Abstract
P2X3 and P2X2+3 receptors are present on sensory neurons, where they contribute not only to transient nociceptive responses, but also to hypersensitivity underlying pathological pain states elicited by nerve injuries. Increased signalling through P2X3 and P2X2+3 receptors may arise from an increased routing to the plasma membrane and/or gain of function of pre-existing receptors. An obvious effector mechanism for functional modulation is protein kinase C (PKC)-mediated phosphorylation, since all P2X family members share a conserved consensus sequence for PKC, TXR/K, within the intracellularly located N-terminal domain. Contradictory reports have been published regarding the exact role of this motif. In the present study, we confirm that site-directed elimination of the potential phosphor-acceptor threonine or the basic residue in the P+2 position of the TXR/K sequence accelerates desensitization of P2X2 receptors and abolishes P2X3 receptor function. Moreover, the PKC activator phorbol 12-myristate 13-acetate increased P2X3 (but not P2X2) receptor-mediated currents. Biochemically, however, we were unable to demonstrate by various experimental approaches a direct phosphorylation of wild-type P2X2 and P2X3 receptors expressed in both Xenopus laevis oocytes and HEK293 cells. In conclusion, our data support the view that the TXR/K motif plays an important role in P2X function and that phorbol 12-myristate 13-acetate is capable of modulating some P2X receptor subtypes. The underlying mechanism, however, is unlikely to involve direct PKC-mediated P2X receptor phosphorylation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
P2X receptors constitute an abundant class of ligand-gated ion channels, which respond to extracellular ATP and related nucleotides with the opening of an intrinsic pore permeable to Na+, K+ and Ca2+ [1, 2]. A family encompassing seven P2X subunit genes, designated P2X1–7, has been identified in rodents and mammals. Six of the seven subunit isoforms (P2X1-P2X5 and P2X7) are able to assemble into homotrimeric receptor channels [3–8] with distinct pharmacological and electrophysiological phenotypes [9]. According to their sensitivity to the synthetic ATP analogue α,β-methylene adenosine 5′-triphosphate (αβ-meATP) and the rate of current desensitization, P2X receptors are generally subgrouped into at least two categories: (1) rapidly desensitizing and αβ-meATP sensitive (P2X1 and P2X3) and (2) slowly or non-desensitizing and αβ-meATP insensitive (P2X2, P2X4 and P2X7) receptors. The term “non-desensitizing” means that the currents are maintained for at least a few seconds in the continuous presence of agonist. A peculiar phenotype is inherent to heteromeric P2X2/P2X3 (P2X2+3) receptors, which feature αβ-meATP sensitivity combined with a non-desensitizing current response.
P2X receptors are found on the surface of a large variety of cells, where they are involved in numerous sensory processes including nociception under both physiological and pathological processes [10–15]. On nociceptive sensory neurons, extracellular ATP acts as a pain-producing neurotransmitter predominantly through homotrimeric P2X3 receptors or heterotrimeric P2X2+3 receptors. Conditions and mediators that facilitate P2X3 and P2X2+3 receptor-mediated signalling, apparently by potentiating ionic currents, include (1) substance P and bradykinin [16], (2) nerve injury [17] and (3) calcitonin gene-related peptide (CGRP), a potent vasodilator and proinflammatory agent [18]. How this increase in receptor function occurs has not been fully solved. One obvious candidate mechanism is protein kinase C (PKC)-mediated phosphorylation, since all P2X family members share a conserved consensus sequence for PKC-mediated phosphorylation (TXR/K) within the intracellularly located N-terminal domain (Fig. 1a, b). Indeed, results obtained with pharmacological activators and inhibitors are consistent with PKC being involved in P2X3 receptor potentiation by substance P and bradykinin [16], as well as the calcitonin gene-related peptide [18]. Direct PKC-mediated phosphorylation has so far been demonstrated only for the P2X2 receptor, with 18T of the 18TPK20 sequence as the phospho-acceptor site [19]. Mutational analysis has further shown that the TXR/K sequence of the P2X1, P2X2 and P2X3 receptors plays an important role in controlling the rate of receptor desensitization [16, 19, 20]. Changes of the rate of desensitization could profoundly influence the efficiency of synaptic transmission and thus contribute to pathological pain states. Overall, there is significant interest in a better understanding of the mechanisms involved in the short-term and long-term regulation of P2X receptors.
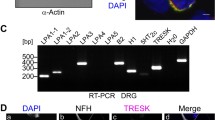
Effect of site-directed modification of a putative PKC motif on currents mediated by ATP-activated P2X2 and P2X3 receptors. a Schematic model of the transmembrane topology of the rat P2X3 subunit illustrating the N-terminal position of the 12TTK14 sequence. b Alignment of intracellular N-terminal amino acid sequences of the seven P2X subunit isoforms reveals a highly conserved consensus motif, TXR/K. c Typical current traces elicited by applying 10-s pulses of 100 μM ATP to oocytes expressing the indicated wild-type or mutant P2X2 receptors. d Typical current traces elicited by applying 10-s pulses of 100 μM ATP to oocytes expressing the indicated wild-type or mutant P2X3 receptors. Gray areas indicate the duration of ATP application. e All the P2X2 and P2X3 receptors and receptor mutants were expressed efficiently at the cell surface. Intact, healthy oocytes expressing the indicated proteins for 2 days were surface-labelled with the membrane impermeant reactive Cy5 dye and then extracted with dodecylmaltoside. Recombinant proteins were isolated by Ni2+ chelate chromatography and resolved by reducing SDS-PAGE. Shown is a fluorescence scan of an SDS-PAGE gel
The aim of this study was to assess biochemically the conditions in which P2X2 and P2X3 receptors become directly phosphorylated by PKC in a heterologous system. While this work was in progress, a similar study was published for the P2X3 receptor that arrived at essentially the same conclusion, namely that the P2X3 receptor is unlikely to be a direct PKC substrate [21]. Our results complement and extend this finding by demonstrating that the P2X2 receptor also does not serve as a substrate for direct PKC-mediated phosphorylation.
Materials and methods
Materials
The sources of antibodies, enzymes or peptide substrates are specified at the appropriate places in the text. Chemicals not otherwise specified were purchased in the highest available quality from Sigma-Aldrich (Taufkirchen, Germany) or Merck (Darmstadt, Germany).
