Abstract
Purpose
The aim of this study was to evaluate the detection rate of [68Ga]prostate-specific membrane antigen ([68Ga]PSMA-11) positron emission tomography (PET)/magnetic resonance imaging (MRI) and to compare it with [68Ga]PSMA-11 PET/X-ray computed tomography (CT) in patients with recurrent prostate cancer (PC) after radical prostatectomy.
Procedures
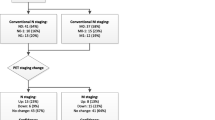
A total of 93 patients with biochemically recurrent prostate cancer underwent [68Ga]PSMA-11 PET/CT and subsequently a whole-body integrated PET/MRI examination. Board certified nuclear medicine physicians and radiologists evaluated PET/CT and PET/MRI datasets regarding identification of tumor lesions ((i) lymph nodes, (ii) bone lesions, (iii) local recurrence, and (iv) parenchymal lesions) based on maximum [68Ga]PSMA-11 uptake as well as morphological changes. Quality of PET images for both PET/CT and PET/MRI were rated using a 5-point scoring system by evaluating lesion homogeneity, contrast, contour, and delineation. Wilcoxon signed-rank tests were used to determine statistical differences.
Results
PC relapse was detected in 62/93 patients. PET/MRI detected 148 out of 150 lesions described in PET/CT. In addition, PET/MRI detected 11 lesions not detected in PET/CT (5 lymph nodes, 6 local recurrences). The exact McNemar statistical test (one-sided) showed significant difference between PET/CT and PET/MRI for diagnosis of local recurrence (p value = 0.031). Diagnostic confidence for (iii) was higher in PET/MRI compared with PET/CT (PET/CT = 1.1; PET/MRI = 4.9). Diagnostic confidence for (i) (PET/CT = 4.9; PET/MRI = 4.6), (ii) (PET/CT = 4.9; PET/MRI = 4.6), and (iv) (PET/CT = 4.6; PET/MRI = 4.8) was equivalent between PET/MRI and PET/CT.
Conclusions
Integrated [68Ga]PSMA-11 PET/MRI provides a similarly high diagnostic performance for localization of recurrent PC as PET/CT. For the detection of local recurrences [68Ga]PSMA-11 PET/MRI is superior compared with [68Ga]PSMA-11 PET/CT.



Similar content being viewed by others
References
Stephenson AJ, Scardino PT, Eastham JA, Bianco FJ Jr, Dotan ZA, Fearn PA, Kattan MW (2006) Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Natl Cancer Inst 98:715–717
Moul JW (2000) Prostate specific antigen only progression of prostate cancer. J Urol 163:1632–1642
Kupelian PA, Elshaikh M, Reddy CA, Zippe C, Klein EA (2002) Comparison of the efficacy of local therapies for localized prostate cancer in the prostate-specific antigen era: a large single-institution experience with radical prostatectomy and external-beam radiotherapy. J Clin Oncol 20:3376–3385
Kattan MW, Zelefsky MJ, Kupelian PA, Scardino PT, Fuks Z, Leibel SA (2000) Pretreatment nomogram for predicting the outcome of three-dimensional conformal radiotherapy in prostate cancer. J Clin Oncol 18:3352–3359
Kattan MW, Potters L, Blasko JC, Beyer DC, Fearn P, Cavanagh W, Leibel S, Scardino PT (2001) Pretreatment nomogram for predicting freedom from recurrence after permanent prostate brachytherapy in prostate cancer. Urology 58:393–399
Kattan MW, Zelefsky MJ, Kupelian PA, Cho D, Scardino PT, Fuks Z, Leibel SA (2003) Pretreatment nomogram that predicts 5-year probability of metastasis following three-dimensional conformal radiation therapy for localized prostate cancer. J Clin Oncol 21:4568–4571
NCCN Guidelines Version 3.2018 Prostate cancer. https://www.nccn.org/professionals/physician_gls/pdf/prostate_blocks.pdf; accessed 07.07.2018
Afshar-Oromieh A, Haberkorn U, Schlemmer HP, Fenchel M, Eder M, Eisenhut M, Hadaschik BA, Kopp-Schneider A, Röthke M (2014) Comparison of PET/CT and PET/MRI hybrid systems using a 68Ga-labelled PSMA ligand for the diagnosis of recurrent prostate cancer: initial experience. Eur J Nucl Med Mol Imaging 41:887–897
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, Eisenhut M, Boxler S, Hadaschik BA, Kratochwil C, Weichert W, Kopka K, Debus J, Haberkorn U (2015) The diagnostic value of PET/CT imaging with the 68Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 42:197–209
Schwarzenboeck SM, Rauscher I, Bluemel C, Fendler WP, Rowe SP, Pomper MG, Asfhar-Oromieh A, Herrmann K, Eiber M (2017) PSMA ligands for PET imaging of prostate cancer. J Nucl Med 58:1545–1552
Perera M, Papa N, Christidis D, Wetherell D, Hofman MS, Murphy DG, Bolton D, Lawrentschuk N (2016) Sensitivity, specificity, and predictors of positive 68Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol 70:926–937
Fendler WP, Eiber M, Beheshti M, Bomanji J, Ceci F, Cho S, Giesel F, Haberkorn U, Hope TA, Kopka K, Krause BJ, Mottaghy FM, Schöder H, Sunderland J, Wan S, Wester HJ, Fanti S, Herrmann K (2017) 68Ga-PSMA PET/CT: joint EANM and SNMMI procedure guideline for prostate cancer imaging: version 1.0. Eur J Nucl Med Mol Imaging 44:1014–1024
