Abstract
Purpose
To analyze the associations between positron emission tomography (PET)/magnetic resonance imaging (MRI) features for primary rectal tumors and metastases.
Procedures
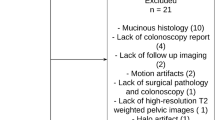
Between November 2016 and April 2018, 101 patients with rectal adenocarcinoma were included in this prospective study (NCT02537340) for whole-body PET/MRI for baseline staging. Two readers analyzed the PET/MRI; they assessed the semiquantitative PET features of the primary tumor and the N- and M-stages. Another reader analyzed the MRI features for locoregional staging. The reference standard for confirming metastatic disease was biopsy or imaging follow-up. Non-parametric tests were used to compare the PET/MRI features of the participants with or without metastatic disease. Binary logistic regression was used to evaluate the associations between the primary tumor PET/MRI features and metastatic disease.
Results
A total of 101 consecutive participants (median age 62 years; range: 33–87 years) were included. Metastases were detected in 35.6% (36 of 101) of the participants. Among the PET/MRI features, higher tumor lesion glycolysis (352.95 vs 242.70; P = .46) and metabolic tumor volume (36.15 vs 26.20; P = .03) were more frequent in patients with than in those without metastases. Additionally, patients with metastases had a higher incidence of PET-positive (64% vs 32%; P = .009) and MRI-positive (56% vs 32%; P = .03) mesorectal lymph nodes, extramural vascular invasion (86% vs 49%; P > .001), and involvement of mesorectal fascia (64% vs 42%; P = .04); there were also differences between the mrT stages of these two groups (P = .008). No differences in the maximum standardized uptake values for the primary tumors in patients with and without metastases were observed (18.9 vs 19.1; P = .56). Multivariable logistic regression showed that extramural vascular invasion on MRI was the only significant predictor (adjusted odds ratio, 3.8 [95% CI: 1.1, 13.9]; P = .001).
Conclusion
PET/MRI facilitated the identification of participants with a high risk of metastatic disease, though these findings were based mainly on MRI features.





Similar content being viewed by others
Change history
04 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11307-021-01696-9
References
Engstrom PF, Arnoletti JP, Iii ABB et al (2009) Rectal cancer. JNCCN J Natl Compr Cancer Netw 7:838–881
van de Velde CJH, Boelens PG, Borras JM et al (2014) EURECCA colorectal: multidisciplinary management: European consensus conference colon & rectum. Eur J Cancer 50:1.e1-1.e34. https://doi.org/10.1016/j.ejca.2013.06.048
Schmoll HJ, Van Cutsem E, Stein A et al (2012) ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol 23:2479–2516. https://doi.org/10.1093/annonc/mds236
Ozis SE, Soydal C, Akyol C et al (2014) The role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the primary staging of rectal cancer. World J Surg Oncol 12:26. https://doi.org/10.1186/1477-7819-12-26
Eglinton T, Luck A, Bartholomeusz D et al (2010) Positron-emission tomography/computed tomography (PET/CT) in the initial staging of primary rectal cancer. Colorectal Dis 12:667–673. https://doi.org/10.1111/j.1463-1318.2009.01873.x
Whaley JT, Fernandes AT, Sackmann R et al (2014) Clinical utility of integrated positron emission tomography/computed tomography imaging in the clinical management and radiation treatment planning of locally advanced rectal cancer. Pract Radiat Oncol 4:226–232. https://doi.org/10.1016/j.prro.2013.09.002
Jo HJ, Kim S-J, Kim IJ, Kim S (2014) Predictive value of volumetric parameters measured by F-18 FDG PET/CT for lymph node status in patients with surgically resected rectal cancer. Ann Nucl Med 28:196–202. https://doi.org/10.1007/s12149-014-0809-x
Li Q, Zheng R, Ling Y et al (2016) Prediction of tumor response after neoadjuvant chemoradiotherapy in rectal cancer using tomography – computed tomography and serum carcinoembryonic antigen: a prospective study. Abdom Radiol 41:1448–1455. https://doi.org/10.1007/s00261-016-0698-7
Jo HJ, Kim S-J, Lee HY, Kim IJ (2014) Prediction of survival and cancer recurrence using metabolic volumetric parameters measured by 18F-FDG PET/CT in patients with surgically resected rectal cancer. Clin Nucl Med 39:493–497. https://doi.org/10.1097/RLU.0000000000000438