Peptide-specific antibodies to P2X1, P2X2 and P2X3 subunits
Peptides ATSSTLGLQENMRTS (residues 385-399 of the P2X1 subunit), QQDSTSTDPKGLAQL (residues 458–472 of the P2X2 subunit) and VEKQSTDSGAYSIGH (residues 383–397 of the P2X3 subunit) were selected based on their lack of similarity with known proteins and predicted hydrophilicity for raising polyclonal antibodies against the C-terminal end of the rat subunits P2X1, P2X2 and P2X3, respectively. Rabbit polyclonal antibodies were ordered through the Custom Antibody Production Services of Eurogentec (Seraing, Belgium). After 3 months and a total of four immunizations, rabbits were sacrificed by complete bleeding. Peptide-specific antibodies were purified from the serum by affinity columns coupled with the peptides used for immunization. Immunoblotting showed that the antibodies recognized only the receptor against which they were raised, thus demonstrating isoform specificity of these antibodies (results not shown). The antibodies were aliquoted at 0.12–0.16 mg/ml in phosphate-buffered saline (PBS) containing 0.1% bovine serum albumin (BSA) and 0.01% thimerosal and stored at −80°C.
cDNA constructs
Plasmids encoding wild-type and N-terminal hexahistidine-tagged (His-tagged) versions of rat P2X1 subunits (rP2X1, GenBank accession no. X80477), P2X2 subunits (rP2X2, GenBank accession no. U14414) or rat P2X3 subunits (rP2X3, GenBank accession no. X90651) in the oocyte expression vector pNKS2 [22] were available from previous studies [3, 8]. Insertion and replacement mutations were introduced by QuikChange site-directed mutagenesis (Stratagene, La Jolla, CA, USA). For protein expression in mammalian cells, the receptor cDNAs were subcloned from the oocyte expression vector pNKS2 into pcDNA3.1. The plasmid His-rP2X2-EGFP-pcDNA3.1 with a C-terminal enhanced green fluorescent protein (EGFP) fusion was generated by eliminating the stop codon in His-rP2X2 and adding the coding sequence of EGFP (Clontech, Palo Alto, CA, USA) in frame. All constructs were verified by restriction analysis and nucleotide sequencing. A pEGFP-C1 plasmid harbouring the N-terminally EGFP-tagged splicing factor SF3B1 was kindly provided by our colleague Dr. Walter Becker [23].
P2X receptor expression in Xenopus laevis oocytes
Capped cRNAs were synthesized from plasmids linearized downstream to the 100 bp long polyA tail provided by the oocyte expression vector pNKS2 [22] and injected at 0.5 μg/μl in 50-nl aliquots into collagenase-defolliculated X. laevis oocytes using a Nanoliter 2000 injector (WPI, Sarasota, FL, USA), as detailed previously [24]. Oocytes were maintained at 19°C in sterile oocyte Ringer’s solution [ORi: 90 mM NaCl, 1 mM KCl, 1 mM CaCl2, 1 mM MgCl2 and 10 mM hydroxyethylpiperazine ethanesulfonic acid (HEPES), pH 7.4] supplemented with 50 μg/ml of gentamicin.
Heterologous expression in HEK293 cells
cDNAs encoding P2X subunits in pcDNA3.1 vector (Invitrogen, Karlsruhe, Germany) or the splicing factor SF3B1 in EGFP-C1 vector were transiently transfected into HEK293 cells using Lipofectamine LTX (Invitrogen, Karlsruhe, Germany). Cells were cultured at 37°C in Dulbecco’s modified Eagle’s medium (DMEM) (Invitrogen) supplemented with 10% (v/v) fetal calf serum (FCS) (PAA Laboratories, Linz, Austria), 100 U/ml of penicillin G and 100 μg/ml of streptomycin.
Metabolic [35S]methionine labelling of oocytes
For metabolic [35S]methionine labelling of oocyte-expressed recombinant proteins, cRNA-injected oocytes and non-injected controls were incubated overnight with L-[35S]methionine (>40 TBq/mmol; PerkinElmer, Boston, MA, USA) at about 100 MBq/ml (0.4 MBq per oocyte) in ORi at 19°C, and then chased for 24 h.
Surface fluorescence labelling of oocytes
Selective fluorescence labelling of plasma membrane-bound P2X receptors was achieved by using the amino-reactive fluorescent Cy5 dye (GE Healthcare, Freiburg, Germany), which is membrane impermeant due to its two sulfonic acid groups. Two days after cRNA injection, oocytes were washed with oocyte-PBS pH 8.5 (20 mM Na phosphate, 110 mM NaCl, 1 mM MgCl2), and then incubated for 30 min at ambient temperature with Cy5 dye, which was diluted 200-fold to a final concentration of 50 μg/ml from a dimethyl sulfoxide (DMSO) stock solution. The reaction was terminated by washing the cells with oocyte-PBS, followed by membrane protein extraction with dodecylmaltoside and receptor purification (see below).
Isolation of recombinant P2X receptors from X. laevis oocytes or HEK293 cells
His-tagged receptors were purified by Ni2+ nitrilotriacetic acid (NTA) agarose (Qiagen, Hilden, Germany) affinity chromatography from non-ionic detergent extracts of oocytes or HEK293 cells in the presence of iodoacetamide essentially as described [3, 8, 25]. Slight modifications were that buffers were supplemented with ethylenediaminetetraacetate (EDTA)-free Halt™ protease inhibitor cocktail (Pierce, Rockford, IL, USA), 50 mM NaF and 50 mM Na4P2O7 for phosphatase inhibition, and that digitonin was replaced by 0.2% and 0.05% dodecylmaltoside for membrane protein extraction and repetitive washing of resin-bound proteins, respectively. Proteins were released from the washed Ni2+ NTA agarose beads with non-denaturing elution buffer consisting of 250 mM imidazole/HCl (pH 7.4) and 0.02% dodecylmaltoside, and then kept at 0°C until analysed on the day of purification.
In addition, immunoprecipitation assays were performed using either cRNA-injected Xenopus oocytes or transiently transfected HEK293 cells. Cells were lysed in ice-cold immunoprecipitation lysis buffer containing 150 mM NaCl, 25 mM Tris/HCl pH 7.4, 20 mM NaF, 20 mM Na4P2O7, 10 μl/ml Halt™ protease inhibitor cocktail without EDTA (Pierce, Rockford, IL, USA), 1% sodium dodecyl sulfate (SDS) (w/v) and 50 mM iodoacetamide. For efficient solubilization, lysates were incubated for 30 min on ice with occasional vortexing, and then cleared by centrifugation for 15 min at 16,100 g and 4°C. The cleared SDS extract was diluted 1:1 with immunoprecipitation binding buffer [150 mM NaCl, 20 mM Tris/HCl pH 7.4, 0.4 mM phenylmethylsulfonyl fluoride (PMSF), 0.5% Triton X-100 v/v and 25 mM iodoacetamide], supplemented 1:1,000 with the desired peptide-specific P2X2 or P2X3 antibodies or a polyclonal goat anti-EGFP antibody (Rockland, Gilbertsville, PA, USA) and incubated for 2 h on ice. Immunocomplexes were bound to the protein A Sepharose by overnight head-over-head rotation at 8°C, then washed 5 times with immunoprecipitation binding buffer containing 0.1% Triton X-100 and finally eluted by incubating the beads for 15 min at 56°C in reducing sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) sample buffer.
