Abstract
The aim of this study has been to determine the incidence of diverse human rotavirus strains circulating in Thailand between October 2004 and April 2006 by means of molecular characterization. Pediatric patients aged between 2 months and 5 years diagnosed with acute diarrhea (n = 307) in Bangkok and Buriram, Thailand were tested for human rotavirus A (RV-A) by RT-PCR. A total of 130 specimens (42.3%) were found RV-A positive and 126 were characterized by direct sequencing of the capsid glycoproteins VP7 and VP4. BLAST/FASTA analysis and phylogenetic analysis revealed genotypes G1P[8] (85.7%), G2P[4] (2.4%), G2P[8] (0.8%), G3P[8] (1.6%), G9P[8] (8.7%), and the uncommon strain G3P[19] (0.8%). Varying sites of polymorphism over time imply dependence on geographical location along with seasonal variation of relative incidence and distribution of rotavirus types. Thus, continuous molecular monitoring of human rotavirus epidemiology is essential for adjusting vaccine development.
Similar content being viewed by others
Introduction
Rotavirus infections are the major cause of acute diarrhea in humans and animals throughout the world. Global surveillance performed from 2000 to 2004 indicated that rotavirus causes 39% (range 29–45%) of childhood diarrhea hospitalizations, and 611,000 (range 454,000–705,000) deaths of children worldwide [1]. Rotaviruses belong to the Reoviridae family and comprise a non-enveloped, triple-layered protein capsid enclosing 11 segments of double stranded RNA. They are classified into groups A–G, but only groups A, B, and C have been identified in humans [2]. To distinguish between types within group A, two classification systems have been established to define the G types based on glycoprotein VP7, and the P types based on the protease-sensitive protein VP4 [3]. At least 15 G types and in excess of 27 P types have been distinguished, of which at least 10 G types and 11 P types have been found in humans [4–6].
In recent years, rotavirus genotyping by reverse transcription-polymerase chain reaction (RT-PCR) and direct sequencing has provided valuable information about the genetic diversity of rotaviruses circulating worldwide, and has led to the discovery of much greater strain diversity than had previously been acknowledged based on serological typing methods. Molecular methods have allowed the detection of rotavirus types such as G5, G6, G8, G9, G10, G12, P[6], P[9], and P[11] not previously found in human infections [7–9].
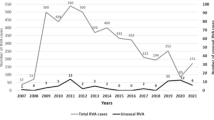
Rotavirus is the principal pathogen responsible for about one-third of children hospitalized with diarrhea in Thailand. Prior to 2000, G1 had been the predominant serotype in Thailand, although occasionally other serotypes such as G4 and G2 were found. A review of nine studies performed in Thailand between 1982 and 1997 revealed that the rotavirus serotype distribution was 37.8% for G1, 21.8% for G2, 2.5% for G3, 7.0% for G4, and 0.4% for G9 serotypes [10]. Serotype G9 is becoming more common in Thailand. Surveillance conducted in different geographical areas of Thailand during 2001–2003 demonstrated that the prevalence of G9, G2, G4, G1, and G3 was 54.8, 17.2, 5.3, 0.8, and 0.1%, respectively [11]. In a recent study in Bangkok, G1 was predominant during 1998–1999 and 2004–2006, whereas G2 was more prevalent during 2002–2004 [12].
Re-assortment among co-circulating strains contributes considerably to the overall genomic diversity of rotaviruses. The gene segments encoding VP7 and VP4 can segregate independently during re-assortment and thus, different G- and P-type combinations can be found in co-circulating rotaviruses. Interspecies transmission and more importantly, exchange of genetic material between animal and human strains through re-assortment can lead to the emergence of novel rotavirus strains of epidemiological significance. Surveillance of rotavirus types in different parts of the world is essential to monitor the emergence of new types or of new G/P combinations, which may emerge over time. The efficacy of any future rotavirus vaccine may depend on the predominant natural strain types [13]. Prior to vaccine introduction into target populations, it is essential to gather epidemiological and molecular surveillance data of rotavirus infection in each individual country.
