Abstract
Purpose
The impacts of body mass index (BMI) on the prognosis of primary IgA nephropathy (IgAN) remain controversial. This systematic review and meta-analysis aimed to solve these issues.
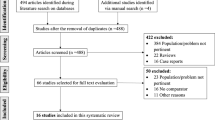
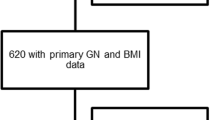
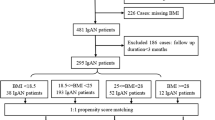
Methods
We searched the PubMed, EMBASE, and Cochrane Library to screen articles investigating the BMI and primary IgAN. BMI was classified according to the World Health Organization as high (≥ 25.0 kg/m2) and low (< 25.0 kg/m2). The baseline renal indexes and the incidences of adverse renal outcomes were focused on.
Results
Six studies with a total of 1723 patients were included in this study. High BMI was demonstrated to be associated with increased baseline levels of serum creatinine (weighted mean difference (WMD) 9.54, 95% confidence interval (CI) 0.63–18.45), blood uric acid (WMD 19.85, 95% CI 10.11–29.59) and urine protein (WMD 0.37, 95% CI 0.21–0.53). Patients with high BMI also showed compromised eGFR at diagnosis (WMD − 8.39, 95% CI − 11.62 to − 5.16) with a higher incidence rate of hypertension (odds ratios (OR) 2.59, 95% CI 1.44–4.66) and higher global optical scores (WMD 1.22, 95% CI 0.70–1.74). Regarding the prognosis, high BMI was significantly associated with the incidence of adverse renal outcomes (OR 2.43, 95% CI 1.66–3.55, P < 0.001) and deteriorated eGFR at the last follow-up (WMD − 11.10, 95% CI − 16.96 to − 5.25, P < 0.001), with non-significantly poorer renal disease-free survival (hazard ratio 1.79, 95% CI 0.58–5.50, P = 0.31).
Conclusion
High BMI was associated with severe onset and poor prognosis of primary IgAN. The management of BMI could be a novel method to promote the therapeutic outcomes of primary IgAN.




Similar content being viewed by others
References
Shao X, Li B, Cao L, Liang L, Yang J, Wang Y et al (2017) Evaluation of crescent formation as a predictive marker in immunoglobulin a nephropathy: a systematic review and meta-analysis. Oncotarget 8(28):46436–46448. https://doi.org/10.18632/oncotarget.17502
Rodrigues JC, Haas M, Reich HN (2017) IgA nephropathy. Clin J Am Soc Nephrol 12(4):677–686. https://doi.org/10.2215/CJN.07420716
Di Vico MC, Messina M, Fop F, Barreca A, Segoloni GP, Biancone L (2018) Recurrent IgA nephropathy after renal transplantation and steroid withdrawal. Clin Transplant 32(4):e13207. https://doi.org/10.1111/ctr.13207
Barbour S, Reich H (2018) An update on predicting renal progression in IgA nephropathy. Curr Opin Nephrol Hypertens 27(3):214–220. https://doi.org/10.1097/MNH.0000000000000405
Wang P, Li Y, Sun H, Liu S, Zhang R, Liu X et al (2019) Predictive value of body mass index for Short-Term outcomes of patients with esophageal cancer after esophagectomy: a meta-analysis. Ann Surg Oncol 26(7):2090–2103. https://doi.org/10.1245/s10434-019-07331-w
Kachur S, Lavie CJ, de Schutter A, Milani RV, Ventura HO (2019) Obesity and cardiovascular diseases. Minerva Med 108(3):212–228. https://doi.org/10.23736/S0026-4806.17.05022-4
Leitner DR, Fruhbeck G, Yumuk V, Schindler K, Micic D, Woodward E et al (2017) Obesity and type 2 diabetes: two diseases with a need for combined treatment strategies—EASO can lead the way. Obes Facts 10(5):483–492. https://doi.org/10.1159/000480525
Ladhani M, Craig JC, Irving M, Clayton PA, Wong G (2017) Obesity and the risk of cardiovascular and all-cause mortality in chronic kidney disease: a systematic review and meta-analysis. Nephrol Dial Transplant 32(3):439–449. https://doi.org/10.1093/ndt/gfw075
Silva JG, Bentes AC, Daher EF, Matos SM (2017) Obesity and kidney disease. J Bras Nefrol 39(1):65–69. https://doi.org/10.5935/0101-2800.20170011
Nagaraju SP, Rangaswamy D, Mareddy AS, Prasad S, Kaza S, Shenoy S et al (2018) Impact of body mass index on progression of primary immunoglobulin a nephropathy. Saudi J Kidney Dis Transpl 29(2):318–325. https://doi.org/10.4103/1319-2442.229261