In vitro PKC phosphorylation assay
In vitro phosphorylation assays were performed by using P2X receptors as substrates, purified as detailed above. In addition, a selective peptide PKC substrate (RRGRTGRGRRGIYR, Calbiochem-Merck, Darmstadt, Germany, final concentration 150 μM) corresponding to the amino acid sequence 1487-1500 of the hepatitis C virus polyprotein [26] was used as a positive control. The proteins or the peptide were incubated for 30 min at 30°C with 0.02 unit (0.02 μg) of purified catalytic PKC subunit from rat brain and 50 μM [γ-32P]ATP (10 mCi/ml, Amersham Biosciences GE Healthcare, Freiburg, Germany) in phosphorylation buffer containing 6 mM CaCl2, 10 mM MgCl2, 20 mM Tris/HCl pH 7.5, 1 mM EDTA, 1 mM mercaptoethanol, 0.05% Triton X-100 (v/v) and 0.1 mg/ml BSA. The reaction was terminated by boiling in reducing SDS-PAGE sample buffer for 30 s. Proteins were resolved by reducing SDS-PAGE and visualized by immunoblotting or phosphorimaging as detailed below.
In vivo phosphorylation assay
Transiently transfected HEK293 cells were metabolically labelled by a 3-h incubation with 500 μCi/ml of [32P]orthophosphate (Amersham Biosciences GE Healthcare, Freiburg, Germany) in phosphate-free oocyte Ringer solution or in phosphate-free DMEM (Invitrogen, Karlsruhe, Germany) as appropriate. Cells were treated with or without 100 nM phorbol 12-myristate 13-acetate (PMA; Sigma-Aldrich, Taufkirchen, Germany) or 100 nM calyculin A (Tocris Bioscience, Ellisville, MO, USA) for 10 min at ambient temperature. Non-incorporated radioactivity was removed by rinsing the cells twice with tracer-free medium. Affinity purification or immunoprecipitation was performed as described above followed by SDS-PAGE and immunoblotting or phosphorimaging.
SDS-PAGE
Samples for SDS-PAGE were denatured by incubating in reducing SDS-PAGE sample buffer for 15 min at 56°C and then electrophoresed on a Laemmli SDS-PAGE gel (10% acrylamide) in parallel with [14C]-labelled molecular mass markers (Rainbow™, Amersham Biosciences GE Healthcare, Freiburg, Germany). Cy5-labelled proteins were visualized by scanning the wet SDS-PAGE gel with a fluorescence scanner (Typhoon, GE Healthcare, Freiburg, Germany). For visualization of radiolabelled or non-labelled proteins, SDS-PAGE gels were either fixed, dried and exposed to a PhosphorImager screen, and scanned using a Storm 820 PhosphorImager (Amersham Biosciences GE Healthcare, Freiburg, Germany) or/and blotted to polyvinylidene fluoride (PVDF) membranes.
Immunoblotting
Proteins separated by SDS-PAGE were electroblotted onto PVDF membranes. Membranes were blocked for 1 h with 5% non-fat milk in PBS (or, alternatively, with 5% BSA if the phosphothreonine monoclonal antibody was used for immunoblotting), washed 3 × 5 min with PBST (0.1% Tween 20 in PBS) and incubated for 2 h at 4°C in PBS containing the appropriate primary antibody. Phosphorylated proteins were detected by immunoblotting with a phosphothreonine monoclonal antibody (Cell Signaling Technology, Beverly, MA, USA). Alternatively, the peptide-specific antibodies to P2X2 and P2X3 subunits were used to verify receptor expression levels. Following washing in PBST, an appropriate horseradish peroxidase-conjugated secondary antibody (goat anti-mouse or goat anti-rabbit, Pierce, Rockford, IL, USA) was applied for 1 h in PBS supplemented with 1% non-fat milk. After another 3 × 5 min washes with PBST, immunoreactive bands were visualized by chemiluminescence imaging using a Fujifilm LAS-3000 system (Tokyo, Japan) and the AIDA Image Analyser Software Version 4.08 (Raytest, Straubenhardt, Germany).
Two-electrode voltage clamp current recordings and electrical capacitance measurements
Two-microelectrode voltage clamp measurements of X. laevis oocytes were performed 2 days after cRNA injection using a Turbo TEC-05 amplifier (npi electronics, Tamm, Germany) interfaced by an INT-20X AD/DA converter (npi electronics, Tamm, Germany) to a personal computer running the CellWorks Lite 5.1 software (npi electronics, Tamm, Germany), as detailed previously [27–29]. Current traces were elicited by 100 μM ATP at 1- to 5-min intervals (Sigma–Aldrich, Taufkirchen, Germany) at a holding potential of −60 mV in nominally Ca2+-free bath medium (designated Mg-ORi) to avoid activation of endogenous Ca2+-activated Cl− channels. ATP was prepared in Mg−ORi at its final concentration and applied by gravity-fed perfusion at a flow rate of 10 ml/min to an oocyte held by the two microelectrodes in the bath chamber (volume ∼10 μl). Switching between different perfusion solutions was achieved with electromagnetic valves controlled by the CellWorks Lite 5.1 software. Electrophysiological recordings were analysed using the Origin 6.0 software (Microcal Software Inc., Northampton, MA, USA). Single exponentials were fitted to the decay phase of the macroscopic currents with a nonlinear least squares method. The time constant τ was taken as an estimate of the rate of receptor desensitization.
To monitor PMA-induced changes in the oocyte surface area, depolarizing voltage steps of ΔV = 10 mV were applied from the holding potential to elicit a capacitive transient I cap, the integral of which yields the charge movement Qcap and thus the membrane capacitance C m = Q cap/ΔV [30–32]. PMA was dissolved in DMSO to a stock solution of 10 mM and stored at −20°C. On the day of the experiment, the stock solution was pre-diluted to 100 μM in DMSO and then further diluted with Mg-ORi to the final concentration of 100 nM. Vehicle control experiments with a final concentration of 0.1% DMSO did not reveal any effects on P2X2 receptor-mediated currents measured with X. laevis oocytes (results not shown). All measurements were made at room temperature (21–23°C).
