Abstract
Purpose
The aim of this study is to determine parameters which influence 6-month compliance of continuous positive airway pressure therapy (CPAP) in patients with obstructive sleep apnea syndrome (OSAS).
Methods
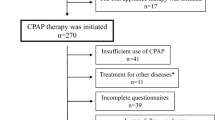
This prospective study investigated 73 patients (24 females) with OSAS and medical indication for CPAP therapy: age 55.1 ± 11.5 years, body mass index (BMI) 30.8 ± 5.0 kg/m2, Apnea–Hypopnea Index (AHI) 39.2 ± 26.7/h, Oxygen Desaturation Index (ODI) 33.2 ± 25.4/h, minimum O2 saturation 78.9 ± 7.6%. The influence of baseline parameters (demographic and polysomnographic data, sleeping medication intakes, BMI, psychometrics [Epworth Sleepiness Scale, Regensburg Insomnia Scale, Vigilance test and Beck Depression Inventory]) on 6-month compliance was evaluated with a correlation and a linear regression analysis.
Results
The baseline value of the Regensburg Insomnia Scale (RIS) predicts 6-month CPAP compliance (r = −0.376, R 2 = 0.14, p < 0.001), although no other baseline parameter correlates. Patients with a compliance of <4 h/night show higher RIS scores, i.e., more insomnia symptoms (17.6 ± 8.8) compared to those with ≥4 h/night (12.6 ± 6.9; p < 0.05).
Conclusions
Insomnia symptoms prior to the beginning of CPAP treatment show a negative influence on CPAP compliance. Further studies should clarify, if a treatment of insomnia symptoms leads to a benefit in compliance.


Similar content being viewed by others
References
American Academy of Sleep Medicine. International classification of sleep disorders (2005) Diagnostic and coding manual, 2nd edn. American Academy of sleep Medicine, Westchester
Shapiro GK, Shapiro CM (2010) Factors that influence CPAP adherence: an overview. Sleep Breath 14:323–335
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation scientific statement from the American Heart Association council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing. Circulation 52:686–717
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29:375–380
Deutsche Gesellschaft für Schlafforschung und Schlafmedizin (DGSM) (2009) S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen. Somnologie 13(Suppl 1):4–160
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, Kader G, Mahowald M, Younger J, Pack AI (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 30:711–719
Broström A, Nilsen P, Johansson P, Ulander M, Strömberg A, Svanborg E, Fridlund B (2010) Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: a qualitative content analysis. Sleep Med 11:126–130
Collard P, Pieters T, Aubert G, Delguste P, Rodenstein DO (1997) Compliance with nasal CPAP in obstructive sleep apnea patients. Sleep Med Rev 1:33–44
Alves C, Caminha JM, da Silva AM, Mendonça D (2011) Compliance to continuous positive airway pressure therapy in a group of Portuguese patients with obstructive sleep apnea syndrome. Sleep Breath. PMID: 21688210 2
Nguyên XL, Chaskalovic J, Rakotonanahary D, Fleury B (2010) Insomnia symptoms and CPAP compliance in OSAS patients: a descriptive study using data mining methods. Sleep Med 11:777–784
Yetkin O, Kunter E, Gunen H (2008) CPAP compliance in patients with obstructive sleep apnea syndrome. Sleep Breath 12:365–367
Sopkova Z, Dorkova Z, Tkacova R (2009) Predictors of compliance with continuous positive airway pressure treatment in patients with obstructive sleep apnea and metabolic syndrome. Wien Klin Wochenschr 121:398–404
de Zeeuw J, Baberg HT, Duchna HW, Kempkens DJ, Walther JW, Schultze-Werninghaus G, Rasche K, Orth M (2007) Locus of control belief is a predictor of CPAP-compliance in patients with obstructive sleep apnea syndrome. Pneumologie 61:283–290
Orth M, Kotterba S, Walther JW, Rasche K, Schultze-Werninghaus G, Duchna HW (2006) Long-term compliance of CPAP-therapy—update, predictors and interventions. Pneumologie 60:480–484
Jean Wiese H, Boethel C, Phillips B, Wilson JF, Peters J, Viggiano T (2005) CPAP compliance: video education may help! Sleep Med 6:171–174
Means MK, Edinger JD, Husain AM (2004) CPAP compliance in sleep apnea patients with and without laboratory CPAP titration. Sleep Breath 8:7–14
Ballard RD, Gay PC, Strollo PJ (2007) Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med 3:706–712
Aloia MS, Di Dio L, Ilniczky N, Perlis ML, Greenblatt DW, Giles DE (2001) Improving compliance with nasal CPAP and vigilance in older adults with OAHS. Sleep Breath 5:13–21
Kohler M, Smith D, Tippett V, Stradling JR (2010) Predictors of long-term compliance with continuous positive airway pressure. Thorax 65:829–832
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. Positive Airway Pressure Titration Task Force; American Academy of Sleep Medicine. J Clin Sleep Med 4:157–171
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15:376–381
Beck AT, Steer RA, Brown GK (1996) Manual for the Beck Depression Inventory – II. Psychological Corporation
Hautzinger M, Keller F, Kühner C (2006) Das Beck Depressionsinventar II. Deutsche Bearbeitung und Handbuch zum BDI II. Harcourt Test Services, Frankfurt
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Smith S, Sullivan K, Hopkins W, Douglas J (2004) Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med 5:449–456
Catcheside PG (2010) Predictors of continuous positive airway pressure adherence. F1000 Med Rep 2. pii: 70
Olsen S, Smith S, Oei T (2008) Adherence to continuous positive airway pressure therapy in obstructive sleep apnoea sufferers: a theoretical approach to treatment adherence and intervention. Clin Psych Rev 28:1355–1371
Edinger JD, Carwile S, Miller P, Hope V, Mayti C (1994) Psychological status, syndromatic measures, and compliance with nasal CPAP therapy for sleep apnea. Percept Mot Skills 78:1116–1128
Stepnowsky CJ, Marler MR, Palau J, Annette Brooks J (2006) Social–cognitive correlates of CPAP adherence in experienced users. Sleep Med 7:350–356
Poulet C, Veale D, Arnol N, Lévy P, Pepin JL, Tyrrell J (2009) Psychological variables as predictors of adherence to treatment by continuous positive airway pressure. Sleep Med 10:993–999
Engleman HM, Wild MR (2003) Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev 7:81–99
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pieh, C., Bach, M., Popp, R. et al. Insomnia symptoms influence CPAP compliance. Sleep Breath 17, 99–104 (2013). https://doi.org/10.1007/s11325-012-0655-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0655-9