Abstract
Background
Malnutrition is highly prevalent and a consequence of inflammation and related comorbidities among patients on maintenance hemodialysis. Oral nutritional supplementation (ONS) is recommended for malnourished patients with kidney failure. The study aimed to evaluate renal-specific oral nutrition (ONCE dialyze) supplement on nutritional status in patients on hemodialysis.
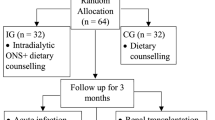
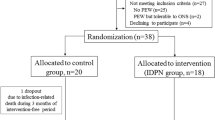
Methods
Patients were randomized into 3 groups; treatment groups received 370 kcal/day of ONCE Dialyze (N = 26) or 370 kcal/day of NEPRO (N = 30) for 30 days. The control group (N = 24) received no intervention. All patients were counseled by the same registered dietitian during the study. The nutritional status was evaluated using malnutrition inflammation score (MIS) assessment, body compositions, serum albumin and pre-albumin levels at baseline and 30 days.
Results
Eighty patients were analyzed with mean age of 57.2 ± 15.9 years. The intervention group exhibited significant improvements in energy, protein, fat, fiber and magnesium intake by dietary interview compared with the control group. Percentage of changes in MIS was − 29.0% (95% CI − 40.5 to − 17.4), − 23.9% (95% CI − 37.2 to − 10.6) and 12.1% (95% CI − 19.2 to 43.4) for the ONCE dialyze, NEPRO and control groups, respectively (overall P = 0.006). Percentage of changes in serum albumin was 5.3% (95% CI 1.9–8.7), 3.3% (95% CI − 0.1 to 6.7) and − 0.8% (95% CI − 4.3 to 2.7) for the ONCE dialyze, NEPRO, and control groups, respectively (overall P = 0.039; P = 0.043 for ONCE dialyze vs. control). No serious adverse effects were reported in any group.
Conclusion
Dietary advice combined with ONS especially ONCE dialyze was associated with improved MIS, serum albumin, dietary energy and macronutrient intake among patients with kidney failure on maintenance hemodialysis.
Clinical trial registration
TCTR20200801001.



Similar content being viewed by others
Data availability
Data supporting this study are available upon request.
References
Ikizler TA, Cano NJ, Franch H, Fouque D, Himmelfarb J, Kalantar-Zadeh K, Kuhlmann MK, Stenvinkel P, TerWee P, Teta D, Wang AY, Wanner C, International Society of Renal N, Metabolism (2013) Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int 84(6):1096–1107. https://doi.org/10.1038/ki.2013.147
Kalantar-Zadeh K, Ikizler TA, Block G, Avram MM, Kopple JD (2003) Malnutrition-inflammation complex syndrome in dialysis patients: causes and consequences. Am J Kidney Dis 42(5):864–881
Ballmer PE, McNurlan MA, Hulter HN, Anderson SE, Garlick PJ, Krapf R (1995) Chronic metabolic acidosis decreases albumin synthesis and induces negative nitrogen balance in humans. J Clin Invest 95(1):39–45. https://doi.org/10.1172/JCI117668
Burrowes JD, Larive B, Cockram DB, Dwyer J, Kusek JW, McLeroy S, Poole D, Rocco MV, Hemodialysis Study G (2003) Effects of dietary intake, appetite, and eating habits on dialysis and non-dialysis treatment days in hemodialysis patients: cross-sectional results from the HEMO study. J Ren Nutr 13(3):191–198. https://doi.org/10.1016/s1051-2276(03)00069-4
Supasyndh O, Satirapoj B, Seenamngoen S, Yongsiri S, Choovichian P, Vanichakarn S (2009) Nutritional status of twice and thrice-weekly hemodialysis patients with weekly Kt/V > 3.6. J Med Assoc Thai 92(5):624–631
Sezer S, Bal Z, Tutal E, Uyar ME, Acar NO (2014) Long-term oral nutrition supplementation improves outcomes in malnourished patients with chronic kidney disease on hemodialysis. JPEN J Parenter Enteral Nutr 38(8):960–965. https://doi.org/10.1177/0148607113517266
Malgorzewicz S, Galezowska G, Cieszynska-Semenowicz M, Ratajczyk J, Wolska L, Rutkowski P, Jankowska M, Rutkowski B, Debska-Slizien A (2019) Amino acid profile after oral nutritional supplementation in hemodialysis patients with protein-energy wasting. Nutrition 57:231–236. https://doi.org/10.1016/j.nut.2018.06.013
