Abstract
Purpose
Treatment of patients with obstructive sleep apnea (OSA) using mandibular advancement appliances enhances the airway and may be an alternative to continuous positive airway pressure (CPAP) in individuals with reduced adherence to CPAP therapy. The effectiveness as well as improved patient compliance associated with these appliances may improve the quality of life in patients with OSA. The aim of this systematic review of studies was to determine the improvement in quality of life amongst patients with OSA who were treated with an oral appliance.
Methods
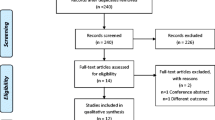
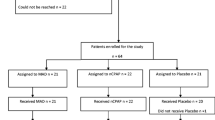
The research study was registered on the International Prospective Register of Systematic Reviews (PROSPERO: CRD42021193386). A search was carried out using the search engines Google Scholar, PubMed, Ovid, Cochrane Trial Registry, and LILACS. Patients with OSA treated with oral appliance therapy to advance the mandible were studied. Twenty-five studies were identified through the literature search and all had varying control groups for assessment of quality of life. Seventeen studies were included for the quantitative synthesis.
Results
QoL, evaluated by the Functional Outcomes of Sleep Questionnaire (FOSQ), significantly improved in patients treated with oral appliance therapy. There was a mean difference of 1.8 points between the baseline scores and the scores following treatment with an oral appliance.
Conclusion
Overall, a significant improvement in the QoL was observed with the Functional Outcomes of Sleep Questionnaire, following oral appliance therapy.



Similar content being viewed by others
References
Vanarsdall RL (1994) Orthodontics: current principles and techniques. CV Mosby
White DP, Younes MK (2012) Obstructive sleep apnoea, Comprehensive Physiology
Garvey JF, Pengo MF, Drakatos P, Kent BD (2015) Epidemiological aspects of obstructive sleep apnea. J Thorac Dis 7(5):920–929
Attanasio R, Bailey DR (2009) Dental management of sleep disorders. John Wiley & Sons
Rangarajan V (2019) Sleep-related disorders and its relevance in dental practice. Journal of Interdisciplinary Dentistry 9(2):49
Behrents RG, Shelgikar AV, Conley RS, Flores-Mir C, Hans M, Levine M, ..., Hittner J (2019). Obstructive sleep apnea and orthodontics: an American Association of Orthodontists White Paper. American Journal of Orthodontics and Dentofacial Orthopedics, 156(1), 13-28
Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R (2018) Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep and Breathing 22(3):555–568
Ferguson KA, Ono T, Lowe AA, Al-Majed S, Love LL, Fleetham JA (1997) A short-term controlled trial of an adjustable oral appliance for the treatment of mild to moderate obstructive sleep apnoea. Thorax 52(4):362–368
Johnston CD, Gleadhill IC, Cinnamond MJ, Gabbey J, Burden DJ (2002) Mandibular advancement appliances and obstructive sleep apnoea: a randomized clinical trial. The European Journal of Orthodontics 24(3):251–262
Cunningham SJ, O’Brien C (2007) Quality of life and orthodontics. In Seminars in Orthodontics (Vol. 13, No. 2, pp. 96–103). WB Saunders
World Health Organization. The world health organization quality of life (WHOQOL)-BREF. No. WHO/HIS/HSI Rev. 2012.02. World Health Organization, 2004
Moyer CA, Sonnad SS, Garetz SL, Helman JI, Chervin RD (2001) Quality of life in obstructive sleep apnea: a systematic review of the literature. Sleep Med 2(6):477–491
Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, Cistulli PA (2014) Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med 10(2):215–227
Kuhn E, Schwarz EI, Bratton DJ, Rossi VA, Kohler M (2017) Effects of CPAP and mandibular advancement devices on health-related quality of life in OSA: a systematic review and meta-analysis. Chest 151(4):786–794
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K, ..., Dinges DE (1997) An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep: 20(10): 835-843
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). Medical care 473:483
Flemons WW, Reimer MA (2002) Measurement properties of the Calgary sleep apnea quality of life index. Am J Respir Crit Care Med 165(2):159–164
ROBINS-I (2016) a tool for assessing risk of bias in non-randomized studies of interventions BMJ 355; i4919
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) BMJ 343:d5928
Engleman HM, McDonald JP, Graham D et al (2002) Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 166(6):855–859
Barnes M, McEvoy RD, Banks S, Tarquinio N, Murray CG, Vowles N, Pierce RJ (2004) Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med 170(6):656–664
Machado MAC, Prado LBFD, Carvalho LBCD, Francisco S, Silva ABD, Atallah ÁN, Prado GFD (2004) Quality of life of patients with obstructive sleep apnea syndrome treated with an intraoral mandibular repositioner. Arq Neuropsiquiatr 62(2a):222–225
Blanco J, Zamarron C, Pazos MA, Lamela C, Quintanilla DS (2005) Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. Sleep and Breathing 9(1):20–25
Lawton HM, Battagel JM, Kotecha B (2005) A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. The European Journal of Orthodontics 27(1):82–90
Johal A (2006) Health-related quality of life in patients with sleep-disordered breathing: effect of mandibular advancement appliances. J Prosthet Dent 96(4):298–302
Lam B, Sam K, Mok WY, Cheung MT, Fong DY, Lam JC, ..., Mary SM (2007) Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. Thorax 62(4): 354-359