The objectives of this study have been to characterize and determine the incidence of human rotavirus strains circulating in Thailand.
Materials and methods
Study population
The study protocol was approved by the Ethics Committee of the Faculty of Medicine, Chulalongkorn University and the Buriram Provincial Hospital, Buriram, Thailand. The parents of all pediatric patients were informed as to the study details and their written consent was obtained before specimen collection.
The specimens comprised 307 fecal samples from 161 boys and 146 girls aged between 2 months and 5 years admitted with acute diarrhea to the Department of Pediatrics, Faculty of Medicine, Chulalongkorn University and Hospital (n = 192, from October 2004 to April 2006) and the provincial hospital of Buriram (n = 115, between October 2005 and January 2006), a province 410 km to the northeast of Bangkok. The specimens were kept at −70°C until further examination.
Rotavirus RNA detection
Fecal specimens were diluted 1:10 in PBS (phosphate buffered saline), centrifuged, and the supernatant was analyzed for rotavirus RNA by RT-PCR. Briefly, RNA was extracted from 50 μl of each diluted specimen by the guanidium-isothiocyanate method as described elsewhere [14], and subsequently reverse transcribed into cDNA using primer End 9: 5′ GGTCACATCATACAATTCTAATCTAAG 3′ (nt 1062–1036) for the VP7 gene and Con2: 5′ ATTTCGGACCATTTATAACC 3′(nt 887–868) for the VP4 gene. The resulting cDNA was PCR amplified using primer Beg9: 5′-GGCTTTAAAAGAGAGAATTTCCGTCTGG-3′ (nt 1–28) [15] as a sense primer and End 9 as an antisense primer for the VP7 gene. For the VP4 gene, Con3 5′ TGGCTTCGCTCATTTATAGACA 3′ was used as a sense primer and Con2 as an antisense primer [16]. For both genes, the PCR was performed in a model 9600 thermocycler (Perkin Elmer Cetus, Norwalk, CT) as follows: initial denaturation at 95°C for 3 min, followed by 30 cycles each of 1 min at 95°C for denaturation, 1 min at 60°C for primer annealing, and 1 min at 72°C for extension and concluded by a final extension step at 72°C for 10 min. After electrophoresis in a 2% agarose gel stained with Ethidium bromide, the expected 1062 and 876 bp-bands for the VP7 and VP4 product, respectively, were visualized on a UV trans-illuminator (Gel Doc 1000, BIO-RAD, CA).
Rotavirus sequencing
The PCR products were purified for sequencing by using the Perfectprep Gel Cleanup Kit (Eppendorf, Westbuty, NY) according to the manufacturer’s specifications and purity was ascertained by gel electrophoresis in 2% agarose. The concentration of purified DNA was determined by measuring absorption at 260 nm with a UV spectrophotometer (Shimadzu UV 160 A, Tokyo, Japan). Between 30 and 180 ng of each DNA sample was subjected to double stranded sequencing using the dideoxy-nucleotide chain termination method with the Big Dye Terminator V.3.1 Cycle Sequencing Ready Reaction kit (ABI Fostercity, CA) and 0.16 μM final concentration of sequencing primers (Beg9 and End9 for amplicon VP7, Con2 and Con3 for amplicon VP4) in a model 9600 thermocycler (Perkin Elmer Cetus, Norwalk, CT) as described previously [12]. The extension products were subsequently purified from excess unincorporated dye terminators by ethanol precipitation according to the manufacturer’s specifications (ABI Sequencing kit, ABI, Fostercity, CA) and subjected to sequence analysis by the ABI Prism 310 Genetic Analyser. (ABI, Fostercity, CA).
All subsequent steps were performed according to the ABI Prism 310 Genetic Analyser user’s manual. All sequences were submitted to the GenBank database.