Freitag MT, Radtke JP, Afshar-Oromieh A, Roethke MC, Hadaschik BA, Gleave M, Bonekamp D, Kopka K, Eder M, Heusser T, Kachelriess M, Wieczorek K, Sachpekidis C, Flechsig P, Giesel F, Hohenfellner M, Haberkorn U, Schlemmer HP, Dimitrakopoulou-Strauss A (2017) Local recurrence of prostate cancer after radical prostatectomy is at risk to be missed in 68Ga-PSMA-11-PET of PET/CT and PET/MRI: comparison with mpMRI integrated in simultaneous PET/MRI. Eur J Nucl Med Mol Imaging 44:776–787
Freitag MT, Radtke JP, Hadaschik BA, Kopp-Schneider A, Eder M, Kopka K, Haberkorn U, Roethke M, Schlemmer HP, Afshar-Oromieh A (2016) Comparison of hybrid (68)Ga-PSMA PET/MRI and 68Ga-PSMA PET/CT in the evaluation of lymph node and bone metastases of prostate cancer. Eur J Nucl Med Mol Imaging 43:70–83
Lütje S, Cohnen J, Gomez B, Grüneisen J, Sawicki L, Rübben H, Bockisch A, Umutlu L, Pöppel TD, Wetter A (2017) Integrated 68Ga-HBED-CC-PSMA-PET/MRI in patients with suspected recurrent prostate cancer. Nuklearmedizin 56:73–81
Eiber M, Weirich G, Holzapfel K, Souvatzoglou M, Haller B, Rauscher I, Beer AJ, Wester HJ, Gschwend J, Schwaiger M, Maurer T (2016) Simultaneous 68Ga-PSMA HBED-CC PET/MRI improves the localization of primary prostate cancer. Eur Urol 70:829–836
Kitajima K, Hartman R, Froemming A et al (2015) Detection of local recurrence of prostate cancer after radical prostatectomy using endorectal coil MRI at 3 T: addition of DWI and dynamic contrast enhancement to T2-weighted MRI. AJR Am J Roentgenol 205:807–816
Bratan F, Niaf E, Melodelima C, Chesnais AL, Souchon R, Mège-Lechevallier F, Colombel M, Rouvière O (2013) Influence of imaging and histological factors on prostate cancer detection and localization on multiparametric MRI: a prospective study. Eur Radiol 23:2019–2029
Eiber M, Herrmann K, Calais J, Hadaschik B, Giesel FL, Hartenbach M, Hope T, Reiter R, Maurer T, Weber WA, Fendler WP (2018) Prostate cancer molecular imaging standardized evaluation (PROMISE): proposed miTNM classification for the interpretation of PSMA-ligand PET/CT. J Nucl Med 59:469–478
Beiderwellen K, Grueneisen J, Ruhlmann V, Buderath P, Aktas B, Heusch P, Kraff O, Forsting M, Lauenstein TC, Umutlu L (2015) [18F]FDG PET/MRI vs. PET/CT for whole-body staging in patients with recurrent malignancies of the female pelvis: initial results. Eur J Nucl Med Mol Imaging 42:56–65
Domachevsky L, Bernstine H, Goldberg N, Nidam M, Stern D, Sosna J, Groshar D (2017) Early 68GA-PSMA PET/MRI acquisition: assessment of lesion detectability and PET metrics in patients with prostate cancer undergoing same-day late PET/CT. Clin Radiol 72:944–950
Wetter A, Lipponer C, Nensa F, Heusch P, Rübben H, Altenbernd JC, Schlosser T, Bockisch A, Pöppel T, Lauenstein T, Nagarajah J (2014) Evaluation of the PET component of simultaneous [18F]choline PET/MRI in prostate cancer: comparison with [18F]choline PET/CT. Eur J Nucl Med Mol Imaging 41:79–88
Spick C, Herrmann K, Czernin J (2016) 18F-FDG PET/CT and PET/MRI perform equally well in cancer: evidence from studies on more than 2,300 patients. J Nucl Med 57:420–430
Heußer T, Mann P, Rank CM, Schäfer M, Dimitrakopoulou-Strauss A, Schlemmer HP, Hadaschik BA, Kopka K, Bachert P, Kachelrieß M, Freitag MT (2017) Investigation of the halo-artifact in 68Ga-PSMA-11-PET/MRI. PLoS One 12:e0183329. https://doi.org/10.1371/journal.pone.0183329
Rischpler C, Beck TI, Okamoto S, Schlitter AM, Knorr K, Schwaiger M, Gschwend J, Maurer T, Meyer PT, Eiber M (2018) 68Ga-PSMA-HBED-CC uptake in cervical, celiac, and sacral ganglia as an important pitfall in prostate cancer PET imaging. J Nucl Med 59:1406–1411
Ruijter ET, van de Kaa CA, Schalken JA et al (1996) Histological grade heterogeneity in multifocal prostate cancer. Biological and clinical implications. J Pathol 180:295–299
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
BH reports grants from German Cancer Aid, German Research Foundation, and Profound Medical, grants, personal fees, and nonfinancial support from Janssen, personal fees and nonfinancial support from Astellas, Bayer, BMS, Lightpoint Medical, Astra Zeneca, and Sanofi, and grants and personal fees from Uromed, all outside the submitted work.
JPR is a company consultant for Saegeling Medizintechnik, Invivo Uronav, Philips, Siemens Healthineers, Beckelmann, and Bender and reports grants from Medical faculty Heidelberg, all outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guberina, N., Hetkamp, P., Ruebben, H. et al. Whole-Body Integrated [68Ga]PSMA-11-PET/MR Imaging in Patients with Recurrent Prostate Cancer: Comparison with Whole-Body PET/CT as the Standard of Reference. Mol Imaging Biol 22, 788–796 (2020). https://doi.org/10.1007/s11307-019-01424-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-019-01424-4