Abstract
Purpose
Many studies have been conducted to find the prevalence of obstructive sleep apnea (OSA) in Western countries. Limited data have been demonstrated in Asian countries; however, no such data have been reported in Thailand. The purpose of this study was to examine the prevalence of OSA and their related factors in Thai adults.
Methods
This study was performed in a university hospital in a rural area of central Thailand and data were collected. The population included office-based workers and people who came to contact with the hospital.
Results
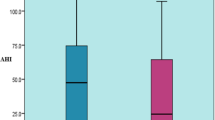
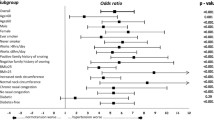
Among the total of 2,685 participants at the baseline examination, a random sample of 199 men and women was studied with employment of overnight full polysomnography to determine the prevalence of OSA and OSA syndrome (OSAS). The percentage of habitual snorers in the study population was 26.4%. The prevalence of OSA (apnea–hypopnea index 5) was 11.4%. When OSAS was defined by an apnea–hypopnea index 5 plus excessive daytime sleepiness, its prevalence was 4.4%. The prevalence of OSA and OSAS in men was 15.4% and 4.8% and in women was 6.3% and 1.9%, respectively. Logistic regression analyses showed that gender, body mass index, age, hypertension, alcohol consumption, and smoking were associated with the risk of OSA.
Conclusion
This study demonstrates that OSA is a common problem in the Thai adult population as in Western and other Asian countries. Understanding and treatment may be essential to reduce the risk of related medical problems.
Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Partinen M, Guilleminault C (1990) Daytime sleepiness and vascular morbidity at seven-year follow-up in obstructive sleep apnea patients. Chest 97:27–32
Kales A, Caldwell AB, Cadieux RJ, Vela-Bueno A, Ruch LG, Mayes SD (1985) Severe obstructive sleep apnea—II: associated psychopathology and psychosocial consequences. J Chronic Dis 38:427–434
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O’Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep-disordered breathing and cardiovascular disease: cross-sectional results of Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Gislason T, Almqvist M, Eriksson G, Taube A, Boman G (1988) Prevalence of sleep apnoea syndrome among Swedish men—an epidemiological study. J Clin Epidemiol 41:571–576
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, Kales A (2001) Prevalence of sleep disordered breathing in women: effects of gender. Am J Respir Crit Care Med 163:608–613
Cirignotta F, D’Alessandro R, Partinen M et al (1989) Prevalence of every night snoring and obstructive sleep apnoeas among 30–69-year-old men in Bologna, Italy. Acta Neurol Scand 79:366–372
Bearpark H, Elliott L, Grunstein R et al (1995) Snoring and sleep apnoea: a population study in Australian men. Am J Respir Crit Care Med 151:1459–1465
Ip MS, Lam B, Lauder IJ, Tsang KW, Chung KF, Mok YW, Lam WK (2001) A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest 119:62–69
Ip MS, Lam B, Tang LC, Lauder IJ, Ip TY, Lam WK (2004) A community study of sleep-disordered breathing in middle-aged Chinese women in Hong Kong: prevalence and gender differences. Chest 125:127–1234
Sharma SK, Kumpawat S, Banga A, Goel A (2006) Prevalence and risk factors of obstructive sleep apnoea syndrome in a population of Delhi, India. Chest 130:149–156
Udwadia ZF, Doshi AV, Lonkar SG, Singh CI (2004) Prevalence of sleep disordered breathing and sleep apnoea in middle-aged urban Indian men. Am J Respir Crit Care Med 169:168–173
Kim J, In K, Kim J, You S, Kang K, Shim J, Lee S, Lee J, Lee S, Park C, Shin C (2004) Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med 170:1108–1113
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 284:3015–3021
Newman AB, Foster G, Givelber R, Nieto FJ, Redline S, Young T (2005) Progression and regression of sleep-disordered breathing with changes in weight: the Sleep Heart Health Study. Arch Intern Med 165:2408–2413
Tishler PV, Larkin EK, Schluchter MD, Redline S (2003) Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep disordered breathing. JAMA 289:2230–2237
Schäfer H, Pauleit D, Sudhop T, Gouni-Berthold I, Ewig S, Berthold HK (2002) Body fat distribution, serum leptin, and cardiovascular risk factors in men with obstructive sleep apnea. Chest 122:829–839
Ancoli-Israel S, Klauber MR, Stepnowsky C, Estline E, Chinn A, Fell R (1995) Sleep-disordered breathing in the African-American elderly. Am J Respir Crit Care Med 152:1946–1949
Scanlan MF, Roebuck T, Little PJ, Redman JR, Naughton MT (2000) Effect of moderate alcohol upon obstructive sleep apnoea. Eur Respir J 16:909–913
Wetter DW, Young TB, Bidwell TR, Badr MS, Palta M (1994) Smoking as a risk factor for sleep disordered breathing. Arch Intern Med 154:2219–2224
Minami J, Ishimitsu T, Matsuoka H (1999) Effects of smoking cessation on blood pressure and heart rate variability in habitual smokers. Hypertension 33:586–590
Hauge T, Persson J, Sjolund K (2001) Neuropeptides in the duodenal mucosa of chronic alcoholic heavy drinkers. Alcohol Alcohol 36:213–218
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ (2003) The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA 289:2560–2572