Rotavirus genotype and sequence analysis
The genotype(s) were determined by BLAST/FASTA (http://www.ncbi.nlm.nih.gov) and phylogenetic analysis. The sequences were edited and assembled by using programs CHROMAS LITE v.2.0 (http://www.mb.mahidol.ac.th/pub/chromas/chromas.htm) and SeqMan (DNASTAR, Madison, WI). To investigate the relationship between rotaviruses strains, the un-rooted tree topology based on multiple alignments of the VP7 and VP4 nucleotide sequences and those of known genotype from Genbank (VP7 genotypes G1–G15 and VP4 genotypes P[1]–P[23]) was established by the neighbor-joining method calculated with MEGA3.1 (http://www.megasoftware.net). Consistency of branching was tested by bootstrap analysis of 1000 re-sampled data using MEGA 3.1. Multiple protein translations and sequence alignments were generated with BioEdit version 7.0.1 (http://www.mbio.ncsu.edu/BioEdit/bioedit.html).
All newly sequenced strains were grouped and compared with the reference strains. Furthermore, we compared the sequences with those obtained during our previous comparative studies on genetic changes and genotypes circulating during 1998–1999 [17], 2002–2004 [12].
Results
Rotavirus RNA detection
During the period of this study (October 2004–April 2006), stool specimens of 130 (69 male, 61 female) out of 307 patients with acute diarrhea (42.3%) were found positive for rotavirus RNA by RT-PCR. The prevalence of rotavirus decreased with increasing age of the children tested. Direct sequencing was performed on 126 rotavirus RNA positive fecal specimens. The subtypes of 126 strains yielding amplicons of 1062 and 876 bp in size representing the VP7 and VP4 genes were identified from their sequences. The nucleotide sequences obtained from this study have been submitted to the GenBank database under accession numbers: VP4 sequences; DQ235956-75, DQ235977-85, DQ235988-6000, DQ236002-09, DQ236011, DQ674935-5009; VP7 sequences; DQ236013-17, DQ236019, DQ236021, DQ236024, DQ236026-30, DQ236032-36, DQ236038-41, DQ236043-44, DQ236048, DQ236050-71, DQ236073-76, DQ674860-934.
Rotavirus genotype analysis
Upon BLAST/FASTA analysis, 108 strains were characterized as G1P[8], 3 as G2P[4], 1 as G2P[8], 2 as G3P[8], 11 as G9P[8], and 1 as the uncommon strain G3P[19] (Table 1). This uncommon strain (DQ674932) showed 87% and 86% aa identity with a rhesus and equine rotavirus strain, respectively, by BLAST analysis. Figures 1 and 2 depict the phylogenetic relationships determined for VP7 and VP4, which include previously published sequences for comparison. These phylogenetic relationships also demonstrate that the rotavirus strains determined in the course of this study belonged to genotypes G1P[8], G2P[4], G2P[8], G3P[8], G9P[8], and the rare G3P[19] strain. For clarification, the regions of reconstruction containing each genotype G1, G2, G3, G9 have been expanded and shown separately (Fig. 3). Phylogenetic analysis of the G1 sequences was compared with a selection of G1 VP7 sequences. The G1 RVs sequences circulating in Thailand from 1999 to 2004 clustered in the same lineage and showed 99–100% nt identity among groups by BLAST/FASTA analysis. The samples in group G1 clustered in the same lineage as some strains isolated in Italy during 2002–2004 and provided the best match with isolate PA9/03 (DQ377597) with 98% nt identity by BLAST analysis. As for G2, the studied sequences (DQ236015-16, DQ236069, DQ236075) clustered with those of strains obtained in Thailand during 2002–2004 (AY456232-37, AY456239, AY456241-44, AY707784-6) and Italy in 2003 (DQ172853-56), which provided the best match of 98–100% nt identity with strain 1-003 (DQ172853) and strain 32g2 (AY456236). As for G3, the sequences (DQ674933-4) clustered with those of isolates from the northern part of Thailand in 2004 (AY707793-4) and provided the best match with strain CMH 055 displaying 99% nt identity. As for G9, the sequences of sample group a and DQ236062 clustered in the same sub-lineage as the strains obtained from Thailand between 1995 and 1997(AY866501-5) and in 2003 (AY456227-31) which showed the best match of 98–99% nucleotide identity by BLAST/FASTA analysis with strain 97CM86 and strain 62g9. The second sub-lineage comprising sequences determined in this study (DQ236060, DQ236064, and DQ036067) and the strains from Hungary obtained during 1998–2001(AJ605303-11) proved the best match with isolate BC4572/00 showing 98% nucleotide identity. The VP7 sequence of an uncommon strain (DQ 674932) by BLAST/FASTA analysis displayed the highest identity to a rhesus and equine rotavirus strain (87% nt and 86% nt) and was characterized as G3. Interestingly, upon sequence analysis of VP4, this strain displayed the rare P[19] specificity, thus revealing the uncommon G/P combination G3P[19].
