Abstract
Objective
We assessed the socio-demographic correlates of snoring and also the patterns of health behaviour and co-morbidity associated with different types of snoring in the Hungarian population. We wanted to study whether different types of snoring are associated with high-risk health behaviour, chronic illnesses, daytime consequences of poor sleep, and with frequent accidents compared with non-snoring individuals.
Method
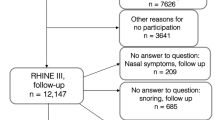
This is a cross-sectional study. Interviews were carried out in the homes of 12,643 people. This was the largest nationally representative study in Central Europe about health behaviour. In the Athens Insomnia Scale, questions about snoring and sleep behaviour, life-style factors and health behaviour, as well as questions on their history and current medical treatment were included in the questionnaire.
Results
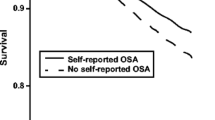
Thirty-seven percent of males and 21% of females reported loud snoring with breathing pauses. We found a significant increasing trend for the consumption of alcohol and coffee as well as smoking among non-snorers, habitual snorers and loud snorers, respectively. In an ordinal regression model male gender, the presence of smoking, the presence of three or more co-morbid conditions and alcohol consumption were independent predictors of snoring (OR [95% CI], 1.99 [1.85–2.1], 1.76 [1.60–1.92], 1.45 [1.30–1.62] and 1.22 [1.04–1.43], respectively, P < 0.001) after controlling for multiple socio-demographic and clinical variables. The frequency of accidents was higher in the loud snoring group than among non-snoring individuals (24% vs 17%, P < 0.0001).
Conclusions
Snoring is common in the Hungarian adult population. Snoring, especially loud snoring with breathing pauses, is strongly associated with high-risk health behaviour, higher co-morbidity and a higher frequency of accidents.

Similar content being viewed by others
References
Cirignotta F (2004) Classification and definition of respiratory disorders during sleep. Minerva Med 95:177–185
Young T, Finn L, Hla KM, Morgan B, Palta M (1996) Snoring as part of a dose–response relationship between sleep-disordered breathing and blood pressure. Sleep 19:S202–S205
Kauffmann F, Annesi I, Neukirch F, Oryszczyn MP, Alperovitch A (1989) The relation between snoring and smoking, body mass index, age, alcohol consumption and respiratory symptoms. Eur Respir J 2:599–603
Franklin KA, Gislason T, Omenaas E, Jogi R, Jensen EJ, Lindberg E, Gunnbjornsdottir M, Nystrom L, Laerum BN, Bjornsson E, Toren K, Janson C (2004) The influence of active and passive smoking on habitual snoring. Am J Respir Crit Care Med 170:799–803
Bearpark H, Elliott L, Grunstein R, Cullen S, Schneider H, Althaus W, Sullivan C (1995) Snoring and sleep apnea. A population study in Australian men. Am J Respir Crit Care Med 151:1459–1465
Ohayon MM, Guilleminault C, Priest RG, Caulet M (1997) Snoring and breathing pauses during sleep: telephone interview survey of a United Kingdom population sample. Bmj 314:860–863
Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR (2007) Epidemiology of insomnia: a longitudinal study in a UK population. Sleep 30:274–280
Chilcott LA, Shapiro CM (1996) The socioeconomic impact of insomnia. An overview. Pharmacoeconomics 10:1–14
Metlaine A, Leger D, Choudat D (2005) Socioeconomic impact of insomnia in working populations. Ind Health 43:11–19
Dunai A, Keszei AP, Kopp MS, Shapiro CM, Mucsi I, Novak M (2008) Cardiovascular disease and health-care utilization in snorers: a population survey. Sleep 31:411–416
Novak M, Mucsi I, Shapiro CM, Rethelyi J, Kopp MS (2004) Increased utilization of health services by insomniacs—an epidemiological perspective. J Psychosom Res 56:527–536
Conigrave KM, Hall WD, Saunders JB (1995) The AUDIT questionnaire: choosing a cut-off score. Alcohol Use Disorder Identification Test. Addiction 90:1349–1356
Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. (2004) Lancet. 363:157-63
Vamos EP, Kopp MS, Keszei A, Novak M, Mucsi I (2008) Prevalence of diabetes in a large, nationally representative population sample in Hungary. Diab Res Clin Pract 81:e5–e8
Molnar MZ, Novak M, Szeifert L, Ambrus C, Keszei A, Koczy A, Lindner A, Barotfi S, Szentkiralyi A, Remport A, Mucsi I (2007) Restless legs syndrome, insomnia, and quality of life after renal transplantation. J Psychosom Res 63:591–597
Soldatos CR, Dikeos DG, Paparrigopoulos TJ (2003) The diagnostic validity of the Athens Insomnia Scale. J Psychosom Res 55:263–267
Reda M, Ullal U, Wilson JA (2000) The quality of life impact of snoring and the effect of laser palatoplasty. Clin Otolaryngol Allied Sci 25:570–576
Janszky I, Lekander M, Blom M, Georgiades A, Ahnve S (2005) Self-rated health and vital exhaustion, but not depression, is related to inflammation in women with coronary heart disease. Brain Behav Immun 19:555–563
Zielinski J, Zgierska A, Polakowska M, Finn L, Kurjata P, Kupsc W, Young T (1999) Snoring and excessive daytime somnolence among Polish middle-aged adults. Eur Respir J 14:946–950
