis of left ventricular diastolic dysfunction. J Am Soc Echocardiogr 32(216–232):212. https://doi.org/10.1016/j.echo.2018.11.011
Zile MR, Brutsaert DL (2002) New concepts in diastolic dysfunction and diastolic heart failure: part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 105:1387–1393. https://doi.org/10.1161/hc1102.105289
Bussoni MF et al (2014) Diastolic function and functional capacity after a single session of continuous positive airway pressure in patients with compensated heart failure. Clinics 69:354–359. https://doi.org/10.6061/clinics/2014(05)010
Bilge AR et al (2014) The effect of long-term continuous positive airway pressure treatment on systolic and diastolic function in patients with obstructive sleep apnoea syndrome: a five year observational study. Anatol J Cardiol 14:265–271. https://doi.org/10.5152/akd.2014.4870
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. Group, P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(264–269):W264. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Craig S et al (2015) Effect of CPAP on cardiac function in minimally symptomatic patients with OSA: results from a subset of the MOSAIC randomized trial. J Clin Sleep Med 11:967–973. https://doi.org/10.5664/jcsm.5004
Banares R et al (2002) Endoscopic treatment versus endoscopic plus pharmacologic treatment for acute variceal bleeding: a meta-analysis. Hepatology 35:609–615. https://doi.org/10.1053/jhep.2002.31354
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al (2008) The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2007. URL: http://www.ohrica/programs/clinicalepidemiology/oxford.htm
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Oliveira W et al (2009) Impact of continuous positive airway pressure treatment on left atrial volume and function in patients with obstructive sleep apnoea assessed by real-time three-dimensional echocardiography. Heart (British Cardiac Society) 95:1872–1878. https://doi.org/10.1136/hrt.2009.173625
ChunMei M, HuiLiang L, Wei H, JianPing L, DeJing J (2008) Effects of nasal continuous positive airway pressure on left ventricular structure and diastolic function in patients with obstructive sleep apnoea syndrome. J Fourth Military Med Univ 29:1593–1596
Li J-R et al (2018) Early cardiac injury in patients with obstructive sleep apnea Zhongguo ying yong sheng li xue za zhi = Zhongguo yingyong shenglixue zazhi. Chi J Appl Physiol 34:457–461. https://doi.org/10.12047/j.cjap.5707.2018.103
Butt M, Dwivedi G, Shantsila A, Khair OA, Lip GYH (2012) Left ventricular systolic and diastolic function in obstructive sleep apnea impact of continuous positive airway pressure therapy. CIRCULATION-HEART FAILURE 5:226–233. https://doi.org/10.1161/CIRCHEARTFAILURE.111.964106
Bayram NA et al (2009) Effects of continuous positive airway pressure therapy on left ventricular function assessed by tissue Doppler imaging in patients with obstructive sleep apnoea syndrome. Eur J Echocardiogr 10:376–382. https://doi.org/10.1093/ejechocard/jen257
Alchanatis M, Paradellis G, Pini H, Tourkohoriti G, Jordanoglou J (2000) Left ventricular function in patients with obstructive sleep apnoea syndrome before and after treatment with nasal continuous positive airway pressure. Respiration 67:367–371. https://doi.org/10.1159/000029532
Arias MA et al (2005) Obstructive sleep apnea syndrome affects left ventricular diastolic function - effects of nasal continuous positive airway pressure in men. Circulation 112:375–383. https://doi.org/10.1161/circulationaha.104.501841
Hammerstingl C et al (2013) Impact of untreated obstructive sleep apnea on left and right ventricular myocardial function and effects of CPAP therapy. PLoS One 8:76352. https://doi.org/10.1371/journal.pone.0076352
Johnson CB et al (2008) Acute and chronic effects of continuous positive airway pressure therapy on left ventricular systolic and diastolic function in patients with obstructive sleep apnea and congestive heart failure. Can J Cardiol 24:697–704. https://doi.org/10.1016/s0828-282x(08)70668-8
Oliveira W et al (2009) Impact of continuous positive airway pressure treatment on left atrial volume and function in patients with obstructive sleep apnoea assessed by real-time three-dimensional echocardiography. Heart 95:1872–1878. https://doi.org/10.1136/hrt.2009.173625
Yu L et al (2020) Left ventricular remodeling and dysfunction in obstructive sleep apnea : systematic review and meta-analysis. Herz 45:726–738. https://doi.org/10.1007/s00059-019-04850-w
Bradley TD, Hall MJ, Ando S, Floras JS (2001) Hemodynamic effects of simulated obstructive apneas in humans with and without heart failure. Chest 119:1827–1835. https://doi.org/10.1378/chest.119.6.1827
Castro-Grattoni AL et al (2016) Intermittent hypoxia-induced cardiovascular remodeling is reversed by normoxia in a mouse model of sleep apnea. Chest 149:1400–1408. https://doi.org/10.1016/j.chest.2015.11.010
Altekin RE et al (2012) Assessment of subclinical left ventricular dysfunction in obstructive sleep apnea patients with speckle tracking echocardiography. Int J Cardiovasc Imaging 28:1917–1930. https://doi.org/10.1007/s10554-012-0026-4
Korcarz,CE, Benca R, BarnetJH & Stein JH (2016) Treatment of obstructive sleep apnea in young and middle-aged adults: effects of positive airway pressure and compliance on arterial stiffness, endothelial function, and cardiac hemodynamics. J Am Heart Assoc 5. https://doi.org/10.1161/jaha.115.002930
Funding
YW provided financial support in the form of the National Key Research and Development Plan of China [20212BBG71004], the National Natural Science Foundation of China [82160085], the Beijing Health Promotion Association [20181BCB24013], special funds for guiding local scientific and technological development by the central government of China [S2019CXSFG0016], and the Natural science funding [20202BAB206005].
Author information
Authors and Affiliations
Contributions
JF and KL designed, performed, and wrote the meta-analysis. WL, FX, and ML took charge of the statistical analysis. YW revised the manuscript. All authors reviewed and agreed on this information before submission.
Corresponding author
Ethics declarations
Ethical approval
For this type of study, formal consent is not required.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feng, J., Li, K., Luo, W. et al. Effect of continuous positive pressure ventilation on left ventricular diastolic function E/A ratio in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath 27, 2333–2340 (2023). https://doi.org/10.1007/s11325-023-02836-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02836-x