Abstract
Background
Sacubitril/valsartan, a new pharmacological class of angiotensin receptor neprilysin inhibitor, is beneficial to heart failure through blocking the degradation of natriuretic peptides and inhibiting renin–angiotensin–aldosterone system (RAAS) activation which also relate to the pathophysiologic mechanisms of chronic kidney disease (CKD). However, its effects on CKD remain unclear. To assess the efficacy and safety of sacubitril/valsartan for patients with CKD, we performed this meta-analysis.
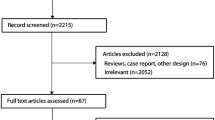
Methods
The Embase, PubMed and the Cochrane Library were searched for randomized controlled trials (RCTs) that compared sacubitril/valsartan with ACEI/ARBs in patients with CKD whose estimated glomerular filtration rate (eGFR) was below 60 mL/min/1.73 m2. We adopted the Cochrane Collaboration tool for assessing the risk of bias. The effect size was estimated using the odds ratio (OR) with 95% confidence interval (CI).
Results
Six trials with a total of 6217 patients with CKD were included. In terms of cardiovascular events, sacubitril/valsartan attenuated the risk of cardiovascular death or heart failure hospitalization (OR: 0.68, 95% CI 0.61–0.76, P < 0.00001, I2 = 43%). With respect to renal function, sacubitril/valsartan prevented the incidence of serum creatinine (Scr) elevation among patients with CKD (OR: 0.79, 95% CI 0.67–0.95, P = 0.01, I2 = 0%). Subgroup analysis about eGFR demonstrated that with long follow-up, sacubitril/valsartan significantly decreased the number of patients with more than 50% reduction in eGFR compared with ACEI/ARBs (OR: 0.52, 95% CI 0.32–0.84, P = 0.008, I2 = 9%). In patients with CKD, the incidence of end-stage renal disease (ESRD) was reduced with sacubitril/valsartan treatment, despite no statistically significant difference between the two groups (OR: 0.59, 95% CI 0.29–1.20, P = 0.14, I2 = 0%). As for the safety, we found that sacubitril/valsartan was associated with the occurrence of hypotension (OR: 1.71, 95% CI 1.15–2.56, P = 0.008, I2 = 51%). However, there was no trend towards increasing the risk of hyperkalemia in patients who received sacubitril/valsartan (OR: 1.09, 95% CI 0.75–1.60, P = 0.64, I2 = 64%).
Conclusion
This meta-analysis indicated that sacubitril/valsartan improved renal function and conferred effective cardiovascular benefits in patients with CKD, without serious safety issues being observed. Thus, sacubitril/valsartan may be a promising option for patients with CKD. Certainly, further large-scale randomized controlled trials are needed to confirm these conclusions.
Systematic review registration
[https://inplasy.com/inplasy-2022-4-0045/], identifier [INPLASY202240045].








Similar content being viewed by others
References
Kuang H, Huang X, Zhou Z, Cheng X, Xu G (2021) Sacubitril/valsartan in chronic kidney disease: from pharmacological mechanism to clinical application. Eur J Pharmacol 907:174288. https://doi.org/10.1016/j.ejphar.2021.174288
Global, Regional, and National Burden of Chronic Kidney Disease, 1990–2017: a systematic analysis for the global burden of disease study 2017 (2020). Lancet (London, England) 395(10225):709–733. https://doi.org/10.1016/s0140-6736(20)30045-3
Li N, Lv D, Zhu X, Wei P, Gui Y, Liu S, Zhou E, Zheng M, Zhou D, Zhang L (2021) Effects of SGLT2 inhibitors on renal outcomes in patients with chronic kidney disease: a meta-analysis. Front Med 8:728089. https://doi.org/10.3389/fmed.2021.728089
Jankowski J, Floege J, Fliser D, Böhm M, Marx N (2021) Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation 143(11):1157–1172. https://doi.org/10.1161/circulationaha.120.050686
Kang H, Zhang J, Zhang X, Qin G, Wang K, Deng Z, Fang Y, Chen G (2020) Effects of sacubitril/valsartan in patients with heart failure and chronic kidney disease: a meta-analysis. Eur J Pharmacol 884:173444. https://doi.org/10.1016/j.ejphar.2020.173444