Data analysis
Data are shown as means±SEM. The paired Student’s t-test (two-tailed) was used to compare current amplitudes with statistical significance set to p < 0.05.
Results
Site-directed modification of a putative N-terminal PKC site affects the electrophysiological phenotype of P2X2 and P2X3 receptor channels
First, we tested each of the non-mutated and mutant receptor constructs for expression of an ATP-gated inward current in cRNA-injected X. laevis oocytes. Application of 100 μM ATP induced typical non-desensitizing currents through oocyte-expressed P2X2 receptors (Fig. 1c, left current trace). The P2X2 subunit shares with other P2X subunit isoforms a conserved consensus site for PKC phosphorylation (TXR/K, where T is the phosphorylation site and X denotes any amino acid; see Fig. 1a, b). Disruption of the conserved N-terminal PKC site by mutating the phosphor-acceptor 18T to A resulted in a rapidly desensitizing channel (Fig. 1c, middle current trace). Also, replacement of 20K by T resulted in a desensitizing phenotype (Fig. 1c, right current trace). Since PKC preferentially phosphorylates threonine (or serine) residues that are close to a C-terminal basic residue, replacement of 20K in the P+2 position by a non-basic residue such as T will destroy the putative PKC site despite preserving the phosphor-acceptor 18T. Virtually identical findings had previously been reported by Boue-Grabot et al. [19]. The average half-times of desensitization (τ) of the 18A and 20T P2X2 mutants were quite similar, with mean τ values (±SEM) of 4.5 ± 0.4 s and 7.3 ± 0.5 s, respectively, of eight oocytes from two females per value.
ATP applied to oocytes expressing the P2X3 receptor elicited a rapidly desensitizing inward current (Fig. 1d, left current trace) as is typical for this P2X receptor subtype. Incorporation of similar mutations, as in the P2X2 subunit in the analogous positions of the P2X3 receptor T12A or K14T, completely abolished P2X3 receptor function (Fig. 1d, middle and right current traces). Visualization of plasma membrane-bound fluorescence-labelled P2X receptors by affinity purification combined with SDS-PAGE and fluorescence scanning verified that all the receptors were efficiently exported to the oocyte surface (Fig. 1e).
The PKC activator PMA augments P2X3 receptor-mediated currents, yet leaves P2X2-mediated currents unchanged
Since the mutagenesis data for the P2X2 and P2X3 receptor were consistent with the possibility of a regulatory role for PKC in P2X receptor function, we examined whether the PKC activator PMA was capable of affecting the electrophysiological phenotype of P2X2 or P2X3 receptors. In planning the experiments, we considered that PMA treatment of X. laevis oocytes is known to induce a pronounced endocytotic reduction of the cell surface area, as evidenced microscopically and electrophysiologically by the disappearance of virtually all microvilli and a concomitant decrease of the electrical capacitance of the plasma membrane, respectively [31, 32]. Associated with oocyte surface reduction is a proportional internalization of membrane proteins, such as endogenous Na+-K+ pumps, suggesting that PMA treatment would stimulate internalization of recombinant P2X receptors as well. Re-examination of the time course of the PMA-induced reduction of the oocyte surface area showed that the electrical capacitance did not start to decline significantly before 10 min after PMA application (Fig. 2a). Accordingly, all current recordings were done within a time window of 10 min after PMA application to prevent any contribution of receptor internalization to the PMA effect on P2X receptor-dependent currents.
Effect of PMA on ATP-induced currents mediated by expressed P2X2 and P2X3 receptors in X. laevis oocytes. a The electrical membrane capacitance was monitored as a measure of the oocyte surface area during sustained stimulation with PMA. Each bar represents the mean Cm±SEM calculated from the areas under the current transients elicited in 10-s intervals by five consecutive 10-mV depolarizing steps. b, c Representative current traces elicited by 10-s lasting pulses of 100 μM ATP applied in 10-min intervals to oocytes expressing the indicated P2X receptors or P2X receptor mutants. Where denoted by a black bar, oocytes were pre-incubated with 100 nM PMA before ATP was co-applied. PMA was without effect on the P2X2 receptor-mediated current (b), but induced a marked increase of the current amplitude mediated by P2X3 receptors (c). Gray areas indicate the duration of ATP application
Figure 2b and c show typical current traces elicited by ATP from P2X2 or P2X3 receptor-expressing oocytes before and after a 10-min exposure to PMA. PMA neither affected the shape nor the amplitude of P2X2 receptor-mediated current (Fig. 2b). However, PMA produced a marked increase of the current amplitude mediated by the P2X3 receptor (Fig. 2c). In one experiment with four oocytes, a statistically significant increase of the P2X3-mediated current amplitude by PMA of 155 ± 42% (SEM) was determined.
P2X2 and P2X3 receptors exist in a non-phosphorylated state in both X. laevis oocytes and HEK293 cells
To explain the accelerated desensitization upon site-directed perturbation of the 18TXK20 motif, it has been suggested that the wild-type P2X2 receptor is constitutively phosphorylated at 18T and that this phosphorylation is responsible for the slow desensitization rate [19]. To address this issue, we next examined biochemically whether P2X3 receptors also exist in a constitutively phosphorylated state; the P2X2 receptor was also analysed to allow for a direct comparison of the results. Both parent P2X receptors and mutants were purified by Ni2+ chelate affinity chromatography from dodecylmaltoside extracts of [35S]methionine-labelled oocytes, resolved by SDS-PAGE, and blotted onto a PVDF membrane. However, probing with a phosphothreonine-specific monoclonal antibody revealed no discernible signal (Fig. 3a) despite the presence of significant amounts of [35S]methionine-labelled P2X2 and P2X3 protein in the SDS-PAGE gel (Fig. 3b).
