Abstract
Background
Chronic fluid overload is common in maintenance hemodialysis (HD) patients and is associated with severe cardiovascular complications, such as arterial hypertension, left ventricular hypertrophy, congestive heart failure, and arrhythmia. Therefore, a crucial target of HD is to achieve the so-called dry weight; however, the best way to assess fluid status and dry weight is still unclear. Dry weight is currently determined in most dialysis units on a clinical basis, and it is commonly defined as the lowest body weight a patient can tolerate without developing intra-dialytic or inter-dialytic hypotension or other symptoms of dehydration. One of the most promising methods that have emerged in recent years is bioelectrical impedance analysis (BIA), which estimates body composition, including hydration status, by measuring the body’s resistance and reactance to electrical current. Our objective was to study the effect BIA-guided versus clinical-guided ultrafiltration on various cardiovascular disease risk factors and markers in HD patients.
Materials and methods
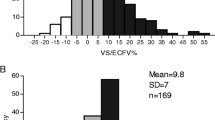
We included 135 HD patients from a single center in a prospective study, aiming to compare the long-term (12 months) effect of BIA-based versus clinical-based assessment of dry weight on blood pressure (BP), pulse wave velocity (PWV), and serum N-terminal fragment of B-type natriuretic peptide (NT-proBNP). The body composition was measured using the portable whole-body multifrequency BIA device, Body Composition Monitor—BCM® (Fresenius Medical Care, Bad Homburg, Germany).
Results
In the “clinical” group there were no changes in BP, body mass index (BMI), and body fluids. The PWV increased from 7.9 ± 2.5 to 9.2 ± 3.6 m/s (P = 0.002), whereas serum NT-proBNP decreased from 5,238 to 3,883 pg/ml (P = 0.05). In the “BIA” group, BMI and body volumes also did not change; however, there was a significant decrease in both systolic BP, from 144.6 ± 14.7 to 135.3 ± 17.8 mmHg (P < 0.001), and diastolic BP, from 79.5 ± 9.7 to 73.2 ± 11.1 mmHg (P < 0.001). In this group, PWV also decreased from 8.2 ± 2.3 to 6.9 ± 2.3 m/s (P = 0.001) and NT-proBNP decreased from 7,552 to 4,561 pg/ml (P = 0.001).
Conclusion
BIA is not inferior and possibly even better than clinical criteria for assessing dry weight and guiding ultrafiltration in HD patients.
Similar content being viewed by others
References
Lin YP, Chen CH, Yu WC, Hsu TL, Ding PY, Yang WC (2002) Left ventricular mass and hemodynamic overload in normotensive hemodialysis patients. Kidney Int 62:1828–1838
Wang MC, Tseng CC, Tsai WC, Huang JJ (2001) Blood pressure and left ventricular hypertrophy in patients on different peritoneal dialysis regimens. Perit Dial Int 21: 36–42
Konings CJ, Kooman JP, Schonck M, Dammers R, Cheriex E, Palmans Meulemans AP et al. (2002) Fluid status, blood pressure, and cardiovascular abnormalities in patients on peritoneal dialysis. Perit Dial Int 22:477–487
Lameire N, Van BW (2001) Importance of blood pressure and volume control in peritoneal dialysis patients. Perit Dial Int 21:206–211
Charra B, Laurent G, Chazot C, Calemard E, Terrat JC, Vanel T, Jean G, Ruffet M (1996) Clinical assessment of dry weight. Nephrol Dial Transplant 11(2):16–19
Sinha AD, Agarwal R (2009) Can chronic volume overload be recognized and prevented in hemodialysis patients? The pitfalls of the clinical examination in assessing volume status. Semin Dial 22:480–482
Raimann J, Liu L, Ulloa D et al (2008) Consequences of overhydration and the need for dry weight assessment. Contrib Nephrol 161:99–107
Zheng D, Cheng LT, Zhuang Z, Gu Y, Tang LJ, Wang T (2009) Correlation between pulse wave velocity and fluid distribution in hemodialysis patients. Blood Purif 27:248–252
