Abstract
Background and Purpose
Sleep disordered breathing (SDB) is frequent in acute stroke patients and is associated with early neurologic worsening and poor outcome. Although continuous positive airway pressure (CPAP) effectively treats SDB, compliance is low. The objective of the present study was to assess the tolerance and the efficacy of a continuous high-flow-rate air administered through an open nasal cannula (transnasal insufflation, TNI), a less-intrusive method, to treat SDB in acute stroke patients.
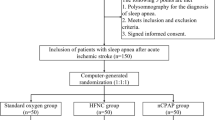
Methods
Ten patients (age, 56.8 ± 10.7 years), with SDB ranging from moderate to severe (apnea–hypopnea index, AHI, >15/h of sleep) and on a standard sleep study at a mean of 4.8 ± 3.7 days after ischemic stroke (range, 1–15 days), were selected. The night after, they underwent a second sleep study while receiving TNI (18 L/min).
Results
TNI was well tolerated by all patients. For the entire group, TNI decreased the AHI from 40.4 ± 25.7 to 30.8 ± 25.7/h (p = 0.001) and the oxygen desaturation index >3% from 40.7 ± 28.4 to 31 ± 22.5/h (p = 0.02). All participants except one showed a decrease in AHI. The percentage of slow-wave sleep significantly increased with TNI from 16.7 ± 8.2% to 22.3 ± 7.4% (p = 0.01). There was also a trend toward a reduction in markers of sleep disruption (number of awakenings, arousal index).
Conclusions
TNI improves SDB indices, and possibly sleep parameters, in stroke patients. Although these changes are modest, our findings suggest that TNI is a viable treatment alternative to CPAP in patients with SDB in the acute phase of ischemic stroke.

Similar content being viewed by others
Abbreviations
- SDB:
-
Sleep disordered breathing
- CPAP:
-
Continuous positive airway pressure
- TNI:
-
Transnasal insufflation
- AHI:
-
Apnea–hypopnea index
- CBFV:
-
Cerebral blood flow velocity
- PSG:
-
Polysomnography
- BL:
-
Baseline diagnostic night
- RERAs:
-
Respiratory effort-related arousals
- RDI:
-
Respiratory disturbance index
- ODI:
-
Oxygen desaturation indexes
- NIHSS:
-
National Institutes of Health Stroke Scale
- OAI:
-
Obstructive Apnea Index
- CAI:
-
Central Apnea Index
- MAI:
-
Mixed Apnea Index
- HI:
-
Hypopnea Index
References
Johnson KG, Johnson DC (2010) Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med 6:131–137
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373:82–93
Fisher M, Garcia JH (1996) Evolving stroke and the ischemic penumbra. Neurology 47:884–888
Iranzo A, Santamaria J, Berenguer J, Sanchez M, Chamorro A (2002) Prevalence and clinical importance of sleep apnea in the first night after cerebral infarction. Neurology 58:911–916
Kaneko Y, Hajek VE, Zivanovic V, Raboud J, Bradley TD (2003) Relationship of sleep apnea to functional capacity and length of hospitalization following stroke. Sleep 26:293–297
Sandberg O, Franklin KA, Bucht G, Gustafson Y (2001) Sleep apnea, delirium, depressed mood, cognition, and ADL ability after stroke. J Am Geriatr Soc 49:391–397
Hermann DM, Bassetti CL (2009) Sleep-related breathing and sleep-wake disturbances in ischemic stroke. Neurology 73:1313–1322
Dinges DF, Kribbs NB, Schwartz AR, Smith PL, Pack AI (1994) Objective measurement of nasal continuous positive airway pressure use: ethical considerations. Am J Respir Crit Care Med 149:291–292
McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ (1999) Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 159:1108–1114
Wessendorf TE, Wang YM, Thilmann AF, Sorgenfrei U, Konietzko N, Teschler H (2001) Treatment of obstructive sleep apnoea with nasal continuous positive airway pressure in stroke. Eur Respir J 18:623–629
Disler P, Hansford A, Skelton J, Wright P, Kerr J, O'Reilly J, Hepworth J, Middleton S, Sullivan C (2002) Diagnosis and treatment of obstructive sleep apnea in a stroke rehabilitation unit: a feasibility study. Am J Phys Med Rehabil 81:622–625
Sandberg O, Franklin KA, Bucht G, Eriksson S, Gustafson Y (2001) Nasal continuous positive airway pressure in stroke patients with sleep apnoea: a randomized treatment study. Eur Respir J 18:630–634
Hui DS, Choy DK, Wong LK, Ko FW, Li TS, Woo J, Kay R (2002) Prevalence of sleep-disordered breathing and continuous positive airway pressure compliance: results in Chinese patients with first-ever ischemic stroke. Chest 122:852–860
Broadley SA, Jorgensen L, Cheek A, Salonikis S, Taylor J, Thompson PD, Antic R (2007) Early investigation and treatment of obstructive sleep apnoea after acute stroke. J Clin Neurosci 14:328–333
Palombini L, Guilleminault C (2006) Stroke and treatment with nasal CPAP. Eur J Neurol 13:198–200
Scala R, Turkington PM, Wanklyn P, Bamford J, Elliott MW (2009) Acceptance, effectiveness and safety of continuous positive airway pressure in acute stroke: a pilot study. Respir Med 103:59–66