Catalano OA, Lee SI, Parente C et al (2021) Improving staging of rectal cancer in the pelvis: the role of PET/MRI. Eur J Nucl Med Mol Imaging 48:1235–1245. https://doi.org/10.1007/s00259-020-05036-x
Rutegård MK, Båtsman M, Axelsson J et al (2019) PET/MRI and PET/CT hybrid imaging of rectal cancer - description and initial observations from the RECTOPET (REctal Cancer trial on PET/MRI/CT) study. Cancer Imaging 19(1):52. https://doi.org/10.1186/s40644-019-0237-1
Atkinson W, Catana C, Abramson JS et al (2016) Hybrid FDG-PET/MR compared to FDG-PET/CT in adult lymphoma patients. Abdom Radiol 41:1338–1348. https://doi.org/10.1007/s00261-016-0638-6
Queiroz MA, Ortega CD, Ferreira FR et al (2021) Diagnostic accuracy of FDG-PET/MRI versus pelvic MRI and thoracic and abdominal CT for detecting synchronous distant metastases in rectal cancer patients. Eur J Nucl Med Mol Imaging 48:186–195. https://doi.org/10.1007/s00259-020-04911-x
Furtado FS, Suarez-Weiss KE, Vangel M et al (2021) Clinical impact of PET/MRI in oligometastatic colorectal cancer. Br J Cancer 125:975–982. https://doi.org/10.1038/s41416-021-01494-8
Gaitanidis A, Alevizakos M, Tsaroucha A et al (2018) Predictive nomograms for synchronous distant metastasis in rectal cancer. J Gastrointest Surg 22:1268–1276. https://doi.org/10.1007/s11605-018-3767-0
Liu H, Cui Y, Shen W, et al (2016) Pretreatment magnetic resonance imaging of regional lymph nodes with carcinoembryonic antigen in prediction of synchronous distant metastasis in patients with rectal cancer. Oncotarget 7(19):27199–207. https://doi.org/10.18632/oncotarget.7979
Amorim BJ, Torrado-Carvajal A, Esfahani SA et al (2020) PET/MRI radiomics in rectal cancer: a pilot study on the correlation between PET- and MRI-derived image features with a clinical interpretation. Mol imaging Biol 22:1438–1445. https://doi.org/10.1007/s11307-020-01484-x
Smith NJ, Barbachano Y, Norman AR et al (2008) Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg 95:229–236. https://doi.org/10.1002/bjs.5917
Beets-Tan RGH, Lambregts DMJ, Maas M et al (2018) Magnetic resonance imaging for clinical management of rectal cancer: updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 28:1465–1475. https://doi.org/10.1007/s00330-017-5026-2
Brendle C, Schwenzer NF, Rempp H et al (2016) Assessment of metastatic colorectal cancer with hybrid imaging: comparison of reading performance using different combinations of anatomical and functional imaging techniques in PET/MRI and PET/CT in a short case series. Eur J Nucl Med Mol Imaging 43:123–132. https://doi.org/10.1007/s00259-015-3137-z
Kang B, Lee JM, Song YS et al (2016) Added value of integrated whole-body PET/MRI for evaluation of colorectal cancer: comparison with contrast-enhanced MDCT. Am J Roentgenol 206:W10–W20. https://doi.org/10.2214/AJR.14.13818
Tudyka V, Blomqvist L, Beets-Tan RGH et al (2014) EURECCA consensus conference highlights about colon & rectal cancer multidisciplinary management: the radiology experts review. Eur J Surg Oncol 40:469–475. https://doi.org/10.1016/j.ejso.2013.10.029
Dewhurst C, Rosen MP, Blake MA et al (2012) ACR appropriateness criteria pretreatment staging of colorectal cancer. J Am Coll Radiol 9:775–781. https://doi.org/10.1016/j.jacr.2012.07.025
Riihimaki M, Hemminki A, Sundquist J, Hemminki K (2016) Patterns of metastasis in colon and rectal cancer. Sci Rep 6:1–9. https://doi.org/10.1038/srep29765
Quadros CA, Falcão MF, Carvalho ME et al (2012) Metastases to retroperitoneal or lateral pelvic lymph nodes indicated unfavorable survival and high pelvic recurrence rates in a cohort of 102 patients with low rectal adenocarcinoma. J Surg Oncol 106:653–658. https://doi.org/10.1002/jso.23144
Hope TA, Kassam Z, Loening A et al (2019) The use of PET/MRI for imaging rectal cancer. Abdom Radiol (NY) 44(11):3559–3568. https://doi.org/10.1007/s00261-019-02089-x
Yoon JH, Lee JM, Chang W et al (2020) Initial M staging of rectal cancer: FDG PET/MRI with a hepatocyte-specific contrast agent versus contrast-enhanced CT. Radiology 294:310–319. https://doi.org/10.1148/radiol.2019190794
MERCURY Study Group (2006) Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ 333:779. https://doi.org/10.1136/bmj.38937.646400.55
Hunter CJ, Garant A, Vuong T et al (2012) Adverse features on rectal MRI identify a high-risk group that may benefit from more intensive preoperative staging and treatment. Ann Surg Oncol 19:1199–1205. https://doi.org/10.1245/s10434-011-2036-1