Immunoblots show no constitutive phosphorylation of oocyte-expressed P2X2 or P2X3 receptors. The indicated wild-type or mutant P2X subunits were purified by Ni2+ chelate chromatography from [35S]methionine-labelled X. laevis oocytes and resolved by denaturing SDS-PAGE. a Shown is a representative immunoblot probed with a phosphothreonine-specific monoclonal antibody and a peroxidase-conjugated secondary antibody. No phosphorylation signal could be detected at the SDS-PAGE migration position of P2X2 and P2X3 subunits, which are indicated by the adjacent PhosphorImager scan in panel b. b Direct PhosphorImager visualization of metabolically [35S]methionine-labelled parent and mutant P2X subunits resolved by SDS-PAGE of the same samples as in panel a. c Left panel: representative immunoblot of P2X2 subunits tagged with either an N-terminal or C-terminal hexahistidine sequence (designated His-P2X2 or P2X2-His, respectively) and probed with a phosphothreonine-specific monoclonal antibody and a peroxidase-conjugated secondary antibody. No phosphorylation signal could be detected at the SDS-PAGE migration position of P2X2 subunits, which were visualized by immunoblotting with the P2X2 subunit polyclonal antibody (middle panel) or PhosphorImager scanning of incorporated [35S]methionine (right panel)
To exclude the possibility that the apparent lack of receptor phosphorylation resulted from an interference between the N-terminal His tag and the PKC site of P2X3 or P2X2 receptor subunits, which are separated by only 12 or 20 residues, respectively, we performed analogous experiments with a C-terminally His-tagged P2X2 receptor, P2X2-His. As apparent from Fig. 3c, neither N-terminally nor C-terminally His-tagged P2X2 receptor became phosphorylated, as evidenced by immunoblotting with a phosphor-specific anti-threonine antibody (Fig. 3c). The presence of P2X2 receptor protein was verified by immunoblotting and metabolic labelling with [35S]methionine (Fig. 3c, middle and right panel).
Boue-Grabot et al. [19] have demonstrated phosphorylation of P2X2 receptors expressed in HEK293 cells. To address the possibility that P2X receptor phosphorylation is host cell specific, we analysed HEK293 cells transiently transfected with P2X2 or P2X3 expression plasmids. P2X receptor proteins were isolated by immunoprecipitation and resolved by reducing SDS-PAGE. The efficient expression of the P2X3 receptor or the C-terminally EGFP-tagged P2X2 receptor in HEK293 cells was verified by immunoblotting with subunit bands migrating at 54 kDa or 83 kDa (27 kDa contributed to the P2X2 subunit by the EGFP tag), respectively (Fig. 4b). However, phosphorylated P2X2 or P2X3 subunits could not be detected by immunoblotting with a phosphothreonine-specific antibody (Fig. 4a). In contrast, the PKC-phosphorylated splicing factor SF3B1, which was expressed in HEK293 cells as a positive control substrate and immunoprecipitated with an EGFP antibody, was efficiently phosphorylated under identical conditions, assuring that the assay was able to detect phosphorylated proteins (Fig. 4a, lane 1). Taken together, these results suggest that both P2X2 and P2X3 receptors exist constitutively in a non-phosphorylated state in both X. laevis oocytes and HEK293 cells.
Immunoblotting reveals no constitutive phosphorylation of HEK293 cell-expressed P2X2 and P2X3 receptors. The indicated proteins were isolated by immunoprecipitation using the peptide-specific P2X3 subunit polyclonal antibody or an EGFP-specific polyclonal antibody as appropriate and resolved by reducing SDS-PAGE. a Shown is an immunoblot probed by phosphothreonine-specific monoclonal antibody and a peroxidase-conjugated secondary antibody. Note that phosphorylation of the P2X3 receptor or the EGFP-tagged P2X2 receptor is not detectable, whereas a positive control—the EGFP-tagged splicing factor SF3B1 (migration mass 97 kDa [23])—was detected by the antibody. b The same samples as in panel a were immunoblotted using peptide-specific P2X2 and P2X3 subunit polyclonal antibodies to verify the expression of the transfected genes
PMA-activated PKC does not drive the phosphorylation of P2X2 or P2X3 receptors
A majority of protein kinases are quiescent unless their activity is stimulated by specific stimuli and effectors. To drive phosphorylation by active endogenous PKC, we incubated non-denatured recombinant His-tagged P2X1, P2X2 and P2X3 receptors isolated by Ni2+ NTA agarose affinity chromatography from dodecylmaltoside extracts of X. laevis oocytes with PMA-stimulated lysates of X. laevis oocytes (Fig. 5a) or HEK293 cells (Fig. 5b) in the presence of [γ-32P]ATP. As a positive control, a specific peptide PKC substrate RRGRTGRGRRGIYR was incubated with the lysates. This peptide was equally well phosphorylated by addition of either cell lysate or a commercial preparation of the rat brain PKC subunit (Fig. 5a, b). In contrast, however, no 32P incorporation could be detected in the SDS-PAGE migration position of the P2X1, P2X3 or P2X2 receptor subunit at 56 kDa, 54 kDa or 66 kDa, respectively. The presence of purified P2X1, P2X2 and P2X3 receptor subunit protein in this assay was verified by immunoblotting using P2X1-, P2X2- or P2X3-specific antibodies (Fig. 5c). The phosphorylation of the synthetic peptide clearly demonstrates that both X. laevis oocytes and HEK293 cells contain sufficient endogenous PKC to drive at least the phosphorylation of a synthetic peptide substrate.
Lysates of X. laevis oocytes or HEK293 cells contain endogenous PKC, but do not support PMA-driven phosphorylation of P2X2 or P2X3 receptors. The indicated wild-type and mutant P2X receptors were purified by non-denaturing Ni2+ chelate chromatography from X. laevis oocytes, supplemented with [γ-32P]ATP, 100 nM PMA and oocyte lysate (a) or HEK293 cell lysate (b), and incubated for 30 min at ambient temperature. In parallel, a peptide PKC substrate (final concentration 0.5 μg/μl) was incubated with [γ-32P]ATP, PMA and either of the two cell lysates or the purified rat brain PKC catalytic subunit as indicated. The proteins were resolved by reducing SDS-PAGE and visualized by phosphorimaging. Note that the band pattern was similar irrespective of whether protein of mock-injected oocytes or P2X receptor-expressing oocytes was used as a substrate, arguing against specific labelling of either P2X receptor. Arrows indicate migration positions of P2X1, P2X2 and P2X3 subunits. Arrowhead in a, dominant background band that is present in all oocyte samples. The peptide PKC substrate was similarly labelled by lysates or purified rat brain PKC, confirming the presence of endogenous PKC in X. laevis oocytes and HEK293 cells. c The same samples as in panels a and b were resolved on a separate SDS-PAGE gel. The indicated P2X subunits were detected by immunoblotting using the appropriate P2X subunit-specific polyclonal antibodies. A sample of mock-transfected cells was simultaneously probed with the P2X2 and P2X3 subunit-specific polyclonal antibodies
Discernible phosphorylation of P2X2 and P2X3 receptors might be obscured by a low level of endogenous PKC. Therefore, an analogous experiment was performed, in which the purified P2X2 and P2X3 receptors were incubated with purified rat brain PKC catalytic subunit rather than cell lysate in the presence of [γ-32P]ATP. Again, the specific peptide PKC substrate was efficiently phosphorylated as demonstrated both by direct phosphorimaging (Fig. 6a) and immunoblotting with the phosphothreonine monoclonal antibody (Fig. 6b). Phosphorylated P2X2 or P2X3 subunits could not be detected by either method (Fig. 6a, b) despite the presence of abundant amounts of the respective P2X subunits in the assays (Fig. 6c).