The phylogenetic relationships determined for VP7, including previously published sequences as follows: D16343 for G1; AB118023 for G2; AY707794 for G3; AF480280 for G4; L35079 for G5; AF162435for G6; X56784 for G7; AF545860 for G8; and L14072 for G9; AY855063 for G10; AY773003 for G11; AB186120 for G12; D13549 for G13; AY750923 for 14 and AF237666 for G15
The phylogenetic relationships determined for VP4, including previously published sequences as follows: D13395 for P[1]; M23188 for P[2]; M18736 for P[3]; M58292 for P[4]; M22306 for P[5]; M33516 for P[6]; X13190 for P[7]; M21014 for P[8]; D90260 for P[9]; M60600 for P[10]; D13394 for P[11]; L04638 for P[12]; L07886 for P[13]; D14724 for P[14]; L11599 for P[15]; U08429 for P[16]; D16352 for P[17]; D13399 for P[18]; D38052 for P[19]; U08424 for P[20]; AF237665 for P[21]; AF526376 for P[22]; and AY174094 for P[23]
Sequence analysis of VP7
Based on analysis of the partial VP7 nucleotide sequences obtained in this study, the amino acid sequence identities between strains of each genotype group range from 95.6–100% for G1, 95–99.5% for G2, 99.2% for G3 and 98.7–100% for G9. Comparison of our strains with reference strains showed identity ranges from 90.6–92.4%, 94.1–97.7%, 99.1%, and 87.5–99.4% for groups G1, G2, G3, and G9, respectively. The identity range between genotypes was 69–77%. In comparison with the reference strains, multiple mutations were predominant in the antigenically dominant VR regions of the G1, G2, G3, G4, and G9 Thai strains, as shown in Fig. 4.
Sequence analysis of VP4
The deduced amino acid sequences of the trypsin-cleaved VP8* product of VP4 of the strains under examination were compared with representative reference sequences of isolate B4633-03 (DQ146641) for P[8], strain Dhaka116-00 (DQ492659) for P[4]). The partial VP4 gene sequence studied contains 789 nucleotides; comparing our sequences with the reference strains, the best match for the P[4] strain is Dhaka116-00 (DQ492659) demonstrating 98.1% nt identity and the best match for P[8] is isolate B4633-03 (DQ146641) with 99% nt identity. The P[8] samples examined were also identical to P[8] specimens circulating in Thailand over the previous years and proved similar to P[8] RVs circulating in other countries with 98–99% nt identity by BLAST. The P[8] lineage shared by the G1, G2, G3, and G9 types showed 99–100% nt identity by BLAST anslysis.