Wu C, Wang AY, Li G, Wang L (2018) Association of high body mass index with development of interstitial fibrosis in patients with IgA nephropathy. Bmc Nephrol 19(1):381. https://doi.org/10.1186/s12882-018-1164-2
Ouyang Y, Xie J, Yang M, Zhang X, Ren H, Wang W et al (2016) Underweight is an independent risk factor for renal function deterioration in patients with IgA nephropathy. PLoS ONE 11(9):e162044. https://doi.org/10.1371/journal.pone.0162044
Berthoux F, Mariat C, Maillard N (2013) Overweight/obesity revisited as a predictive risk factor in primary IgA nephropathy. Nephrol Dial Transplant 28(Suppl 4):iv160–iv166. https://doi.org/10.1093/ndt/gft286
Kataoka H, Ohara M, Shibui K, Sato M, Suzuki T, Amemiya N et al (2012) Overweight and obesity accelerate the progression of IgA nephropathy: prognostic utility of a combination of BMI and histopathological parameters. Clin Exp Nephrol 16(5):706–712. https://doi.org/10.1007/s10157-012-0613-7
Bonnet F, Deprele C, Sassolas A, Moulin P, Alamartine E, Berthezene F et al (2001) Excessive body weight as a new independent risk factor for clinical and pathological progression in primary IgA nephritis. Am J Kidney Dis 37(4):720–727. https://doi.org/10.1016/s0272-6386(01)80120-7
Luo D, Wan X, Liu J et al (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27:1785–1805. https://doi.org/10.1177/0962280216669183
Wan X, Wang W, Liu J et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
WHO expert consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403):157–163. https://doi.org/10.1016/s0140-6736(03)15268-3
Wang Y, Beydoun MA, Min J, Xue H, Kaminsky LA, Cheskin LJ (2020) Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int J Epidemiol 49(3):810–823. https://doi.org/10.1093/ije/dyz273
Puigdomenech PE, Robles N, Saigi-Rubio F, Zamora A, Moharra M, Paluzie G et al (2019) Assessment of the efficacy, safety, and effectiveness of weight control and obesity management mobile health interventions: systematic review. Jmir Mhealth Uhealth 7(10):e12612. https://doi.org/10.2196/12612
Andonian C, Langer F, Beckmann J, Bischoff G, Ewert P, Freilinger S et al (2019) Overweight and obesity: an emerging problem in patients with congenital heart disease. Cardiovasc Diagn Ther 9(Suppl 2):S360–S368. https://doi.org/10.21037/cdt.2019.02.02
Andersen CJ, Murphy KE, Fernandez ML (2016) Impact of obesity and metabolic syndrome on immunity. Adv Nutr 7(1):66–75. https://doi.org/10.3945/an.115.010207
Emerenziani S, Guarino M, Trillo AL, Altomare A, Ribolsi M, Balestrieri P et al (2019) Role of overweight and obesity in gastrointestinal disease. Nutrients. https://doi.org/10.3390/nu12010111
Kovesdy CP, Furth S, Zoccali C (2017) Obesity and kidney disease: hidden consequences of the epidemic. Physiol Int 104(1):1–14. https://doi.org/10.1556/2060.104.2017.1.9
Foster MC, Hwang SJ, Larson MG, Lichtman JH, Parikh NI, Vasan RS et al (2018) Overweight, obesity, and the development of stage 3 CKD: The Framingham Heart Study. Am J Kidney Dis 52(1):39–48. https://doi.org/10.1053/j.ajkd.2008.03.003
Chang A, Van Horn L, Jacobs DJ, Liu K, Muntner P, Newsome B et al (2013) Lifestyle-related factors, obesity, and incident microalbuminuria: The CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Kidney Dis 62(2):267–275. https://doi.org/10.1053/j.ajkd.2013.02.363
Lu JL, Molnar MZ, Naseer A, Mikkelsen MK, Kalantar-Zadeh K, Kovesdy CP (2015) Association of age and BMI with kidney function and mortality: a cohort study. Lancet Diabetes Endocrinol 3(9):704–714. https://doi.org/10.1016/S2213-8587(15)00128-X
Ma X, Zhang C, Su H, Gong X, Kong X (2018) Increasing body mass index predicts rapid decline in renal function: a 5 year retrospective study. Horm Metab Res 50(7):556–561. https://doi.org/10.1055/a-0599-6360
Chang AR, Surapaneni A, Kirchner HL, Young A, Kramer HJ, Carey DJ et al (2018) Metabolically healthy obesity and risk of kidney function decline. Obesity (Silver Spring) 26(4):762–768. https://doi.org/10.1002/oby.22134
Gigante A, Giannakakis K, Di Mario F, Barbano B, Rosato E, Pofi R et al (2018) BMI, nephroangiosclerosis and glomerulonephritis: is there any meeting point? Nephrology (Carlton) 23(11):991–996. https://doi.org/10.1111/nep.13155