PKC phosphorylates a specific PKC substrate in vitro, but does not phosphorylate P2X2 or P2X3 receptors. The immunoprecipitated recombinant P2X2 or P2X3 receptor from X. laevis oocytes or a synthetic peptide (1 or 10 μg) derived from the non-structural protein 3 of hepatitis C virus, which serves as a specific substrate for PKC, were incubated for 30 min with purified rat brain PKC catalytic subunit (0.02 μg corresponding to 0.02 U/μl) in the presence of 50 μM [γ-32P]ATP (10 mCi/ml), and then subjected to SDS-PAGE and phosphorimaging. The rat brain PKC catalytic subunit does not require Ca2+ and phosphatidylserine for activity [42]. 32P was incorporated into the PKC substrate (left panel) and was also detected by immunoblotting with an anti-phosphothreonine antibody (middle panel). However, there was no detectable 32P incorporation at a migration position of ∼66 kDa or ∼54 kDa of the P2X2 or P2X3 subunit, respectively, the presence of which could be verified by immunoblotting (right panel)
PMA or calyculin A do not enhance phosphorylation of P2X3 receptors in intact HEK cells
In a final set of experiments, we attempted to directly demonstrate phosphorylation in vivo by using metabolic [32P]orthophosphate labelling combined with immunoprecipitation analysis as a read out. Mock-transfected and P2X3 receptor-transfected HEK293 cells were incubated with [32P]orthophosphate in phosphate-free DMEM, followed by incubation with the PKC activator PMA and/or the phosphoserine/phosphothreonine phosphatase inhibitor calyculin A. The PhosphorImager scan revealed an identical pattern of phosphorylated bands almost irrespective of the experimental conditions, with no evidence for a significant 32P-labelling of the P2X3 subunit (Fig. 7, top panel). P2X3 receptor expression was verified by immunoblotting (Fig. 7, bottom panel).
PMA and calyculin A do not induce phosphorylation of P2X3 receptors in intact HEK cells. Mock- and P2X3 receptor-transfected HEK293 cells were incubated with [32P]orthophosphate (500 μCi/ml) for 3 h in phosphate-free DMEM, followed by a 10-min incubation with 100 nM of each, the PKC activator PMA and/or the phosphatase inhibitor calyculin A. Triton X-100 extracts were then prepared from the cells and subjected to immunoprecipitation using the peptide-specific P2X3 subunit polyclonal antibody, followed by reducing SDS-PAGE and phosphorimaging. The migration position of the P2X3 subunit is marked by an arrow, indicating the absence of 32P incorporation into the P2X3 subunit. P2X3 receptor expression was verified by immunoblotting with the P2X3 subunit polyclonal antibody (bottom panel)
Discussion
Both P2X3 and P2X2+3 receptors are present on sensory neurons, where they play an important role in nociception. In addition to mediating transient nociceptive responses, these receptors contribute critically to the hyperexcitability that underlies abnormal pain states elicited by nerve injuries. One mechanism for the increased responsiveness to ATP is sensitization of P2X3 and P2X2+3 receptors arising from a significant enhancement in the trafficking of P2X3 subunit-containing receptors and/or an increase in function of pre-existing receptors [17]. An obvious candidate mechanism for functional modulation is phosphorylation, which is believed to occur universally in all ligand-gated ion channels as reviewed by Levitan [33].
Evidence for a control of P2X receptor channel function by PKC-mediated phosphorylation
Site-directed elimination of the putative N-terminal PKC site has already previously been shown to severely affect the electrophysiological phenotype of several P2X receptor subtypes, including P2X1, P2X2 and P2X3 receptors from rat and/or human [16, 19, 20, 34] and P2X5 receptors from frog [35]. Replacing the putative phospho-acceptor residue 18T or the basic residue in the P+2 position (20K) by A or a non-basic residue, respectively, imposed rapidly desensitizing properties onto the non-desensitizing wt P2X2 receptor without grossly affecting the current amplitude. In contrast, when analogous mutations were introduced into the rapidly desensitizing receptor subtypes P2X1 or P2X3, peak currents declined to low or undetectable levels, respectively [16 ,20, 34]; the same observation was also made with the slower desensitizing frog P2X5 receptor [35]. Overall, the results obtained by site-directed elimination of the N-terminal TXR/K motif can be plausibly reconciled with the hypothesis that the rate of P2X receptor channel desensitization is controlled by a phosphorylation-dephosphorylation mechanism, with phosphorylation at this site being associated with a decreased rate of desensitization.
Additional evidence for a possible involvement of PKC-dependent phosphorylation comes from experiments with the PKC activator PMA, which was consistently found to elicit a severalfold increase in currents mediated by the P2X1 receptor [36] or the P2X3 receptor [16, 18, 21] without changing the rate of desensitization. A PMA-induced change of the current desensitization was noted for C-terminally truncated P2X2 receptors, which are known to exhibit a desensitizing phenotype in contrast to the parent full-length P2X2 receptors [19, 37]. PMA treatment converted the rapidly desensitizing phenotype of truncated P2X2 receptors to slowly desensitizing, but did not affect the kinetic properties or current amplitudes of the full-length P2X2 receptors. The same lack of effect of PMA has been observed with wild-type P2X2 receptors stably expressed in HEK293 [38]. It has been inferred from these data that P2X2 receptors are constitutively phosphorylated and that this phosphorylation is responsible for their non-desensitizing phenotype. Consistent with this view, immunoblot analysis with a phosphothreonine-proline-specific monoclonal antibody efficiently detected wild-type P2X2 receptors with an intact PKC site, but not P2X2 receptor mutants with a disrupted PKC site [19]. Constitutive phosphorylation has been also demonstrated for the P2X1 receptor expressed in HEK293 cells [34]. Further studies demonstrated that exogenously added uridine triphosphate (UTP) potentiated the current mediated by endogenous and expressed P2X3 receptors in response to αβ-meATP as agonist. Substitution of phospho-acceptor residues of PKC consensus sites located in the ectodomain of the P2X3 receptor abolished this UTP-induced current potentiation, suggesting a role of ecto-protein kinase C in P2X3 receptor regulation [39, 40].