Leonberg-Yoo AK, Wang W, Weiner DE, Lacson E Jr (2019) Oral nutritional supplements and 30-day readmission rate in hypoalbuminemic maintenance hemodialysis patients. Hemodial Int 23(1):93–100. https://doi.org/10.1111/hdi.12694
Weiner DE, Tighiouart H, Ladik V, Meyer KB, Zager PG, Johnson DS (2014) Oral intradialytic nutritional supplement use and mortality in hemodialysis patients. Am J Kidney Dis 63(2):276–285. https://doi.org/10.1053/j.ajkd.2013.08.007
Benner D, Brunelli SM, Brosch B, Wheeler J, Nissenson AR (2018) Effects of oral nutritional supplements on mortality, missed dialysis treatments, and nutritional markers in hemodialysis patients. J Ren Nutr 28(3):191–196. https://doi.org/10.1053/j.jrn.2017.10.002
Lacson E Jr, Ikizler TA, Lazarus JM, Teng M, Hakim RM (2007) Potential impact of nutritional intervention on end-stage renal disease hospitalization, death, and treatment costs. J Ren Nutr 17(6):363–371. https://doi.org/10.1053/j.jrn.2007.08.009
Liu PJ, Ma F, Wang QY, He SL (2018) The effects of oral nutritional supplements in patients with maintenance dialysis therapy: a systematic review and meta-analysis of randomized clinical trials. PLoS ONE 13(9):e0203706. https://doi.org/10.1371/journal.pone.0203706
Sabatino A, Piotti G, Cosola C, Gandolfini I, Kooman JP, Fiaccadori E (2018) Dietary protein and nutritional supplements in conventional hemodialysis. Semin Dial 31(6):583–591. https://doi.org/10.1111/sdi.12730
Satirapoj B, Limwannata P, Kleebchaiyaphum C, Prapakorn J, Yatinan U, Chotsriluecha S, Supasyndh O (2017) Nutritional status among peritoneal dialysis patients after oral supplement with ONCE dialyze formula. Int J NephrolRenovasc Dis 10:145–151. https://doi.org/10.2147/IJNRD.S138047
Cano N, Fiaccadori E, Tesinsky P, Toigo G, Druml W, Dgem KM, Mann H, Horl WH, Espen (2006) ESPEN guidelines on enteral nutrition: adult renal failure. ClinNutr 25(2):295–310. https://doi.org/10.1016/j.clnu.2006.01.023
Kistler BM, Benner D, Burrowes JD, Campbell KL, Fouque D, Garibotto G, Kopple JD, Kovesdy CP, Rhee CM, Steiber A, Stenvinkel P, Ter Wee P, Teta D, Wang AYM, Kalantar-Zadeh K (2018) Eating during hemodialysis treatment: a consensus statement from the international society of renal nutrition and metabolism. J Ren Nutr 28(1):4–12. https://doi.org/10.1053/j.jrn.2017.10.003
Kalantar-Zadeh K, Kopple JD, Block G, Humphreys MH (2001) A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am J Kidney Dis 38(6):1251–1263. https://doi.org/10.1053/ajkd.2001.29222
Leal VO, Stockler-Pinto MB, Farage NE, Aranha LN, Fouque D, Anjos LA, Mafra D (2011) Handgrip strength and its dialysis determinants in hemodialysis patients. Nutrition 27(11–12):1125–1129. https://doi.org/10.1016/j.nut.2010.12.012
Wight JP, Edwards L, Brazier J, Walters S, Payne JN, Brown CB (1998) The SF36 as an outcome measure of services for end stage renal failure. Qual Health Care 7(4):209–221. https://doi.org/10.1136/qshc.7.4.209
Wang AY, Sanderson J, Sea MM, Wang M, Lam CW, Li PK, Lui SF, Woo J (2003) Important factors other than dialysis adequacy associated with inadequate dietary protein and energy intakes in patients receiving maintenance peritoneal dialysis. Am J ClinNutr 77(4):834–841. https://doi.org/10.1093/ajcn/77.4.834
Mpio I, Cleaud C, Arkouche W, Laville M (2015) Results of therapeutics strategy of protein-energy wasting in chronic hemodialysis: a prospective study during 12 months. NephrolTher 11(2):97–103. https://doi.org/10.1016/j.nephro.2014.11.002
Tomayko EJ, Kistler BM, Fitschen PJ, Wilund KR (2015) Intradialytic protein supplementation reduces inflammation and improves physical function in maintenance hemodialysis patients. J Ren Nutr 25(3):276–283. https://doi.org/10.1053/j.jrn.2014.10.005
Fouque D, McKenzie J, de Mutsert R, Azar R, Teta D, Plauth M, Cano N, RenilonMulticentre Trial Study G (2008) Use of a renal-specific oral supplement by haemodialysis patients with low protein intake does not increase the need for phosphate binders and may prevent a decline in nutritional status and quality of life. Nephrol Dial Transplant 23(9):2902–2910. https://doi.org/10.1093/ndt/gfn131