The uncommon strain was classified as P[19] genotype by BLAST/FASTA analysis and phylogenetic analysis, which showed 95% nucleotide identity with the reference isolate RMC321 (AF523677). Amino acid comparisons between VP8* and P[19] (AF523677), P[3] (AJ311735), and P[8] (DQ674936) are shown in Fig. 5. In addition, some polymorphisms were found in P[4] at amino acid positions I35V, R51G, R111H, I120V, I130V, N133S, N150D, and V199I and in P[8] at positions V35I, K75T, L77P, V91I, V106I, I108V, I113D, N, Q114P, T120N, E150D, K162R, D195G, V, I199T, K245T, and V249I. Conservation of the trypsin cleavage site and the proline residues has been observed in this study and with most rotavirus strains [20].
Discussion
The predominant human rotavirus strain detected in Thailand between November 1998 and August 1999 was genotype G1 (83.3%) [17], whereas between November 2002 and March 2004, G2 prevailed (69.4%) [12]. This study revealed an 85.7% frequency of G1P[8], 2.4% of G2P[4], 0.8% of G2P[8], 1.6% of G3P[8], 0.8% of G3P[19], and 8.7% of G9P[8]. The distribution of predominant G serotypes apparently depends on the year of infection and the G1 rotavirus strain was predominant during a 2–3 year cycle, whereupon other types prevailed [10, 17]. This was similar to the results of a 4-year survey on rotavirus infection conducted from 1996 to 2000, which revealed a changing G genotype distribution pattern in Japan with a decrease of G1 and increase of G9 and G2 [19].
Coinciding with a global emergence, the prevalence of G9 rotavirus has increased in Thailand during 1998–2005. The G9 serotype was first isolated in 1989 from children in Chiang Mai, a province in the North of Thailand [18, 21]. The serotype G9 strain emerged as the third major serotype after G1 and G2 with a frequency of 16.2% among specimens collected in Chiang Mai between 1996 and 1997 [22]. During 2000–2001, genotype G9 was identified in 91.6% of the strains tested in this province [23]. G9 genotype has also been reported as a common genotype causing diarrhea in children in India [24].
Strains of the same lineage were detected during different years, even after long-time intervals. This may suggest continuous circulation across various geographical regions and re-emergence of previous strains at a new location [25]. The VP7 gene of both G9 strains in this study and G9 from the previous study [12] clustered in a sub-lineage different from the lineage containing strains obtained from the northern part of Thailand during 1995–1997, but all clustered in the P[8] branch (Fig. 2). The uncommon strain isolated in this study belonged to G3 according to BLAST/FASTA analysis, but showed up as an unusual strain by phylogenetic analysis sharing 87% amino acid identity with a rhesus strain (AF295303) and 86% with an equine strain (AY750924). This virus may have arisen from multiple, independent re-assortment events involving rhesus or equine rotavirus genes. It is thought that different lineages may be under varying selective pressure and evolve at alternate rates, reaching an evolutionary stasis when completely adapted to their host [26, 27]. The results presented here are consistent with other epidemiology studies [28–30], which have indicated that since the mid 1980s, unclassified serotypes have been emerging globally.
Between 1989 and 2004, the global distribution of the P and G types of rotavirus group A among children worldwide amounted to G1P[8] 64%, G3P[8] 3%, G4P[8] 9%, G2P[4] 12%, G2P[8] 2.5%, and G9P[8], representing 4.1% of global infection [31]. An unclassified strain of rotaviruses with long electropherotype which predominated in the outbreak of infantile gastroenteritis in India during 1987–1988 displayed G9P[19] specificity [32]. Most of that strain’s nucleotide sequences including VP6 and NSP4 were intimately related to porcine rotaviruses and were still circulating during subsequent epidemiological studies conducted within the same population from 1989 to 1992 [33, 34].
Amino acid comparison between VP7 of the Japanese G1 strain KU and the Thai G1 strain (between 1998 and 2006) is shown in Fig. 4. The amino acid sequences of rotavirus strain G1 were nearly identical except for 3-point mutations discovered in 10 strains of this study (2005) at positions Q28R, A46V, and Q72R. On the other hand, G2 amino acid sequence alignment with prototype HRV reference strain DS-1 (AB118023) showed five amino acid changes of S15F in VR1, I44M in VR3, D96N in VR5, N122S in VR6 and V281, which are fairly typical for the Thai strain.
