Abstract
Purpose
The definition of positional obstructive sleep apnea (POSA) is widely accepted as a difference of 50% or more in AHI between supine and non-supine position. Upper airway stimulation (UAS) is an effective treatment for OSA but the implant delivers a single voltage over sleep period without consideration of body position. Clinical practice suggests different outcomes for OSA in supine position under UAS treatment.
Methods
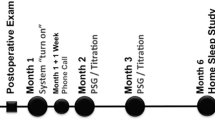
Outcomes of 44 patients were analyzed 12 months after implantation in a two-center, prospective consecutive trial in a university hospital setting. Total night and supine AHI were evaluated and the ratio of time spent in supine was considered. Correlation between the classic and the modified definition of POSA and treatment response were evaluated.
Results
The time ratio spent in supine position did not differ before implantation and after 12 months. Total and supine AHI were reduced with the use of UAS therapy (p < 0.001) but both the baseline and final supine AHI were higher than total night AHI. Considering POSA definition as a ratio of supine to non-supine AHI, there was no clear cutoff for defining responders neither with nor without the additional component of time in supine position.
Conclusions
The OSA reduction is strong for the total AHI and supine AHI. Nonetheless, here, there is no cutoff for defining POSA as critical for UAS therapy response. Therefore, there is no evidence for excluding POSA patients from UAS in general. Future technology improvement should take body position and adaptive voltage into account.
Similar content being viewed by others
References
Strollo PJ Jr, Soose RJ, Maurer JT, et al.; STAR Trial Group (2014) Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 370:139–149
Woodson BT, Soose RJ, Gillespie MB, et al.; STAR trial investigators (2016) Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg 154:181–188
Gillespie MB, Soose RJ, Woodson BT, et al.; STAR Trial Investigators (2017) Upper airway stimulation for obstructive sleep apnea: patient-reported outcomes after 48 months of follow-up. Otolaryngol Head Neck Surg 156:765–771
Strollo PJ, Soose R, Badr M, et al.; STAR trial investigators (2017) Upper airway stimulation for obstructive sleep apnea: objective and patient reported outcomes after five years of follow-up. SLEEP 40:Supplement A209
Heiser C, Thaler E, Boon M, Soose RJ, Woodson BT (2016) Updates of operative techniques for upper airway stimulation. Laryngoscope 126(Suppl 7):S12–S16
Heiser C, Hofauer B, Lozier L, Woodson BT, Stark T (2016) Nerve monitoring-guided selective hypoglossal nerve stimulation in obstructive sleep apnea patients. Laryngoscope 126:2852–2858
Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B (2017) Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol 274:1727–1734
Heiser C, Maurer JT, Hofauer B, Sommer UJ, Seitz A, Steffen A (2017) Outcomes of upper airway stimulation for obstructive sleep apnea in a multi-center German Post-Market Study. Otolaryngol Head Neck Surg 156:378–384
Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C (2017) Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope 128:509–515. https://doi.org/10.1002/lary.26688
Cartwright RD (1984) Effect of sleep position on sleep apnea severity. Sleep 7:110–114
Steffen A, Maibücher L, König IR (2017) Supine position and REM dependence in obstructive sleep apnea: Critical model considerations. HNO 65(Suppl 1):52–58
Iber C, Ancoli-Israel S, Chessonn A, Quan SF. AASM Manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007
Strollo PJ Jr, Gillespie MB, Soose RJ, et al.; Stimulation Therapy for Apnea Reduction (STAR) Trial Group (2015) Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep 38:1593–1598
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Ravesloot MJ, van Maanen JP, Dun L, de Vries N (2013) The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath 17:39–49
Galetke W, Anduleit N, Richter K, Stieglitz S, Randerath WJ (2008) Comparison of automatic and continuous positive airway pressure in a night-by-night analysis: a randomized, crossover study. Respiration 75:163–169
Prasad B, Usmani S, Steffen AD, van Dongen HPA, Pack FM, Strakovsky I, Staley B, Dinges D, Maislin G, Pack AI, Weaver TE (2016) Short-term variability in apnea-hypopnea index during extended home portable monitoring. J Clin Sleep Med 12:855–863
Levendowski DJ, Zack N, Rao S, Wong K, Gendreau M, Kranzler J, Zavora T, Westbrook PR (2009) Assessment of the test-retest reliability of laboratory polysomnography. Sleep Breath 13:163–167
Mjid M, Ouahchi Y, Toujani S et al (2016) Night-to-night variability of the obstructive sleep apnoea-hypopnoea syndrome. Rev Mal Respir 33:775–780
Logan MB, Branham GH, Eisenbeis JF, Hartse K (1996) 11: 48 AM: unattended home monitoring in the evaluation of sleep apnea: is it equal to formal polysomnograph? Otolaryngol Head Neck Surg 115:P156–P156
Metersky ML, Castriotta RJ (1996) The effect of polysomnography on sleep position: possible implications on the diagnosis of positional obstructive sleep apnea. Respiration 63:283–287
Bignold JJ, Mercer JD, Antic NA, McEvoy RD, Catcheside PG (2011) Accurate position monitoring and improved supine-dependent obstructive sleep apnea with a new position recording and supine avoidance device. J Clin Sleep Med 7:376–383
Acknowledgements
We wish to express our gratitude to Quan Ni, PhD, and Luke Lozier, Inspire Medical, for the consultative input on this study.
Funding
There was no external funding for this evaluation. Underlying data from German Post-market Study was furnished by Inspire Medical Systems, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Armin Steffen and Clemens Heiser are study investigators and received honoraria and travel expenses for invited talks on behalf of Inspire Medical, Inc., outside the submitted work. Benedikt Hofauer received travel expenses from Inspire Medical, Inc. Inke R. König and Julia Hartmann have nothing to declare. Madeline Ravesloot is a consultant for Nightbalance.
Informed consent
Informed consent was obtained for each patient. The study was approved by the local ethics committee (Ethikkommission, Universität zu Lübeck, Germany; Fakultät für Medizin, Ethikkommission, Technische Universität München, Germany) and is a sub-investigation of the German Post-market Study registered as NCT02293746 on clinicaltrials.gov.
Rights and permissions
About this article
Cite this article
Steffen, A., Hartmann, J.T., König, I.R. et al. Evaluation of body position in upper airway stimulation for obstructive sleep apnea—is continuous voltage sufficient enough?. Sleep Breath 22, 1207–1212 (2018). https://doi.org/10.1007/s11325-018-1716-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1716-5