Teculescu D, Benamghar L, Hannhart B, Montaut-Verient B, Michaely JP (2007) Habitual snoring. Prevalence and risk factors in a sample of the French male population. Rev Mal Respir 24:281–287
Liu SA, Liu CY (2004) Prevalence of snoring in Taichung area: an epidemiological study. J Chin Med Assoc 67:32–36
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Khoo SM, Tan WC, Ng TP, Ho CH (2004) Risk factors associated with habitual snoring and sleep-disordered breathing in a multi-ethnic Asian population: a population-based study. Respir Med 98:557–566
Bloom JW, Kaltenborn WT, Quan SF (1988) Risk factors in a general population for snoring. Importance of cigarette smoking and obesity. Chest 93:678–683
Marchesini G, Pontiroli A, Salvioli G, Novi RF, Vitacolonna E, Taboga C, Ciccarone AM, Grossi E (2004) Snoring, hypertension and type 2 diabetes in obesity. Protection by physical activity. J Endocrinol Invest 27:150–157
Lavie P, Herer P, Lavie L (2007) Mortality risk factors in sleep apnoea: a matched case-control study. J Sleep Res 16:128–134
Jancso Z, Marton H, Simay A, Ujhelyi I, Ilyes I (2003) Cardiovascular risk among patients of general practices, who are not in current acute care. Orv Hetil 144:1433–1439
Lindberg E, Berne C, Franklin KA, Svensson M, Janson C (2007) Snoring and daytime sleepiness as risk factors for hypertension and diabetes in women—a population-based study. Respir Med 101:1283–1290
Tasali E, Mokhlesi B, Van Cauter E (2008) Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest 133:496–506
Angelico F, del Ben M, Augelletti T, de Vita R, Roma R, Violi F, Fabiani M (2010) Obstructive sleep apnoea syndrome and the metabolic syndrome in an internal medicine setting. Eur J Intern Med 21:191–195
Joo S, Lee S, Choi HA, Kim J, Kim E, Kimm K, Kim J, Shin C (2006) Habitual snoring is associated with elevated hemoglobin A1c levels in non-obese middle-aged adults. J Sleep Res 15:437–444
Steiropoulos P, Papanas N, Nena E, Maltezos E, Bouros D (2010) Continuous positive airway pressure treatment in patients with sleep apnoea: does it really improve glucose metabolism? Curr Diab Rev 6:156–166
Ohayon MM, Caulet M, Philip P, Guilleminault C, Priest RG (1997) How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med 157:2645–2652
Peppard PE, Szklo-Coxe M, Hla KM, Young T (2006) Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 166:1709–1715
Guilleminault C, Stoohs R, Duncan S (1991) Snoring (I). Daytime sleepiness in regular heavy snorers. Chest 99:40–48
Stradling JR, Crosby JH, Payne CD (1991) Self reported snoring and daytime sleepiness in men aged 35–65 years. Thorax 46:807–810
Lloberes P, Levy G, Descals C, Sampol G, Roca A, Sagales T, de la Calzada MD (2000) Self-reported sleepiness while driving as a risk factor for traffic accidents in patients with obstructive sleep apnoea syndrome and in non-apnoeic snorers. Respir Med 94:971–976
Young T, Blustein J, Finn L, Palta M, Young T, Blustein J, Finn L, Palta M (1997) Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep 20:608–613
Ekici M, Ekici A, Keles H, Akin A, Karlidag A, Tunckol M, Kocyigit P (2008) Risk factors and correlates of snoring and observed apnea. Sleep Med 9:290–296
Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M (2006) Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med 2:193–200
Lindberg E, Carter N, Gislason T, Janson C (2001) Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med 164:2031–2035
Lindberg E, Elmasry A, Janson C, Gislason T (2000) Reported snoring—does validity differ by age? J Sleep Res 9:197–200
Ulfberg J, Carter N, Talback M, Edling C (1996) Headache, snoring and sleep apnoea. J Neurol 243:621–625
Hoffstein V, Mateika S, Nash S (1996) Comparing perceptions and measurements of snoring. Sleep 19:783–789
Acknowledgements
The authors would like to thank the other members of the "Hungarostudy 2002" team (Csilla Csoboth, György Gyukits, Katalin Hajdú, János Lőke, Andrea Odor, János Réthelyi, Sándor Rózsa, Árpád Skrabski, Adrienne Stauder, András Székely, László Szűcs) for their work and to the network of community nurses for the home interviews, and for the National Population Register for the sample selection.
The research of M. Novak has been supported by an unrestricted research grant from Canadian Home Healthcare Inc.
Funding
This study was supported by the NKFP 1/002/2001 project, by the United Nation Development Program (UNDP), project No HUN/00/002/A/01/99, and the National Research Fund (OTKA) projects No: T-32974 (2000), TS-040889, T038409 (MN, IM) and the Foundation for Prevention in Medicine. This paper was supported by the János Bolyai Research Scholarship of the Hungarian Academy of Sciences (Marta Novak).
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torzsa, P., Keszei, A., Kalabay, L. et al. Socio-demographic characteristics, health behaviour, co-morbidity and accidents in snorers: a population survey. Sleep Breath 15, 809–818 (2011). https://doi.org/10.1007/s11325-010-0442-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0442-4