Vlachopoulos C, Aznaouridis K, Stefanadis C (2010) Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 55:1318–1327
Verbeke F, Van Biesen W, Honkanen E, Wikström B, Jensen PB, Krzesinski JM, Rasmussen M, Vanholder R, Rensma PL (2010) on behalf of the CORD Study Investigators. Prognostic value of aortic stiffness and calcification for cardiovascular events and mortality in dialysis patients: Outcome of the Calcification Outcome in Renal Disease (CORD) Study. Clin J Am Soc Nephrol [Epub ahead of print]
Chongthanakorn K, Tiranathanagul K, Susantitaphong P, Praditpornsilpa K, Eiam-Ong S (2009) Effective determination of dry weight by intradialytic bioimpedance analysis in hemodialysis. Blood Purif 27:235–241
Wabel P, Chamney P, Moissl U, Jirka T (2009) Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif 27:75–80
Wystrychowski G, Levin NW (2007) Dry weight: sine qua non of adequate dialysis. Adv Chronic Kidney Dis 14: e10–e16
Charra B (1998) ‘Dry weight’ in dialysis: the history of a concept. Nephrol Dial Transplant 7:1882–1885
Wizemann V, Schilling M (1995) Dilemma of assessing volume state—the use and the limitations of a clinical score. Nephrol Dial Transplant 10:2114–2117
Charra B (2007) Fluid balance, dry weight, and blood pressure in dialysis. Hemodial Int 11:21–31
Kouw PM, Kooman JP, Cheriex EC et al. (1993) Assessment of postdialysis dry weight: a comparison of techniques. J Am Soc Nephrol 4:98–104
Leunissen KML, Kouw PM, Kooman JP et al. (1993) New techniques to determine fluid status in hemodialysed patients. Kidney Int 43:50–56
Dasselaar JJ, Huisman RM, de Jong PE et al. (2005) Measurement of relative blood volume changes during haemodialysis: merits and limitations. Nephrol Dial Transplant 20:2043–2049
Agarwal R, Kelley K, Light RP (2008) Diagnostic utility of blood volume monitoring in hemodialysis patients. Am J Kidney Dis 51(2):242–254
Katzarski KS, Nisell J, Randmaa I, Danielsson A, Freyschuss U, Bergstrom J (1997) A critical evaluation of ultrasound measurement of inferior vena cava diameter in assessing dry weight in normotensive and hypertensive hemodialysis patients. Am J Kidney Dis 30:459–465
Chang ST, Chen CL, Chen CC, Lin FC, Wu D (2004) Enhancement of quality of life with adjustment of dry weight by echocardiographic measurement of inferior vena cava diameter in patients undergoing chronic hemodialysis. Nephron Clin Pract 97:c90–c97
Brennan JM, Ronan A, Goonewardena S, Blair JE, Hammes M, Shah D, Vasaiwala S, Kirkpatrick JN, Spencer KT (2006) Handcarried ultrasound measurement of the inferior vena cava for assessment of intravascular volume status in the outpatient hemodialysis clinic. Clin J Am Soc Nephrol 1:749–753
Haug C, Metzele A, Steffgen J et al. (1994) Changes in brain natriuretic peptide and atrial natriuretic peptide plasma concentrations during hemodialysis in patients with chronic renal failure. Horm Metab Res 26:246–249
Zoccali C, Mallamaci F, Benedetto FA, Tripepi G, Parlongo S, Cataliotti A, Cutrupi S, Giacone G, Bellanuova I, Cottini E, Malatino LS (2001) Creed Investigators. Cardiac natriuretic peptides are related to left ventricular mass and function and predict mortality in dialysis patients. J Am Soc Nephrol 12:1508–1515
Sommerer C, Beimler J, Schwenger V, Heckele N, Katus HA, Giannitsis E, Zeier M (2007) Cardiac biomarkers and survival in haemodialysis patients. Eur J Clin Invest 37:350–356
Vickery S, Price CP, John RI et al. (2005) B-type natriuretic peptide (BNP) and amino-terminal proBNP in patients with CKD: relationship to renal function and left ventricular hypertrophy. Am J Kidney Dis 46:610–620