Xu Y, Chen Y, Zhao JW, Li C, Wang AY (2021) Effect of angiotensin–neprilysin versus renin–angiotensin system inhibition on renal outcomes: a systematic review and meta-analysis. Front Pharmacol 12:604017. https://doi.org/10.3389/fphar.2021.604017
Mc Causland FR, Lefkowitz MP, Claggett B, Anavekar NS, Senni M, Gori M, Jhund PS, McGrath MM, Packer M, Shi V, Van Veldhuisen DJ, Zannad F, Comin-Colet J, Pfeffer MA, McMurray JJV, Solomon SD (2020) Angiotensin–neprilysin inhibition and renal outcomes in heart failure with preserved ejection fraction. Circulation 142(13):1236–1245. https://doi.org/10.1161/circulationaha.120.047643
Voors AA, Gori M, Liu LC, Claggett B, Zile MR, Pieske B, McMurray JJ, Packer M, Shi V, Lefkowitz MP, Solomon SD (2015) Renal effects of the angiotensin receptor neprilysin inhibitor LCZ696 in patients with heart failure and preserved ejection fraction. Eur J Heart Fail 17(5):510–517. https://doi.org/10.1002/ejhf.232
Damman K, Gori M, Claggett B, Jhund PS, Senni M, Lefkowitz MP, Prescott MF, Shi VC, Rouleau JL, Swedberg K, Zile MR, Packer M, Desai AS, Solomon SD, McMurray JJV (2018) Renal effects and associated outcomes during angiotensin–neprilysin inhibition in heart failure. JACC Heart Fail 6(6):489–498. https://doi.org/10.1016/j.jchf.2018.02.004
Quiroga B, de Santos A, Sapiencia D, Saharaui Y, Álvarez-Chiva V (2019) Sacubitril/valsartan in chronic kidney disease, the nephrologist point of view. Nefrologia 39(6):646–652. https://doi.org/10.1016/j.nefro.2019.01.005
Haynes R, Judge PK, Staplin N, Herrington WG, Storey BC, Bethel A, Bowman L, Brunskill N, Cockwell P, Hill M, Kalra PA, McMurray JJV, Taal M, Wheeler DC, Landray MJ, Baigent C (2018) Effects of sacubitril/valsartan versus irbesartan in patients with chronic kidney disease. Circulation 138(15):1505–1514. https://doi.org/10.1161/circulationaha.118.034818
Cho IJ, Kang SM (2021) Angiotensin receptor–neprilysin inhibitor in patients with heart failure and chronic kidney disease. Kidney Res Clin Pract 40(4):555–565. https://doi.org/10.23876/j.krcp.21.900
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, Shi V, Bransford T, Takeuchi M, Gong J, Lefkowitz M, Packer M, McMurray JJ (2012) The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet (London) 380(9851):1387–1395. https://doi.org/10.1016/s0140-6736(12)61227-6
Velazquez EJ, Morrow DA, DeVore AD, Duffy CI, Ambrosy AP, McCague K, Rocha R, Braunwald E (2019) Angiotensin–neprilysin inhibition in acute decompensated heart failure. N Engl J Med 380(6):539–548. https://doi.org/10.1056/NEJMoa1812851
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Claggett B, Jhund PS, Boytsov SA, Comin-Colet J, Cleland J, Düngen HD, Goncalvesova E, Katova T, Kerr Saraiva JF, Lelonek M, Merkely B, Senni M, Shah SJ, Zhou J, Rizkala AR, Gong J, Shi VC, Lefkowitz MP (2019) Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620. https://doi.org/10.1056/NEJMoa1908655
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR (2014) Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371(11):993–1004. https://doi.org/10.1056/NEJMoa1409077
Tsutsui H, Momomura SI, Saito Y, Ito H, Yamamoto K, Sakata Y, Desai AS, Ohishi T, Iimori T, Kitamura T, Guo W (2021) Efficacy and safety of sacubitril/valsartan in japanese patients with chronic heart failure and reduced ejection fraction—results from the PARALLEL-HF study. Circ J 85(5):584–594. https://doi.org/10.1253/circj.CJ-20-0854
Berg DD, Samsky MD, Velazquez EJ, Duffy CI, Gurmu Y, Braunwald E, Morrow DA, DeVore AD (2021) Efficacy and safety of sacubitril/valsartan in high-risk patients in the PIONEER-HF trial. Circ Heart Fail 14(2):e007034. https://doi.org/10.1161/circheartfailure.120.007034
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 136(6):e137–e161. https://doi.org/10.1161/cir.0000000000000509
