Abstract
Purpose
Our objective was to investigate whether self-reported obstructive sleep apnea (OSA), simple snoring, and various markers of sleep-disordered breathing (SDB) are associated with cardiovascular risk.
Methods
We examined a representative nationwide cohort of 5177 Finnish adults aged ≥30 years. The participants underwent measurement of traditional cardiovascular risk factors and answered SDB-related questions derived from the Basic Nordic Sleep Questionnaire, which were used to operationalize self-reported OSA. The primary end point was incidence of a cardiovascular event (cardiovascular mortality, non-fatal myocardial infarction, non-fatal stroke, hospitalization for heart failure, or coronary interventions).
Results
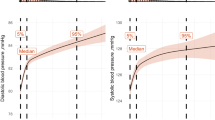
During a median follow-up of 11.2 years and 52,910 person-years of follow-up, 634 participants suffered a cardiovascular event. In multivariable-adjusted Cox models, self-reported OSA (hazard ratio [HR] 1.34; 95 % confidence interval [CI] 1.04–1.73; p = 0.03) was an independent predictor of cardiovascular events. Self-reported simple snoring by itself was not associated with future cardiovascular events (HR 0.88 versus non-snorers, 95 % CI 0.75–1.04, p = 0.15). However, among snorers (n = 3152), frequent breathing cessations (HR 2.19, 95 % CI 1.26–3.81, p = 0.006) and very loud and irregular snoring (HR 1.82, 95 % CI 1.31–2.54, p < 0.001) were associated with cardiovascular risk.
Conclusions
Self-reported OSA and SDB-related snoring variables are associated with cardiovascular risk, whereas simple snoring is not. In clinical practice and in surveys, questions concerning only habitual snoring should be amended with questions focusing on respiratory pauses and snoring stertorousness, which can be used to estimate the risk of OSA and cardiovascular events.


Similar content being viewed by others
References
Phillips CL, O’Driscoll DM (2013) Hypertension and obstructive sleep apnea. Nat Sci Sleep 5:43–52
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342:1378–1384
Lam JCM, Ip MSM (2007) An update on obstructive seep apnea and the metabolic syndrome. Curr Opin Pulm Med 13:484–489
Dong JY, Zhang YH, Qin LQ (2013) Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis 229:489–495
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041
Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, Diener-West M, Sanders MH, Wolf PA, Geraghty EM, Ali T, Lebowitz M, Punjabi NM (2010) Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med 182:269–277
Peker Y, Kraiczi H, Hedner J, Loth S, Johansson A, Bende M (1999) An independent association between obstructive sleep apnoea and coronary artery disease. Eur Resp J 14:179–184
Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto J, Stubbs R, Hla KM (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31:1071–1078
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O’Connor GT, Rapoport DM, Redline S, Resnick HE, Robbins JA, Shahar E, Unruh ML, Samet JM (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. doi:10.1371/journal.pmed.1000132
Marin JM, Carrizo SJ, Vicente E, Agusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Bearpark H, Elliott L, Grunstein R, Cullen S, Schneider H, Althaus W, Sullivan C (1995) Snoring and sleep apnea. A population study in Australian men. Am J Respir Crit Care Med 151:1459–1465
Marshall NS, Wong KKH, Cullen SRJ, Knuiman MW, Grunstein RR (2012) Snoring is not associated with all-cause mortality, incident cardiovascular disease, or stroke in the Busselton Health Study. Sleep 35:1235–1240
Knutson KL, Van Cauter E, Rathouz PJ, Yan LL, Hulley SB, Liu K, Lauderdale DS (2009) Association between sleep and blood pressure in midlife: the CARDIA sleep study. Arch Intern Med 169:1055–1061
Leineweber C, Kecklund G, Akerstedt T, Janszky I, Orth-Gomer K (2003) Snoring and the metabolic syndrome in women. Sleep Med 4:531–536
Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB (2002) Snoring as a risk factor for type II diabetes mellitus: a prospective study. Am J Epidemiol 155:387–393