The amino acid sequences of the G3 strains in this study are almost identical, but the uncommon strain proved similar to a rhesus and equine strain. In a previous study in India, a child has been reported infected with both simian SA11-human re-assorted, G3P[8] and AU 32 G9P[8] rotavirus strains [35]. Khamrin et al. also reported a re-assorted strain of human rotavirus G3P[3], containing simian-like VP7 and caprine-like VP4 genes isolated from a child in Chiang Mai [36]. These findings provide additional evidence for the increasing genetic/antigenic diversity of group A rotaviruses in nature which is crucial for understanding rotavirus re-assortment [37].
Comparison between the amino acid sequences of the G9 strains from our study conducted in 2002–2004 and the reference strains 116E (L14072; vaccine strain in India (phase I), WI61 and AU32 (prototype G9 strain of 1985) [38] showed approximately 88% nucleotide identity. Comparison between our study and the human reference strain 95H115 which had re-emerged among rotaviruses recovered from Japanese children hospitalized in 1995 (and not evolved from AU32) [38] showed 98% identity. Although the reference and study samples belonged to the same strain, they still displayed low amino acid identity with the prototype. This may be due to geographically specific infection over time and the relative incidence and distribution of rotavirus types varying between geographical areas during a rotavirus season and from one season to the next, very similar to the molecular epidemiology of influenza A virus. As shown in Fig. 4, during 2002 and 2003, the point mutations of interest relative to the above references are found in VR3 at position P46S and in VR5 at T101I, during 2003 and 2004, at positions F106 L and A181T. The first amino acid change (aa 46) shown by this alignment appears in all strains from 2002 to 2005 and hence, may be typical for the Thai strain. The second amino acid change is evident among strains from 2002 to 2004 but does not appear among the more recent ones and thus, may depend on the year of infection. The remaining two changes at F106L and A181T have only been found among recent strains and could imply mutations specific for the Thai strain, but still require additional sequence studies in order to confirm that. The glycosylation site at aa 69–71 in VR4 and peptide cleavage site at aa 50 in VR3 are conserved in the G1, G2, and G9 genotypes of the Thai strain from 1998–2006.
Surveillance of rotavirus types in different parts of the world is essential to monitor the emergence of new types or of new G/P combinations, which may predominate over time. Since the vaccine can protect, to a lesser extent, against rotavirus strains that do not share G or P epitopes with the vaccine strains, understanding the differences between the epidemiological features of rotaviruses in developing and developed countries is essential for designing optimal rotavirus immunization programs.
Abbreviations
- RT-PCR:
-
Reverse transcription-polymerase chain reaction