Chen X, Jin C, Xie L, Xiang M (2020) LCZ696 and preservation of renal function in heart failure: a meta-analysis of 6 randomized trials. Rev Cardiovasc Med 21(1):113–118. https://doi.org/10.31083/j.rcm.2020.01.2
Imamah NF, Lin HR (2021) Palliative care in patients with end-stage renal disease: a meta synthesis. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph182010651
Li Q, Li L, Wang F, Zhang W, Guo Y, Wang F, Liu Y, Jia J, Lin S (2019) Effect and safety of LCZ696 in the treatment of hypertension: a meta-analysis of 9 RCT studies. Medicine 98(28):e16093. https://doi.org/10.1097/md.0000000000016093
Zhao Y, Yu H, Zhao X, Ma R, Li N, Yu J (2017) The effects of LCZ696 in patients with hypertension compared with angiotensin receptor blockers: a meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol Ther 22(5):447–457. https://doi.org/10.1177/1074248417693379
Kario K, Sun N, Chiang FT, Supasyndh O, Baek SH, Inubushi-Molessa A, Zhang Y, Gotou H, Lefkowitz M, Zhang J (2014) Efficacy and safety of LCZ696, a first-in-class angiotensin receptor neprilysin inhibitor, in Asian patients with hypertension: a randomized, double-blind, placebo-controlled study. Hypertension (Dallas, Tex, 1979) 63(4):698–705. https://doi.org/10.1161/hypertensionaha.113.02002
Niu CY, Yang SF, Ou SM, Wu CH, Huang PH, Hung CL, Lin CC, Li SY (2022) Sacubitril/valsartan in patients with heart failure and concomitant end-stage kidney disease. J Am Heart Assoc 11(18):e026407. https://doi.org/10.1161/jaha.122.026407
Gan L, Lyu X, Yang X, Zhao Z, Tang Y, Chen Y, Yao Y, Hong F, Xu Z, Chen J, Gu L, Mao H, Liu Y, Sun J, Zhou Z, Du X, Jiang H, Li Y, Sun N, Liang X, Zuo L (2022) Application of angiotensin receptor–neprilysin inhibitor in chronic kidney disease patients: Chinese expert consensus. Front Med 9:877237. https://doi.org/10.3389/fmed.2022.877237
Ito S, Satoh M, Tamaki Y, Gotou H, Charney A, Okino N, Akahori M, Zhang J (2015) Safety and efficacy of LCZ696, a first-in-class angiotensin receptor neprilysin inhibitor, in Japanese patients with hypertension and renal dysfunction. Hypertens Res off J Jpn Soc Hypertens 38(4):269–275. https://doi.org/10.1038/hr.2015.1
Feng Y, Yin Y, Deng R, Li H (2020) Renal safety and efficacy of angiotensin receptor–neprilysin inhibitor: a meta-analysis of randomized controlled trials. J Clin Pharm Ther 45(6):1235–1243. https://doi.org/10.1111/jcpt.13243
Vollmer Barbosa C, Lang H, Melk A, Schmidt BMW (2022) Renal events in patients receiving neprilysin inhibitors: a systematic review and meta-analysis. Nephrol Dial Transpl Off Publ Eur Dial Transpl Assoc Eur Renal Assoc 37(12):2418–2428. https://doi.org/10.1093/ndt/gfac001
Funding
This work was supported by the Hebei Provincial Specialty Capacity Building and Specialty Leader Training Project [(2018)674], the Hebei Provincial Excellent Talents in Clinical Medicine Training Project [(2019)139], the Hebei province medical technology tracking project (GZ2020013), the Hebei Clinical Medical Research Centre Project (20577701D), and the project of the Hebei Provincial Excellent Health Talents and High-Quality Development of Public Hospitals [(2022)180].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors state that there is no conflict of interest.
Ethics approval
No ethical approval was required because the data were extracted from previously published articles.
Informed consent
This study did not directly involve human participants or animal subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, W., Yang, X., Jin, J. et al. The efficacy and safety of sacubitril/valsartan in chronic kidney disease: a systematic review and meta-analysis. Int Urol Nephrol 56, 181–190 (2024). https://doi.org/10.1007/s11255-023-03599-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03599-w