Chang GJ, You YN, Park IJ et al (2012) Pretreatment high-resolution rectal MRI and treatment response to neoadjuvant chemoradiation. Dis Colon Rectum 55:371–377. https://doi.org/10.1097/DCR.0b013e31824678e3
Taylor FGM, Quirke P, Heald RJ et al (2011) Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European study. Ann Surg 253:711–719. https://doi.org/10.1097/SLA.0b013e31820b8d52
Siddiqui MRS, Simillis C, Hunter C et al (2017) A meta-analysis comparing the risk of metastases in patients with rectal cancer and MRI-detected extramural vascular invasion (mrEMVI) vs mrEMVI-negative cases. Br J Cancer 116:1513–1519. https://doi.org/10.1038/bjc.2017.99
Kim H, Kim M-J, Kim NK et al (2014) MRI-detected extramural vascular invasion is an independent prognostic factor for synchronous metastasis in patients with rectal cancer. Eur Radiol 25:1347–1355. https://doi.org/10.1007/s00330-014-3527-9
Chand M, Evans J, Swift RI et al (2015) The prognostic significance of postchemoradiotherapy high-resolution MRI and histopathology detected extramural venous invasion in rectal cancer. Ann Surg 261:473–479. https://doi.org/10.1097/SLA.0000000000000848
Zhang X-Y, Wang S, Li X-T et al (2018) MRI of extramural venous invasion in locally advanced rectal cancer: relationship to tumor recurrence and overall survival. Radiology 289:677–685. https://doi.org/10.1148/radiol.2018172889
Liao CY, Chen SW, Wu YC et al (2014) Correlations between 18F-FDG PET/CT parameters and pathological findings in patients with rectal cancer. Clin Nucl Med 39:e40-5. https://doi.org/10.1097/RLU.0b013e318292f0f6
Dos Anjos DA, Perez RO, Habr-Gama A et al (2016) Semiquantitative volumetry by sequential PET/CT may improve prediction of complete response to neoadjuvant chemoradiation in patients with distal rectal cancer. Dis Colon Rectum 59:805–812. https://doi.org/10.1097/DCR.0000000000000655
Bundschuh RA, Dinges J, Neumann L et al (2014) Textural parameters of tumor heterogeneity in 18F-FDG PET/CT for therapy response assessment and prognosis in patients with locally advanced rectal cancer. J Nucl Med 55:891–897. https://doi.org/10.2967/jnumed.113.127340
Bazan JG, Koong AC, Kapp DS et al (2013) Metabolic tumor volume predicts disease progression and survival in patients with squamous cell carcinoma of the anal canal. J Nucl Med 54:27–32. https://doi.org/10.2967/jnumed.112.109470
Crimì F, Valeggia S, Baffoni L et al (2021) [18F]FDG PET/MRI in rectal cancer. Ann Nucl Med 35:281–290
Nensa F, Beiderwellen K, Heusch P, Wetter A (2014) Clinical applications of PET/MRI: current status and future perspectives. Diagn Interv Radiol 20:438–447. https://doi.org/10.5152/dir.2014.14008
Catalano OA, Coutinho AM, Sahani DV et al (2017) Colorectal cancer staging: comparison of whole-body PET/CT and PET/MR. Abdom Radiol 42:1141–1151. https://doi.org/10.1007/s00261-016-0985-3
Lee SJ, Seo HJ, Kang KW et al (2015) Clinical performance of whole-body 18F-FDG PET/Dixon-VIBE, T1-weighted, and T2-weighted MRI protocol in colorectal cancer. Clin Nucl Med 40:e392–e398. https://doi.org/10.1097/RLU.0000000000000812
Viglianti BL, Wale DJ, Wong KK et al (2018) Effects of tumor burden on reference tissue standardized uptake for PET imaging: modification of PERCIST criteria. Radiology 287:993–1002. https://doi.org/10.1148/radiol.2018171356
Ilyas H, Mikhaeel NG, Dunn JT et al (2018) Defining the optimal method for measuring baseline metabolic tumour volume in diffuse large B cell lymphoma. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-018-3953-z
Funding
GE Healthcare partially financed this study, covering the costs of the PET/MRI, including the dose of fluorine-18 deoxyglucose (18F-FDG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The institutional review board approved this prospective study, and all participants signed an informed consent form. This study is registered on clinicaltrials.gov with the identification number NCT02537340.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Queiroz, M.A., Ortega, C.D., Ferreira, F.R. et al. Value of Primary Rectal Tumor PET/MRI in the Prediction of Synchronic Metastatic Disease. Mol Imaging Biol 24, 453–463 (2022). https://doi.org/10.1007/s11307-021-01674-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-021-01674-1