- MEIA:
-
Monoclonal antibody-based enzyme immunoassay
References
U.D. Parashar, C.J. Gibson, J.S. Bresee, R.I. Glass, Emerg. Infect. Dis. 12, 304–306 (2006)
A.F. Manuel, H.B. Greenberg, in Clinical Virology, (2nd edn) ed. by D.D. Richman, R.J. Whitley, F.G. Hayden, (ASM Press, Washington, DC, 2002), pp. 743–762
M. Estes, in Field Virology, (3rd edn), ed. by B.N. Fields (Lippincott-Raven, Philadelphia, PA, 1996), pp. 1625–1655
U. Desselberger, M. Iturriza-Gomara, J.J. Gray, Rotavirus epidemiology and surveillance. Novartis Found Symp. 238, 125–147 (2001) discussion 147–152
A.Z. Kapikian, Y. Hoshino, R.M. Chanock, in Field Virology, (4th edn), ed. by D.M. Knipe (Lippincott-Williams, Philadelphia, PA, 2001), pp. 1787–1833
V. Martella, M. Ciarlet, K. Banyai, E. Lorusso, A. Cavalli, M. Corrente, G. Elia, S. Arista, M. Camero, C. Desario, N. Decaro, A. Lavazza, C. Buonavoglia, Virology 346, 301–311 (2006)
V. Gouvea, L. de Castro, M.C. Timenetsky, H. Greenberg, N. Santos, J. Clin. Microbiol. 32, 1408–1409 (1994)
Y. Pongsuwanna, R. Guntapong, M. Chiwakul, R. Tacharoenmuang, N. Onvimala, M. Wakuda, N. Kobayashi, K. Taniguchi, J. Clin. Microbiol. 40, 1390–1394 (2002)
A.D. Steele, B. Ivanoff, Vaccine 17, 361–367 (2003)
N. Maneekarn, H. Ushijima, Pediatr. Int. 42, 415–421 (2000)
C. Jiraphongsa, J.S. Bresee, Y. Pongsuwanna, P. Kluabwang, U. Poonawagul, P. Arporntip, M. Kanoksil, N. Premsri, U. Intusoma, J. Infect. Dis. 192(Suppl 1), S87–S93 (2005)
A. Theamboonlers, M. Veravigrom, O. Yambangyang, P. Trairatvorakul, V. Chongsrisawat, Y. Poovorawan, Acta Virol. 49, 111–115 (2005)
G.M. Ruiz-Palacios, I. Perez-Schael, F.R. Velazquez, H. Abate, T. Breuer, S.C. Clemens, B. Cheuvart, F. Espinoza, P. Gillard, B.L. Innis, Y. Cervantes, A.C. Linhares, P. Lopez, M. Macias-Parra, E. Ortega-Barria, V. Richardson, D.M. Rivera-Medina, L. Rivera, B. Salinas, N. Pavia-Ruz, J. Salmeron, R. Ruttimann, J.C. Tinoco, P. Rubio, E. Nunez, M.L. Guerrero, J.P. Yarzabal, S. Damaso, N. Tornieporth, X. Saez-Llorens, R.F. Vergara, T. Vesikari, A. Bouckenooghe, R. Clemens, B. De Vos, M. O’Ryan, N. Engl. J. Med. 354, 11–22 (2006)
T.A. Cha, J. Kolberg, B. Irvine, M. Stempien, E. Beall, M. Yano, Q.L. Choo, M. Houghton, G. Kuo, J.H. Han, M.S. Urdea, J. Clin. Microbiol. 29, 2528–2534 (1991)
V. Gouvea, R.I. Glass, P. Woods, K. Taniguchi, H.F. Clark, B. Forrester, Z.Y. Fang, J. Clin. Microbiol. 28, 276–282 (1990)
J.R. Gentsch, R.I. Glass, P. Woods, V. Gouvea, M. Gorziglia, J. Flores, B.K. Das, M.K. Bhan, J. Clin. Microbiol. 30, 1365–1373 (1992)
S. Noppornpanth, A. Theamboonlers, Y. Poovorawan, Asian Pac. J. Allergy Immunol. 19, 49–53 (2001)
S. Urasawa, A. Hasegawa, T. Urasawa, K. Taniguchi, F. Wakasugi, H. Suzuki, S. Inouye, B. Pongprot, J. Supawadee, S. Suprasert, J. Infect. Dis. 166, 227–234 (1992)
Y. Zhou, L. Li, S. Okitsu, N. Maneekarn, H. Ushijima, Microbiol. Immunol. 47, 591–599 (2003)
V. Martella, M. Ciarlet, R. Baselga, S. Arista, G. Elia, E. Lorusso, K. Banyai, V. Terio, A. Madio, F.M. Ruggeri, E. Falcone, M. Camero, N. Decaro, C. Buonavoglia, Virology 337, 111–123 (2005)
