Abstract
Background
Chronic volume overload is very frequent in hemodialysis (HD) patients and is directly associated with hypertension, increased arterial stiffness, left ventricular hypertrophy (LVH), heart failure and ultimately with higher mortality and morbidity. One major issue is that presently there are very few comparative studies of the various methods (clinical, bioimpedance, inferior cava vein diameter (ICV) and Brain Natriuretic Peptide (NT-proBNP)) for volume status evaluation and their correlation with cardiovascular disease.
Methods
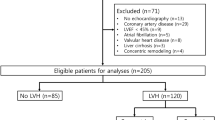
In 160 patients treated by chronic HD in our center, euvolemic according to clinical assessment, we performed evaluation of volume status through bioimpedance spectroscopy (BIS), ICV and NT-proBNP, as well as echocardiography, to estimate the left ventricle structure and function.
Results
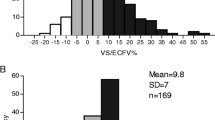
Despite appearing clinically euvolemic, severe fluid overload, as defined by a relative tissue hydration (RTH)—i.e. fluid overload over extracellular water ratio (FO/ECW)—above 15% was found in 25.6% of patients. Four categories of patients were considered according to pre-HD BP and BIS values. Forty-five percent of patients (group A) had a reasonable control of BP and volume (SBP < 150 mmHg and RTH < 15%), 29.3% (group B) were classified as hypertensive (SBP > 150 mmHg and RTH < 15%), 16.7% (group C) had high blood pressure and marked volume expansion, (SBP > 150 mmHg and RTH > 15%), while 9% (group D) had SBP < 150 mmHg despite RTH > 15%. Assuming that BIS is the most accurate and validated method to assess hydration status, we calculated the positive predictive value for ICV-based evaluation—18%, with a sensitivity of 67% and an important proportion of false negative cases (45%). NT-proBNP was even less accurate: PPV of only 26%, with a sensitivity of 60% and a specificity of only 45% and an extremely high proportion of false positive cases (73%). Group A patients had the best cardio-vascular profile: lowest LV mass and NT-proBNP levels.
Conclusion
Using multi-frequency body impedance spectroscopy, we found a large group of hypertensive and/or fluid-overloaded patients despite apparently being at “dry weight” on clinical evaluation and a marked discrepancy between clinical appearance and fluid status. Of the 4 different methods, assuming BCM “gold standard”, there were major disagreements and discrepancies between the other three methodologies. BCM is a valuable and simple bed-side tool for the correct management of BP and risk stratification in HD patients as it allows for excellent discriminators of more abnormal cardiac and vascular profiles.



Similar content being viewed by others
References
Gusbeth-Tatomir P, Covic A (2007) Causes and consequences of increased arterial stiffness in chronic kidney disease patients. Kidney Blood Press Res. 30:97–107
Tonelli M, Wiebe N, Culleton B et al (2006) Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol 17:2034–2047
Surekha M, Sridevi D, Ishwarlal J (2002) Accelerated atherosclerosis, dyslipidemia, and oxidative stress in end-stage renal disease. Curr Opin Nephrol Hypertens 11:141–147
Goodman WG, London G, Amann K et al (2004) Vascular calcification in chronic kidney disease. Am J Kidney Dis 43:572–579
Kuhlmann MK, Zhu F, Seibert E, Levin NW (2005) Bioimpedance, dry weight and blood pressure control: new methods and consequences. Curr Opin Nephrol Hypertens 14:543–549
Ozkahya M, Ok E, Toz H et al (2006) Long-term survival rates in haemodialysis patients treated with strict volume control. Nephrol Dial Transplant 21:3506–3513
Agarwal R, Andersen MJ, Pratt HJ (2008) On the importance of pedal edema in hemodialysis patients. Clin J Am Soc Nephrol 3:153–158
Leunissen KM, Kouw P, Kooman JP et al (1993) New techniques to determine fluid status in hemodialyzed patients. Kidney Int 41:S50–S56
Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351:1097–1105