Hu FB, Willett WC, Manson JAE, Colditz GA, Rimm EB, Speizer FE, Hennekens CH, Stampfer MJ (2000) Snoring and risk of cardiovascular disease in women. J Am Coll Cardiol 35:308–313
Koskenvuo M, Kaprio J, Telakivi T, Partinen M, Heikkilä K, Sarna S (1987) Snoring as a risk factor for ischaemic heart disease and stroke in men. Br Med J 294:16–19
Sands M, Loucks EB, Lu B, Carskadon MA, Sharkey K, Stefanick M, Ockene J, Shah N, Hairston KG, Robinson J, Limacher M, Hale L, Eaton CB (2013) Self-reported snoring and risk of cardiovascular disease among postmenopausal women (from the Women’s Health Initiative). Am J Cardiol 111:540–546
Davies DP, Rodgers H, Walshaw D, James OFW, Gibson GJ (2003) Snoring, daytime sleepiness and stroke: a case–control study of first-ever stroke. J Sleep Res 12:313–318
Marshall NS, Wong KKH, Cullen SRJ, Knuiman MW, Grunstein RR (2013) The burden of proof lies with the prosecution: is snoring guilty? Sleep 36:615
Kezirian EJ (2013) Snoring without OSA and health consequences: the jury is still out. Sleep 36:613
Rice TB (2012) Noise in the signal or bad vibrations? Sleep 35:1193–1194
Heistaro S (2008) Methodology report. Health 2000 Survey. National Public Health Institute, Helsinki
Partinen M, Gislason T (1995) Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res 4:150–155
Fogelholm M, Kronholm E, Kukkonen-Harjula K, Partonen T, Partinen M, Härmä M (2007) Sleep-related disturbances and physical inactivity are independently associated with obesity in adults. Int J Obes 31:1713–1721
Johansson JK, Kronholm E, Jula A (2011) Variability of home-measured blood pressure and heart rate: associations with self-reported insomnia and sleep duration. J Hypertens 29:1897–1905
International Classification of Sleep Disorders, 3rd ed. (2014) American Academy of Sleep Medicine, Chicago
Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Räiha P, Karja-Koskenkari PK, Mahonen M, Niemela M, Kuulasmaa K, Palomäki P, Mustonen J, Lehtonen A, Arstila M, Vuorenmaa T, Lehto S, Miettinen H, Torppa J, Tuomilehto J, Kesaniemi YA, Pyorälä K, Salomaa V (2005) The validity of the Finnish hospital discharge register and causes of death register data on coronary heart disease. Eur J Cardiovasc Prev Rehabil 12:132–137
Mähönen M, Jula A, Harald K, Antikainen R, Tuomilehto J, Zeller T, Blankenberg S, Salomaa V (2013) The validity of heart failure diagnoses obtained from administrative registers. Eur J Prev Cardiol 20:254–259
Tolonen H, Salomaa V, Torppa J, Sivenius J, Immonen-Räiha P, Lehtonen A (2007) The validation of the Finnish hospital discharge register and causes of death register data on stroke diagnoses. Eur J Cardiovasc Prev Rehabil 14:380–385
Zhang X, Loberiza FR, Klein JP, Zhang M-J (2007) A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput Methods Prog Biomed 88:95–101
Kasai T, Floras JS, Bradley TD (2012) Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation 126:1495–1510
Acknowledgments
The project organization created for the study involved the Finnish Centre for Pensions, the Social Insurance Institution, the National Public Health Institute, the Local Government Pensions Institution, the National Research and Development Centre for Welfare and Health, the Finnish Dental Society and the Finnish Dental Association, Statistics Finland, the Finnish Work Environment Fund, the Finnish Institute for Occupational Health, the UKK Institute for Health Promotion, the State Pensions Office, and the State Work Environment Fund.
Compliance with ethical standards
ᅟ
Ethical standards
All participants of the study gave their informed consent prior to inclusion in the study.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Teemu J. Niiranen and Erkki Kronholm contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Niiranen, T.J., Kronholm, E., Rissanen, H. et al. Self-reported obstructive sleep apnea, simple snoring, and various markers of sleep-disordered breathing as predictors of cardiovascular risk. Sleep Breath 20, 589–596 (2016). https://doi.org/10.1007/s11325-015-1253-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1253-4