International Diabetes Institute, World Health Organization (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia, Melbourne, pp 15–21
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. US Government Printing Office, Washington, DC
Iber C, Ancoli-Israel S, Chesson A, Quan S, for the American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Duran J, Esnaola S, Rubio R, Iztueta A (2001) Obstructive sleep apnea–hypopnea and related clinical features in a population-based sample of subjects aged 30–70 year. Am J Respir Crit Care Med 163:685–689
Block AJ, Boysen PG, Wynne JW, Hunt LA (1979) Sleep apnea, hypopnea and oxygen desaturation in normal subjects: a strong male predominance. N Engl J Med 300:513–517
Wilhoit SC, Suratt PM (1987) Obstructive sleep apnea in premenopausal women: a comparison with men and with postmenopausal women. Chest 91:654–658
Schmidt-Nowara WW, Coultas DB, Wiggins C, Skipper BE, Samet JM (1990) Snoring in a Hispanic-American population. Risk factors and association with hypertension and other morbidity. Arch Intern Med 150:597–601
Friedman M, Bliznikas D, Klein M, Duggal P, Somenek M, Joseph NJ (2006) Comparison of the incidences of sleep apnea–hypopnea syndrome in African-American vs Caucasian-Americans. Otolaryngol Head Neck Surg 134:545–550
Bresnitz EA, Goldberg R, Kosinski RM (1994) Epidemiology of obstructive sleep apnea. Epidemiol Rev 16:210–227
Anuntaseree W, Rookkapan K, Kuasirikul S, Thongsuksai P (2001) Snoring and obstructive sleep apnea in Thai school-age children: prevalence and predisposing factors. Pediatr Pulmonol 32:22–27
Resta O, Caratozzolo G, Pannacciulli N, Stefano A, Giliberti T, Carpagnano GE, De Pergola G (2003) Gender, age and menopause effects on the prevalence and the characteristics of obstructive sleep apnea in obesity. Eur J Clin Invest 33:1084–1089
Deegan PC, McNicholas WT (1996) Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J 9:117–124
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 157:144–148
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Campos-Rodriguez F, Pena-Grinan N, Reyes-Nunez N, De la Cruz-Moron I, Perez-Ronchel J, De la Vega-Gallardo F, Fernandez-Palacin A (2005) Mortality in obstructive sleep apnea hypopnea patients treated with positive airway pressure. Chest 128:624–633
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041
Young T, Peppard PE, Taheri S (2005) Excess weight and sleep-disordered breathing. J Appl Physiol 99:1592–1599
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Leiby BE, Vela-Bueno A, Kales A (2000) Association of hypertension and sleep-disordered breathing. Arch Intern Med 160:2289–2295
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study Sleep Heart Health Study. JAMA 283:1829–1836
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep disordered breathing and hypertension. N Engl J Med 342:1378–1384
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, Young T, Pickering TG (2005) Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 111:614–621
Jennum P, Hein HO, Suadicani P, Gyntelberg F (1992) Cardiovascular risk factors in snorers: a cross-sectional study of 3,323 men aged 54–74 years. The Copenhagen Male Study. Chest 102:1371–1376
Jennum P, Sjol A (1993) Snoring, sleep apnoea and cardiovascular risk factors: the MONICA II study. Int J Epidemiol 22:439–444
Bloom JW, Kaltenborn WT, Quan SF (1998) Risk factors in a general population for snoring: importance of cigarette smoking and obesity. Chest 93:678–683
Lindberg E, Taube A, Janson C, Gislason T, Swardsudd K, Boman G (1998) A 10-year follow-up of snoring in men. Chest 114:1048–1055
Pack AI, Cola MF, Goldszmidt A, Ogilvie MD, Gottschalk A (1992) Correlation between oscillations in ventilation and frequency content of the electroencephalogram. J Appl Physiol 72:985–992
Robinson RW, White DP, Zwillich CW (1985) Moderate alcohol ingestion increases upper airway resistance in normal subjects. Am Rev Respir Dis 132:1238–1241
Dolly FR, Block AJ (1983) Increased ventricular ectopy and sleep apnea following ethanol ingestion in COPD patients. Chest 83:469–472
Issa FG, Sullivan CE (1982) Alcohol, snoring and sleep apnea. J Neurol Neurosurg 45:353–359
Mitler MM, Dawson A, Henriksen SJ, Sobers M, Bloom FE (1988) Bedtime ethanol increases resistance of upper airways and produces sleep apneas in asymptomatic snorers. Alcohol Clin Exp Res 12:801–805
Berry RB, Desa MM, Light RW (1991) Effect of ethanol on the efficacy of nasal continuous positive airway pressure as a treatment for obstructive sleep apnea. Chest 99:339–343
Taasan VC, Block AJ, Boysen PG, Wynne JW (1981) Alcohol increases sleep apnea and oxygen desaturation in asymptomatic men. Am J Med 71:240–245
Acknowledgments
The authors would like to thank Dumnern Srinualta, MS for statistical analysis.
Financial disclosure
This study was supported in part by a grant no. SWUEC 189-2551 from the Faculty of Medicine, Srinakharinwirot University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neruntarat, C., Chantapant, S. Prevalence of sleep apnea in HRH Princess Maha Chakri Srinthorn Medical Center, Thailand. Sleep Breath 15, 641–648 (2011). https://doi.org/10.1007/s11325-010-0412-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0412-x