Bargnoux AS, Klouche K, Fareh J et al (2008) Prohormone brain natriuretic peptide (proBNP), BNP and N-terminal-proBNP circulating levels in chronic hemodialysis patients. Correlation with ventricular function, fluid removal and effect of hemodiafiltration. Clin Chem Lab Med 46:1019–1024
Kotanko P, Levin NW, Zhu F (2008) Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant 23:808–812
Chamney PW, Wabel P, Moissl UM et al (2007) A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr 85:80–89
Moissl UM, Wabel P, Chamney PW et al (2006) Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27:921–933
Passauer J, Miller H, Schleser A et al (2007) Evaluation of clinical dry weight assessment in haemodialysis patients by bioimpedance-spectroscopy. J Am Soc Nephrol 18A:256
Wizemann V, Wabel P, Chamney C et al (2009) The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant 24:1574–1579
Wabel P, Moissl U, Chamney C et al (2008) Towards improved cardiovascular management: the necessity of combining blood pressure and fluid overload. Nephrol Dial Transplant 23:2965–2971
Devolder I, Verleysen A, Vijt D, Vanholder R, Van Biesen B (2010) Body composition, hydration and related parameters in hemodialysis versus peritoneal dialysis patients. Perit Dial Int (in press)
Essig M, Escoubet B, de Zuttere D et al (2008) Cardiovascular remodeling and extracellular fluid excess in early stages of chronic kidney disease. Nephrol Dial Transplant 23:239–248
Cole KS, Li CL, Bak AF (1969) Electrical analogues for tissues. Exp Neurol 24:459–473
Moissl UM, Wabel P, Chamney PW et al (2006) Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27:921–933
Wabel P, Chamney P, Moissl U (2007) Reproducibility of bioimpedance spectroscopy for the assessment of body composition and dry weight. J Am Soc Nephrol 18:A255
Daugirdas JT (1993) Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 4:1205–1213
Brennan JM, Ronan A, Goonewardena S et al (2006) Handcarried ultrasound measurement of the inferior vena cava for assessment of intravascular volume status in the outpatient hemodialysis clinic. Clin J Am Soc Nephrol 1:749–753
Prontera C, Emdin M, Zucchelli GC, Ripoli A, Passino C, Clerico A (2003) Natriuretic peptides (NPs): automated electrochemiluminescent immunoassay for N-terminal pro-BNP compared with IRMAs for ANP and BNP in heart failure patients and healthy individuals. Clin Chem 49:1552–1554
Charra B, Laurent G, Chazot C et al (1996) Clinical assessment of dry weight. Nephrol Dial Transplant 11(Suppl 2):16–19
Sommerer C, Beimler J, Schwenger V et al (2007) Cardiac biomarkers and survival in haemodialysis patients. Eur J Clin Invest 37:350–356
Machek P, Jirka T, Moissl U, Chamney P, Wabel P (2010) Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant 25:538–544
Goldsmith D, Covic A (2009) Blood pressure control in CKD stage 5D patients–are we more or less certain what to do in 2009? Nephrol Dial Transplant 14:3597–3601
Rahman D, Smith M (2001) Hypertension in dialysis patients. Curr Hypertens Rep 3:496–502
Leypoldt JK, Cheung AK, Delmez JA (2002) Relationship between volume status and blood pressure during chronic hemodialysis. Kidney Int 61:266–275
Bos W, Bruin S, wan Olden RW et al (2000) Cardiac and hemodynamic effects of hemodialysis and ultrafiltration. Am J Kidney Dis 35:819–826
Agarwal R (2005) Hypertension in chronic kidney disease and dialysis: pathophysiology and management. Cardiol Clinics 23:237–248
Li Z, Lacson E, Lowrie EG et al (2006) The epidemiology of systolic blood pressure and death risk in hemodialysis patients. Am J Kidney Dis 48:606–615
D’Amico G, Locatelli F (2002) Hypertension in dialysis: pathophysiology and treatment. J Nephrol 15:438–445
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Voroneanu, L., Cusai, C., Hogas, S. et al. The relationship between chronic volume overload and elevated blood pressure in hemodialysis patients: use of bioimpedance provides a different perspective from echocardiography and biomarker methodologies. Int Urol Nephrol 42, 789–797 (2010). https://doi.org/10.1007/s11255-010-9767-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-010-9767-y