Evidence against a control of P2X receptor channel function by PKC-mediated phosphorylation
In direct contrast to the results of Boue-Grabot et al. [19], we were unable to demonstrate a direct phosphorylation of wild-type P2X2 receptors expressed in X. laevis oocytes and HEK293 cells. The various experimental approaches for phosphorylation detection that we applied included immunoblot analysis of purified P2X2 receptors. In the experiments shown, we used a phosphothreonine-specific monoclonal antibody instead of a phosphothreonine-proline-specific antibody, because the TXK motif of the P2X3 receptor contains a threonine in the -X-position instead of the proline found in the amino acid sequence of the P2X1 and P2X2 subunit (cf. Fig. 1b). However, even when we used the same phosphothreonine-proline-specific antibody as Boue-Grabot et al. [19], we could not demonstrate phosphorylation of P2X2 receptors in our experiments (data not shown).
Recently, it has been shown that a proline in the P+1 position strongly disfavours substrate recognition by PKC [41], suggesting that our negative results with P2X2 receptors may not result from technical limitations, but reflect the inherent inability of P2X2 receptors to serve as substrates for PKC. Notably, P2X3 receptors, despite harbouring a T in the P+1 position, could also not be demonstrated to become phosphorylated by PKC in our experiments, as well as in a recently published paper [21]. Further evidence against a direct PKC-mediated P2X receptor phosphorylation comes from co-expression studies of P2X1 and G protein-coupled receptors. Co-expression of the metabotropic glutamate receptor mGluR1α with P2X1 receptors produced a 2.5-fold increase of the P2X1 receptor-mediated current that was blocked by the PKC inhibitor staurosporine and could be mimicked by PMA treatment of singly expressed P2X1 receptors. Although the pharmacological data are basically consistent with PKC-mediated receptor phosphorylation being involved, mutant P2X1 receptors with a disrupted N-terminal PKC site (T18V) still showed PMA-mediated and mGluR1α-mediated potentiation. Also, PMA treatment did not lead to an increase in the (rather weak) basal phosphorylation of the P2X1 receptor [36].
Functional data supporting a role of PKC in P2X receptor regulation have been detailed above. There are, however, also functional data that are inconsistent with the view that the TXR/K motif represents a true PKC site: (1) replacement of the phospho-acceptor threonine by an acidic residue to mimic incorporation of a negatively charged phosphate group by constitutive phosphorylation was unable to restore the function of P2X1 receptors [34] and P2X3 receptors [16]; (2) the PMA-induced potentiation of hP2X1 receptor currents could be blocked by the PKC inhibitor staurosporine, but surprisingly, not by site-directed elimination of the PKC site [36]; thus it is much more likely that PMA exerts its effect on the P2X1 receptor (and the P2X3 receptor) through a yet to be identified accessory protein.
Taken together, there is no doubt that the TXR/K motif plays an important role in the functioning of P2X receptors, and that PMA is capable of modulating P2X1- and P2X3-mediated receptor currents. The underlying mechanism, however, is unlikely to involve direct PKC-mediated phosphorylation of P2X receptors. The existence of a proline in the P+1 position in several P2X subunit isoforms (P2X1, P2X2, P2X4) might be one causative factor preventing direct phosphorylation by PKC. Additional steric constraints may explain why P2X3 receptors also do not serve as PKC substrates, despite lacking the proline in P+1. The exact role of the TXR/K motif awaits further clarification.
Abbreviations
- ATP:
-
adenosine 5′-triphosphate
- αβ-meATP:
-
α,β-methylene adenosine 5′-triphosphate
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- DMSO:
-
dimethyl sulfoxide
- EGFP:
-
enhanced green fluorescent protein
- HEK293:
-
human embryonic kidney cell line
- mGluR1α:
-
metabotropic glutamate receptor subtype 1α
- PBS:
-
phosphate-buffered saline
- PBST:
-
0.1% Tween 20 in phosphate-buffered saline
- PKC:
-
protein kinase C
- PMA:
-
phorbol 12-myristate 13-acetate
- PMSF:
-
phenylmethylsulfonyl fluoride
- PVDF:
-
polyvinylidene fluoride
- SF3B1:
-
splicing factor 3b subunit 1
References
Burnstock G (2004) Introduction: P2 receptors. Curr Top Med Chem 4:793–803
North RA (2002) Molecular physiology of P2X receptors. Physiol Rev 82:1013–1067
Aschrafi A, Sadtler S, Niculescu C et al (2004) Trimeric architecture of homomeric P2X2 and heteromeric P2X1+2 receptor subtypes. J Mol Biol 342:333–343
Barrera NP, Ormond SJ, Henderson RM et al (2005) Atomic force microscopy imaging demonstrates that P2X2 receptors are trimers but that P2X6 receptor subunits do not oligomerize. J Biol Chem 280:10759–10765
Jiang LH, Kim M, Spelta V et al (2003) Subunit arrangement in P2X receptors. J Neurosci 23:8903–8910
Khakh BS, Burnstock G, Kennedy C et al (2001) International union of pharmacology. XXIV. Current status of the nomenclature and properties of P2X receptors and their subunits. Pharmacol Rev 53:107–118
Mio K, Kubo Y, Ogura T et al (2005) Visualization of the trimeric P2X2 receptor with a crown-capped extracellular domain. Biochem Biophys Res Commun 337:998–1005
Nicke A, Bäumert HG, Rettinger J et al (1998) P2X1 and P2X3 receptors form stable trimers: a novel structural motif of ligand-gated ion channels. EMBO J 17:3016–3028
Gever JR, Cockayne DA, Dillon MP et al (2006) Pharmacology of P2X channels. Pflugers Arch 452:513–537
Burnstock G (2005) Purinergic P2 receptors as targets for novel analgesics. Pharmacol Ther 110:433–454
Chizh BA, Illes P (2001) P2X receptors and nociception. Pharmacol Rev 53:553–568
Jarvis MF (2003) Contributions of P2X3 homomeric and heteromeric channels to acute and chronic pain. Expert Opin Ther Targets 7:513–522