Sharma M, Rao M, Jacob S, Jacob CK (2002) A controlled trial of intermittent enteral nutrient supplementation in maintenance hemodialysis patients. J Ren Nutr 12(4):229–237. https://doi.org/10.1053/jren.2002.35300
Caglar K, Fedje L, Dimmitt R, Hakim RM, Shyr Y, Ikizler TA (2002) Therapeutic effects of oral nutritional supplementation during hemodialysis. Kidney Int 62(3):1054–1059. https://doi.org/10.1046/j.1523-1755.2002.00530.x
Stratton RJ, Bircher G, Fouque D, Stenvinkel P, de Mutsert R, Engfer M, Elia M (2005) Multinutrient oral supplements and tube feeding in maintenance dialysis: a systematic review and meta-analysis. Am J Kidney Dis 46(3):387–405. https://doi.org/10.1053/j.ajkd.2005.04.036
Coombes JS, Fassett RG (2012) Antioxidant therapy in hemodialysis patients: a systematic review. Kidney Int 81(3):233–246. https://doi.org/10.1038/ki.2011.341
Cheu C, Pearson J, Dahlerus C, Lantz B, Chowdhury T, Sauer PF, Farrell RE, Port FK, Ramirez SP (2013) Association between oral nutritional supplementation and clinical outcomes among patients with ESRD. Clin J Am SocNephrol 8(1):100–107. https://doi.org/10.2215/CJN.13091211
Pupim LB, Majchrzak KM, Flakoll PJ, Ikizler TA (2006) Intradialytic oral nutrition improves protein homeostasis in chronic hemodialysis patients with deranged nutritional status. J Am SocNephrol 17(11):3149–3157. https://doi.org/10.1681/ASN.2006040413
Kalantar-Zadeh K, Kilpatrick RD, Kuwae N, McAllister CJ, Alcorn H Jr, Kopple JD, Greenland S (2005) Revisiting mortality predictability of serum albumin in the dialysis population: time dependency, longitudinal changes and population-attributable fraction. Nephrol Dial Transplant 20(9):1880–1888. https://doi.org/10.1093/ndt/gfh941
Chen WC, Huang WC, Chiu CC, Chang YK, Huang CC (2014) Whey protein improves exercise performance and biochemical profiles in trained mice. Med Sci Sports Exerc 46(8):1517–1524. https://doi.org/10.1249/MSS.0000000000000272
Huang WC, Chang YC, Chen YM, Hsu YJ, Huang CC, Kan NW, Chen SS (2017) Whey protein improves marathon-induced injury and exercise performance in elite track runners. Int J Med Sci 14(7):648–654. https://doi.org/10.7150/ijms.19584
Hassan AM, Abdel-Aziem SH, Abdel-Wahhab MA (2012) Modulation of DNA damage and alteration of gene expression during aflatoxicosis via dietary supplementation of Spirulina (Arthrospira) and Whey protein concentrate. Ecotoxicol Environ Saf 79:294–300. https://doi.org/10.1016/j.ecoenv.2012.01.017
Tang JE, Moore DR, Kujbida GW, Tarnopolsky MA (1985) Phillips SM (2009) Ingestion of whey hydrolysate, casein, or soy protein isolate: effects on mixed muscle protein synthesis at rest and following resistance exercise in young men. J ApplPhysiol 107(3):987–992. https://doi.org/10.1152/japplphysiol.00076.2009
Acknowledgements
The authors wish to acknowledge the contributions of the following individuals to this study: staff in the Division of Nephrology in Phramongkutklao Hospital.
Funding
The study was supported by a Grant from Phramongkutklao Hospital and College of Medicine, Bangkok, Thailand and the Thai Otsuka Pharmaceutical Co., Ltd. Thailand, which had no influence on the design, conduct, analysis or reporting of our trial.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
The study was approved by the Ethics Committee of the Institute Review Board at the Royal Thai Army Medical Department and was conducted according to the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Limwannata, P., Satirapoj, B., Chotsriluecha, S. et al. Effectiveness of renal-specific oral nutritional supplements compared with diet counseling in malnourished hemodialysis patients. Int Urol Nephrol 53, 1675–1687 (2021). https://doi.org/10.1007/s11255-020-02768-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02768-5