Hoekema A, Stegenga B, Wijkstra PJ, Van der Hoeven JH, Meinesz AF, De Bont LG (2008 Sep) Obstructive sleep apnea therapy. J Dent Res 87(9):882–887
Petri N, Svanholt P, Solow B, Wildschiødtz G, Winkel P (2008) Mandibular advancement appliance for obstructive sleep apnoea: results of a randomised placebo controlled trial using parallel group design. J Sleep Res 17(2):221–229
Vecchierini MF, Leger D, Laaban JP, Putterman G, Figueredo M, Levy J, ..., Philip P (2008) Efficacy and compliance of mandibular repositioning device in obstructive sleep apnea syndrome under a patient-driven protocol of care. Sleep medicine 9(7): 762-769
Gauthier L, Laberge L, Beaudry M, Laforte M, Rompré PH, Lavigne GJ (2009) Efficacy of two mandibular advancement appliances in the management of snoring and mild-moderate sleep apnea: a cross-over randomized study. Sleep Med 10(3):329–336
Aarab G, Lobbezoo F, Hamburger HL, Naeije M (2011) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial. Respiration 81(5):411–419
Gauthier L, Laberge L, Beaudry M, Laforte M, Rompré PH, Lavigne GJ (2011) Mandibular advancement appliances remain effective in lowering respiratory disturbance index for 2.5–4.5 years. Sleep medicine 12(9):844–849
Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, Srinivasan VK, Yee BJ, ..., Cistulli PA (2013) Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. American journal of respiratory and critical care medicine 187(8): 879-887
Schütz TCB, Cunha TCA, Moura-Guimaraes T, Luz GP, Ackel-D'Elia C, Alves, EDS, ..., Bittencourt L (2013) Comparison of the effects of continuous positive airway pressure, oral appliance and exercise training in obstructive sleep apnea syndrome. Clinics 68: 1168-1174
Doff MH, Hoekema A, Wijkstra PJ, van der Hoeven JH, Huddleston Slater JJ, de Bont LG, Stegenga B (2013) Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: a 2-year follow-up. Sleep 36(9):1289–1296
Quinnell TG, Bennett M, Jordan J, Clutterbuck-James AL, Davies MG, Smith, IE, ..., Sharples LD (2014) A crossover randomised controlled trial of oral mandibular advancement devices for obstructive sleep apnoea-hypopnoea (TOMADO). Thorax, 69(10), 938-945
Banhiran W, Kittiphumwong P, Assanasen P, Chongkolwatana C, Metheetrairut C (2014) Adjustable thermoplastic mandibular advancement device for obstructive sleep apnea: outcomes and practicability. Laryngoscope 124(10):2427–2432
Marklund M, Carlberg B, Forsgren L, Olsson T, Stenlund H, Franklin KA (2015) Oral appliance therapy in patients with daytime sleepiness and snoring or mild to moderate sleep apnea: a randomized clinical trial. JAMA Intern Med 175(8):1278–1285
Bhushan A, Tripathi A, Gupta A, Tripathi S (2015) The effects of an oral appliance in obstructive sleep apnea patients with prehypertension. J Dent Sleep Med 2:37–43
Benoist L, de Ruiter M, de Lange J, de Vries N (2017) A randomized, controlled trial of positional therapy versus oral appliance therapy for position-dependent sleep apnea. Sleep Med 34:109–117
Gagnadoux F, Nguyen XL, Le Vaillant M, Priou P, Meslier N, Eberlein A, ..., Launois S (2017) Comparison of titrable thermoplastic versus custom-made mandibular advancement device for the treatment of obstructive sleep apnoea. Respiratory medicine 131: 35-42
Cunha TC, Guimaraes TD, Schultz TC, Almeida FR, Cunha TM, Simamoto Junior PC, Bittencourt LR (2017) Predictors of success for mandibular repositioning appliance in obstructive sleep apnea syndrome. Brazilian Oral Research 31
Fernández-Julián E, Pérez-Carbonell T, Marco R, Pellicer V, Rodriguez-Borja E, Marco J (2018) Impact of an oral appliance on obstructive sleep apnea severity, quality of life, and biomarkers. Laryngoscope 128(7):1720–1726
de Ruiter MH, Benoist LB, de Vries N, de Lange J (2018) Durability of treatment effects of the Sleep Position Trainer versus oral appliance therapy in positional OSA: 12-month follow-up of a randomized controlled trial. Sleep and Breathing 22(2):441–450
Ahrens A, McGrath C, Hägg U (2010) Subjective efficacy of oral appliance design features in the management of obstructive sleep apnea: a systematic review. Am J Orthod Dentofac Orthop 138(5):559–576
Vroegop AV, Vanderveken OM, Van de Heyning PH, Braem (MJ, (2012) Effects of vertical opening on pharyngeal dimensions in patients with obstructive sleep apnoea. Sleep Med 13(3):314–316
Pitsis AJ, Darendeliler MA, Gotsopoulos H, Petocz P, Cistulli PA (2002) Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med 166:860–864
Vanderveken OM, Devolder A, Marklund M, Boudewyns AN, Braem MJ, Okkerse W, Verbraecken JA, Franklin KA, De Backer WA, Van de Heyning PH (2008) Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med 178:197–202
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Comment
The measurement of quality of life (QoF) is an important aspect in the evaluation of oral appliance treatment for OSA, compared with CPAP, UPPP, and other treatments. This systematic review is more patient-centered and provides more valuable results for clinicians.
Yanyan Ma.
Beijing, China.
This article is part of the Topical Collection on Oral Appliance Therapy
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rangarajan, H., Padmanabhan, S., Ranganathan, S. et al. Impact of oral appliance therapy on quality of life (QoL) in patients with obstructive sleep apnea — a systematic review and meta-analysis. Sleep Breath 26, 983–996 (2022). https://doi.org/10.1007/s11325-021-02483-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02483-0