Kennedy C, Assis TS, Currie AJ et al (2003) Crossing the pain barrier: P2 receptors as targets for novel analgesics. J Physiol 553:683–694
North RA (2004) P2X3 receptors and peripheral pain mechanisms. J Physiol 554:301–308
North RA (2003) The P2X3 subunit: a molecular target in pain therapeutics. Curr Opin Investig Drugs 4:833–840
Paukert M, Osteroth R, Geisler HS et al (2001) Inflammatory mediators potentiate ATP-gated channels through the P2X3 subunit. J Biol Chem 276:21077–21082
Chen Y, Li GW, Wang C et al (2005) Mechanisms underlying enhanced P2X receptor-mediated responses in the neuropathic pain state. Pain 119:38–48
Fabbretti E, D’Arco M, Fabbro A et al (2006) Delayed upregulation of ATP P2X3 receptors of trigeminal sensory neurons by calcitonin gene-related peptide. J Neurosci 26:6163–6171
Boue-Grabot E, Archambault V, Seguela P (2000) A protein kinase C site highly conserved in P2X subunits controls the desensitization kinetics of P2X2 ATP-gated channels. J Biol Chem 275:10190–10195
Ennion SJ, Evans RJ (2002) P2X1 receptor subunit contribution to gating revealed by a dominant negative PKC mutant. Biochem Biophys Res Commun 291:611–616
Brown DA, Yule DI (2007) Protein kinase C regulation of P2X3 receptors is unlikely to involve direct receptor phosphorylation. Biochim Biophys Acta 1773:166–175
Gloor S, Pongs O, Schmalzing G (1995) A vector for the synthesis of cRNAs encoding Myc epitope-tagged proteins in Xenopus laevis oocytes. Gene 160:213–217
de Graaf K, Czajkowska H, Rottmann S et al (2006) The protein kinase DYRK1A phosphorylates the splicing factor SF3b1/SAP155 at Thr434, a novel in vivo phosphorylation site. BMC Biochem 7:7
Schmalzing G, Gloor S, Omay H et al (1991) Up-regulation of sodium pump activity in Xenopus laevis oocytes by expression of heterologous β1 subunits of the sodium pump. Biochem J 279:329–336
Duckwitz W, Hausmann R, Aschrafi A et al (2006) P2X5 subunit assembly requires scaffolding by the second transmembrane domain and a conserved aspartate. J Biol Chem 281:39561–39572
Borowski P, Resch K, Schmitz H et al (2000) A synthetic peptide derived from the non-structural protein 3 of hepatitis C virus serves as a specific substrate for PKC. Biol Chem 381:19–27
Rettinger J, Schmalzing G (2003) Activation and desensitization of the recombinant P2X1 receptor at nanomolar ATP concentrations. J Gen Physiol 121:451–461
Rettinger J, Schmalzing G (2004) Desensitization masks nanomolar potency of ATP at the P2X1 receptor. J Biol Chem 279:6426–6433
Hausmann R, Rettinger J, Gerevich Z et al (2006) The suramin analog 4,4′,4″,4′′′-(carbonylbis(imino-5,1,3-benzenetriylbis (carbonylimino)))tetra-kis-benzenesulfonic acid (NF110) potently blocks P2X3 receptors: subtype selectivity is determined by location of sulfonic acid groups. Mol Pharmacol 69:2058–2067
Adrian RH, Almers W (1974) Membrane capacity measurements on frog skeletal muscle in media of low ion content. J Physiol 237:573–605
Vasilets LA, Schmalzing G, Mädefessel K et al (1990) Activation of protein kinase C by phorbol ester induces downregulation of the Na+/K+-ATPase in oocytes of Xenopus laevis. J Membr Biol 118:131–142
Schmalzing G, Richter H-P, Hansen A et al (1995) Involvement of the GTP binding protein Rho in constitutive endocytosis in Xenopus laevis oocytes. J Cell Biol 130:1319–1332
Levitan IB (1999) Modulation of ion channels by protein phosphorylation. How the brain works. Adv Second Messenger Phosphoprotein Res 33:3–22
Liu GJ, Brockhausen J, Bennett MR (2003) P2X1 receptor currents after disruption of the PKC site and its surroundings by dominant negative mutations in HEK293 cells. Auton Neurosci 108:12–16
Jensik P, Cox T (2002) ATP-induced internalization of amphibian epithelial P2X receptors is linked to channel opening. Pflugers Arch 444:795–800
Vial C, Tobin AB, Evans RJ (2004) G-protein-coupled receptor regulation of P2X1 receptors does not involve direct channel phosphorylation. Biochem J 382:101–110
He ML, Zemkova H, Koshimizu TA et al (2003) Intracellular calcium measurements as a method in studies on activity of purinergic P2X receptor channels. Am J Physiol Cell Physiol 285:C467–C479
Chow YW, Wang HL (1998) Functional modulation of P2X2 receptors by cyclic AMP-dependent protein kinase. J Neurochem 70:2606–2612
Wirkner K, Stanchev D, Koles L et al (2005) Regulation of human recombinant P2X3 receptors by ecto-protein kinase C. J Neurosci 25:7734–7742
Stanchev D, Flehmig G, Gerevich Z et al (2006) Decrease of current responses at human recombinant P2X3 receptors after substitution by Asp of Ser/Thr residues in protein kinase C phosphorylation sites of their ecto-domains. Neurosci Lett 393:78–83
Zhu G, Fujii K, Belkina N et al (2005) Exceptional disfavor for proline at the P+1 position among AGC and CAMK kinases establishes reciprocal specificity between them and the proline-directed kinases. J Biol Chem 280:10743–10748
Huang KP, Huang FL (1986) Conversion of protein kinase C from a Ca2+-dependent to an independent form of phorbol ester-binding protein by digestion with trypsin. Biochem Biophys Res Commun 139:320–326
Acknowledgement
We gratefully acknowledge helpful discussions with our colleague Dr. Walter Becker and his gift of the EGFP-tagged SF3B1 splicing factor plasmid. This research project was supported by the START-Program of the Faculty of Medicine, RWTH Aachen University to R.H. and a grant of the Deutsche Forschungsgemeinschaft (FOR450, TP 11) to G.S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Franklin, C., Braam, U., Eisele, T. et al. Lack of evidence for direct phosphorylation of recombinantly expressed P2X2 and P2X3 receptors by protein kinase C. Purinergic Signalling 3, 377–388 (2007). https://doi.org/10.1007/s11302-007-9067-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-007-9067-x