Martinez Garcia MA, Galiano Blancart R, Cabero Salt L, Soler Cataluna JJ, Escamilla T, Roman Sanchez P (2004) Prevalence of sleep-disordered breathing in patients with acute ischemic stroke: influence of onset time of stroke. Arch Bronconeumol 40:196–202
Hsu CY, Vennelle M, Li HY, Engleman HM, Dennis MS, Douglas NJ (2006) Sleep-disordered breathing after stroke: a randomised controlled trial of continuous positive airway pressure. J Neurol Neurosurg Psychiatry 77:1143–1149
Martinez-Garcia MA, Soler-Cataluna JJ, Ejarque-Martinez L, Soriano Y, Roman-Sanchez P, Illa FB, Canal JM, Duran-Cantolla J (2009) Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med 180:36–41
Teschler H, Stampa J, Ragette R, Konietzko N, Berthon-Jones M (1999) Effect of mouth leak on effectiveness of nasal bilevel ventilatory assistance and sleep architecture. Eur Respir J 14:1251–1257
Haring HP, Hormann C, Schalow S, Benzer A (1994) Continuous positive airway pressure breathing increases cerebral blood flow velocity in humans. Anesth Analg 79:883–885
Droste DW, Ludemann P, Anders F, Kemeny V, Thomas M, Krauss JK, Ringelstein EB (1999) Middle cerebral artery blood flow velocity, end-tidal pCO2 and blood pressure in patients with obstructive sleep apnea and in healthy subjects during continuous positive airway pressure breathing. Neurol Res 21:737–741
Bowie RA, O'Connor PJ, Hardman JG, Mahajan RP (2001) The effect of continuous positive airway pressure on cerebral blood flow velocity in awake volunteers. Anesth Analg 92:415–417
Scala R, Turkington PM, Wanklyn P, Bamford J, Elliott MW (2003) Effects of incremental levels of continuous positive airway pressure on cerebral blood flow velocity in healthy adult humans. Clin Sci (Lond) 104:633–639
McGinley BM, Patil SP, Kirkness JP, Smith PL, Schwartz AR, Schneider H (2007) A nasal cannula can be used to treat obstructive sleep apnea. Am J Respir Crit Care Med 176:194–200
Nilius G, Wessendorf T, Maurer J, Stoohs R, Patil SP, Schubert N, Schneider H (2010) Predictors for treating obstructive sleep apnea with an open nasal cannula system (transnasal insufflation). Chest 137:521–528
McGinley B, Halbower A, Schwartz AR, Smith PL, Patil SP, Schneider H (2009) Effect of a high-flow open nasal cannula system on obstructive sleep apnea in children. Pediatrics 124:179–188
Iber C, Ancoli-Israel S, Chesson A, Qaun SF (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
No authors listed (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force Sleep 22:667–689
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (1991) Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337:1521–1526
Werner C, Kochs E, Dietz R, Schulte am Esch J (1990) The effect of positive end expiratory pressure on the blood flow velocity in the basal cerebral arteries during general anesthesia. Anasth Intensivther Notfallmed 25:331–334
Hormann C, Mohsenipour I, Gottardis M, Benzer A (1994) Response of cerebrospinal fluid pressure to continuous positive airway pressure in volunteers. Anesth Analg 78:54–57
Feldman Z, Robertson CS, Contant CF, Gopinath SP, Grossman RG (1997) Positive end expiratory pressure reduces intracranial compliance in the rabbit. J Neurosurg Anesthesiol 9:175–179
Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O'Connor GT, Resnick HE, Diener-West M, Sanders MH, Wolf PA, Geraghty EM, Ali T, Lebowitz M, Punjabi NM (2010) Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med 182:269–277
Hayakawa T, Terashima M, Kayukawa Y, Ohta T, Okada T (1996) Changes in cerebral oxygenation and hemodynamics during obstructive sleep apneas. Chest 109:916–921
Valipour A, McGown AD, Makker H, O'Sullivan C, Spiro SG (2002) Some factors affecting cerebral tissue saturation during obstructive sleep apnoea. Eur Respir J 20:444–450
Guilleminault C, Connolly S, Winkle R, Melvin K, Tilkian A (1984) Cyclical variation of the heart rate in sleep apnoea syndrome. Mechanisms, and usefulness of 24 h electrocardiography as a screening technique. Lancet 1:126–131
Balfors EM, Franklin KA (1994) Impairment of cerebral perfusion during obstructive sleep apneas. Am J Respir Crit Care Med 150:1587–1591
Klingelhofer J, Hajak G, Sander D, Schulz-Varszegi M, Ruther E, Conrad B (1992) Assessment of intracranial hemodynamics in sleep apnea syndrome. Stroke 23:1427–1433
Stepnowsky CJ Jr, Orr WC, Davidson TM (2004) Nightly variability of sleep-disordered breathing measured over 3 nights. Otolaryngol Head Neck Surg 131:837–843
Acknowledgments
The authors thank Pr Hartmut Schneider for his helpful comments.
Disclosure statement
This is not an industry-supported study. The authors have no financial conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registration number
ACTRN12611000150943
Rights and permissions
About this article
Cite this article
Haba-Rubio, J., Andries, D., Rey, V. et al. Effect of transnasal insufflation on sleep disordered breathing in acute stroke: a preliminary study. Sleep Breath 16, 759–764 (2012). https://doi.org/10.1007/s11325-011-0572-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0572-3