Paniagua R, Ventura MD, Avila-Díaz M, Hinojosa-Heredia H, Méndez-Durán A, Cueto-Manzano A, Cisneros A, Ramos A, Madonia-Juseino C, Belio-Caro F, García-Contreras F, Trinidad-Ramos P, Vázquez R, Ilabaca B, Alcántara G, Amato D (2010) NT-proBNP, fluid volume overload and dialysis modality are independent predictors of mortality in ESRD patients. Nephrol Dial Transplant 25:551–557
Codognotto M, Piccoli A, Zaninotto M, Mion MM, Ruzza L, Barchita A, Naso A, Plebani M (2010) Effect of a dialysis session on the prognostic values of NT-proBNP, troponins, endothelial damage and inflammation biomarkers. J Nephrol 23:465–471
Kyle UG, Bosaeus I, De Lorenzo AD et al. (2004) Bioelectrical impedance analysis. II. Utilization in clinical practice. Clin Nutr 23:1430–1453
Kuhlmann MK, Zhu F, Seibert E et al (2005) Bioimpedance, dry weight and blood pressure control: new methods and consequences. Curr Opin Nephrol Hypertens 14:543–549
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, Korth O, Müller MJ, Ellegård L, Malmros V, Kaitwatcharachai C, Kuhlmann MK, Zhu F, Fuller NJ (2006) Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27:921–933
Kotanko P, Levin NW, Zhu F (2008) Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant 23:808–812
Chamney PW, Kramer M, Rode C et al. (2002) A new technique for establishing dry weight in hemodialysis patients via whole body bioimpedance. Kidney Int 61:2250–2258
Wabel P, Moissl U, Chamney P et al. (2008) Towards improved cardiovascular management: the necessity of combining blood pressure and fluid overload. Nephrol Dial Transplant 23:2965–2971
Park J, Yang WS, Kim SB et al. (2009) Usefulness of segmental bioimpedance ratio to determine dry body weight in new hemodialysis patients: a pilot study. Am J Nephrol 29:25–30
Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C, Malecka-Masalska T, Marcelli D (2009) The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant 24:1574–1579
Machek P, Jirka T, Moissl U, Chamney P, Wabel P (2010) Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant 25(2):538–544
Tattersall J (2009) Bioimpedance analysis in dialysis: state of the art and what we can expect. Blood Purif 27(1):70–74
Segers P, Qasem A, DeBacker T, Carlier S, Verdonck P, Avolio A (2001) Peripheral ‘oscillatory’ compliance is associated with aortic augmentation index. Hypertension 37:1434–1439
Safar ME, London GM (2000) Therapeutic studies and arterial stiffness in hypertension: recommendations of the European Society of Hypertension. The Clinical Committee of Arterial Structure and Function. Working group on vascular structure and function of the European Society of Hypertension. J Hypertens 18:1527–1535
National Kidney Foundation (2006) K/DOQI Clinical Practice Guidelines for Hemodialysis Adequacy, update 2006. Am J Kidney Dis 48:S33–S39
Hörl WH (2010) Hypertension in end-stage renal disease: different measures and their prognostic significance. Nephrol Dial Transplant 25:3161–3166
Chang TI, Friedman GD, Cheung AK, Greene T, Desai M, Chertow GM (2011) Systolic blood pressure and mortality in prevalent haemodialysis patients in the HEMO study. J Hum Hypertens 25:98–105
Agarwal R (2010) Blood pressure and mortality among hemodialysis patients. Hypertension 55:762–768
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Onofriescu, M., Mardare, N.G., Segall, L. et al. Randomized trial of bioelectrical impedance analysis versus clinical criteria for guiding ultrafiltration in hemodialysis patients: effects on blood pressure, hydration status, and arterial stiffness. Int Urol Nephrol 44, 583–591 (2012). https://doi.org/10.1007/s11255-011-0022-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-011-0022-y