D’Agati VD, Chagnac A, de Vries AP, Levi M, Porrini E, Herman-Edelstein M et al (2016) Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol 12(8):453–471. https://doi.org/10.1038/nrneph.2016.75
Kalaitzidis RG, Siamopoulos KC (2011) The role of obesity in kidney disease: recent findings and potential mechanisms. Int Urol Nephrol 43(3):771–784. https://doi.org/10.1007/s11255-011-9974-1
Hong YA, Min JW, Ha MA et al (2020) The impact of obesity on the severity of clinicopathologic parameters in patients with IgA nephropathy. J Clin Med 9(9):2824. https://doi.org/10.3390/jcm9092824
Tanaka M, Yamada S, Iwasaki Y et al (2009) Impact of obesity on IgA nephropathy: comparative ultrastructural study between obese and non-obese patients. Nephron Clin Pract 112(2):c71–c78. https://doi.org/10.1159/000213084
Kittiskulnam P, Kanjanabuch T, Tangmanjitjaroen K, Chancharoenthana W, Praditpornsilpa K, Eiam-Ong S (2014) The beneficial effects of weight reduction in overweight patients with chronic proteinuric immunoglobulin a nephropathy: a randomized controlled trial. J Ren Nutr 24(3):200–207. https://doi.org/10.1053/j.jrn.2014.01.016
Shahar A, Shahar D, Kahar Y, Nitzan-Kalusky D (2005) Low-weight and weight loss as predictors of morbidity and mortality in old age. Harefuah 144(6): 443–448, 452
Thorogood M, Appleby PN, Key TJ, Mann J (2003) Relation between body mass index and mortality in an unusually slim cohort. J Epidemiol Commun Health 57(2):130–133. https://doi.org/10.1136/jech.57.2.130
Gupta R, Knobel D, Gunabushanam V, Agaba E, Ritter G, Marini C et al (2011) The effect of low body mass index on outcome in critically ill surgical patients. Nutr Clin Pract 26(5):593–597. https://doi.org/10.1177/0884533611419666
Castaneda C, Charnley JM, Evans WJ, Crim MC (1995) Elderly women accommodate to a low-protein diet with losses of body cell mass, muscle function, and immune response. Am J Clin Nutr 62(1):30–39. https://doi.org/10.1093/ajcn/62.1.30
Wang PY, Li Y, Wang Q (2020) Sarcopenia: an underlying treatment target during the COVID-19 pandemic. Nutrition 84:111104. https://doi.org/10.1016/j.nut.2020.111104
Muscaritoli M, Anker SD, Argiles J, Aversa Z, Bauer JM, Biolo G (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics.” Clin Nutr 29(2):154–159. https://doi.org/10.1016/j.clnu.2009.12.004
Rondanelli M, Klersy C, Terracol G et al (2016) Whey protein, amino acids, and vitamin D supplementation with physical activity increases fat-free mass and strength, functionality, and quality of life and decreases inflammation in sarcopenic elderly. Am J Clin Nutr 103(3):830–840. https://doi.org/10.3945/ajcn.115.113357
Bauer JM, Verlaan S, Bautmans I et al (2015) Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc 16(9):740–747. https://doi.org/10.1016/j.jamda.2015.05.021
Acknowledgements
The work was funded by the Medical Science and Technology Research Project of Henan Province (SB201901042) and the Medical Science and Technology Research Project of Henan Province (SBGJ202003050).
Author information
Authors and Affiliations
Contributions
QW, WD, PS, and JZ: research idea and study design; QW, WD, HZ, and JW: data acquisition; QW, WD, HZ, and PS: data analysis/interpretation; QW, WD, JW, and JZ: statistical analysis; HZ, PS, JW, and JZ: supervision or mentorship. Each author contributed important intellectual content during manuscript drafting or revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Data availability
All data generated or analyzed during this study are included in this published article.
Code availability
All codes used were provided in the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Q., Zhang, Jj., Dou, Wj. et al. Impact of body mass index on primary immunoglobulin A nephropathy prognosis: a systematic review and meta-analysis. Int Urol Nephrol 54, 1067–1078 (2022). https://doi.org/10.1007/s11255-021-02978-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02978-5