J. Okada, T. Urasawa, N. Kobayashi, K. Taniguchi, A. Hasegawa, K. Mise, S. Urasawa, J. Med. Virol. 60, 63–69 (2000)
Y. Zhou, J. Supawadee, C. Khamwan, S. Tonusin, S. Peerakome, B. Kim, K. Kaneshi, Y. Ueda, S. Nakaya, K. Akatani, N. Maneekarn, H. Ushijima, J. Med. Virol. 65, 619–628 (2001)
P. Khamrin, S. Peerakome, L. Wongsawasdi, S. Tonusin, P. Sornchai, V. Maneerat, C. Khamwan, F. Yagyu, S. Okitsu, H. Ushijima, N. Maneekarn, J. Med. Virol. 78, 273–280 (2006)
M. Ramachandran, B.K. Das, A. Vij, J. Clin. Microbiol. 34, 436–439 (1996)
S. Arista, G.M. Giammanco, S. De Grazia S. Ramirez, C. Lo Biundo, C. Colomba, A. Cascio, V. Martella, J. Virol. 80, 10724–10733 (2006)
K. Banyai, V. Martella, F. Jakab, B. Melegh, G. Szucs, J. Clin. Microbiol. 42, 4338–4343 (2004)
N. Maneekarn, P. Khamrin, W. Chan-it, S. Peerakome, S. Sukchai, K. Pringprao, H. Ushijima, J. Clin. Microbiol. 44, 4113–4119 (2006)
N. Santos, R.C. Lima, C.F. Pereira, V. Gouvea, J. Clin. Microbiol. 36, 2727–2729 (1998)
M. Ramachandran, C.D. Kirkwood, L. Unicomb, N.A. Cunliffe, R.L. Ward, M.K. Bhan, H.F. Clark, R.I. Glass, J.R. Gentsch, Virology 278, 436–444 (2000)
N.A. Cunliffe, J.S. Gondwe, S.M. Graham, B.D. Thindwa, W. Dove, R.L. Broadhead, M.E. Molyneux, C.A. Hart, J. Clin. Microbiol. 39, 836–843 (2001)
N. Santos, Y. Hoshino, Rev. Med. Virol. 15, 29–56 (2005)
S.K. Ghosh, T.N. Naik, Epidemiol. Infect. 102, 523–530 (1989)
V. Varghese, S. Das, N.B. Singh, K. Kojima, S.K. Bhattacharya, T. Krishnan, N. Kobayashi, T.N. Naik, Arch. Virol. 149, 155–172 (2004)
T. Krishnan, B. Burke, S. Shen, T.N. Naik, U. Desselberger, Arch. Virol. 134, 279–292 (1994)
P.S. Awachat, S.D. Kelkar, J. Med. Virol. 78, 134–138 (2006)
P. Khamrin, N. Maneekarn, S. Peerakome, F. Yagyu, S. Okitsu, H. Ushijima, J. Med. Virol. 78, 986–994 (2006)
V. Martella, M. Ciarlet, A. Camarda, A. Pratelli, M. Tempesta, G. Greco, A. Cavalli, G. Elia, N. Decaro, V. Terio, G. Bozzo, M. Camero, C. Buonavoglia, Virology 314, 358–370 (2003)
T. Nakagomi, O. Nakagomi, Microbiol. Immunol. 46, 575–578 (2002)
Acknowledgments
We are grateful to the Thailand Research Fund, Senior Research Scholar, Center of Excellence in Viral Hepatitis Fund, and the Department of Microbiology, Faculty of Medicine, Chulalongkorn University. Also, we would like to express our gratitude to the entire staff of the Center of Excellence in Viral Hepatitis, Chulalongkorn University and the staff from Buriram Hospital for their efforts in contributing to the present study, Ms. Petra Hirsch and Dr. Philip Shaw for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Theamboonlers, A., Bhattarakosol, P., Chongsrisawat, V. et al. Molecular characterization of group A human rotaviruses in Bangkok and Buriram, Thailand during 2004–2006 reveals the predominance of G1P[8], G9P[8] and a rare G3P[19] strain. Virus Genes 36, 289–298 (2008). https://doi.org/10.1007/s11262-008-0201-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11262-008-0201-9