Abstract
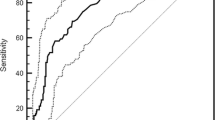
This study evaluated whether degradation products of plasma fibrin and fibrinogen (FDP) level can be used to differentiate acute aortic dissection (AAD) from acute myocardial infarction (AMI), angina pectoris, acute cerebral infarction, or transient cerebral ischemic attack (TIA). Ninety-six consecutive patients with definitive diagnosis of AAD by contrast-enhanced computed tomography scan underwent measurement of FDP on admission. Of these patients, 45 had a patent false lumen (patent-type), and 51 had complete thrombosis of the false lumen (thrombosed-type). Control groups were patients admitted during the same period for whom a diagnosis of either AMI (n = 187), angina pectoris (n = 142), cerebral infarction (n = 353), or TIA (n = 94) was confirmed. FDP was significantly higher in patients with patent-type AAD (median, 210 μg/mL; interquartile range, 70–358 μg/mL) than in those with thrombosed-type AAD (16.5, 7.2–50.1). Patients with patent-type AAD or thrombosed-type AAD had a significantly higher FDP than patients in any of the control groups. Receiver operating characteristic curve analysis indicated that FDP ≥ 12.6 μg/mL was the cutoff value that best differentiated patients with patent-type AAD from patients in any of the control groups (sensitivity, 100 %; negative predictive value [NPV], 100 %). And, this FDP cutoff level was associated with a high positive predictive value (PPV) (80–92 %). The cutoff value to differentiate patients with thrombosed-type AAD from patients in any of the control groups was FDP ≥ 5.6 μg/mL (sensitivity, 100 %; NPV, 100 %). However, this FDP cutoff level was associated with a low PPV (36–81 %). FDP and D-dimer were measured at the same time on admission in 30 patients with AAD and 41 patients in control groups. A simple liner regression, calculated using FDP and D-dimer values from a total of 71 patients, yielded a correlation coefficient (R 2) of 0.95, indicating a strong correlation. In symptomatic patients with suspected AAD, a diagnosis of patent-type AAD should be considered if FDP ≥ 12.6 μg/mL. Patients with FDP ≥ 5.6 μg/mL have the possibility of thrombosed-type AAD.



Similar content being viewed by others
References
Castelan DJ, Hirsh J, Martin M (1968) Latex-bound antifibrinogen test for plasma fibrinogen assay. J Clin Pathol 21(5):638–642
Rowbotham BJ, Carroll P, Whitaker AN, Bunce IH, Cobcroft RG, Elms MJ, Masci PP, Bundesen PG, Rylatt DB, Webber AJ (1987) Measurement of crosslinked fibrin derivatives–use in the diagnosis of venous thrombosis. Thromb Haemost 57(1):59–61
Guidelines on diagnosis and management of acute pulmonary embolism (2000) Task Force on Pulmonary Embolism, European Society of Cardiology. Eur Heart J 21(16):1301–1336
Ohlmann P, Faure A, Morel O, Petit H, Kabbaj H, Meyer N, Cheneau E, Jesel L, Epailly E, Desprez D et al (2006) Diagnostic and prognostic value of circulating D-Dimers in patients with acute aortic dissection. Crit Care Med 34(5):1358–1364
Suzuki T, Distante A, Zizza A, Trimarchi S, Villani M, Salerno Uriarte JA, De Luca Tupputi Schinosa L, Renzulli A, Sabino F, Nowak R et al (2009) Diagnosis of acute aortic dissection by D-dimer: the International Registry of Acute Aortic Dissection Substudy on Biomarkers (IRAD-Bio) experience. Circulation 119(20):2702–2707
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK et al (2000) The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 283(7):897–903
Nienaber CA, von Kodolitsch Y, Nicolas V, Siglow V, Piepho A, Brockhoff C, Koschyk DH, Spielmann RP (1993) The diagnosis of thoracic aortic dissection by noninvasive imaging procedures. N Engl J Med 328(1):1–9
Erbel R, Alfonso F, Boileau C, Dirsch O, Eber B, Haverich A, Rakowski H, Struyven J, Radegran K, Sechtem U et al (2001) Diagnosis and management of aortic dissection. Eur Heart J 22(18):1642–1681
Tsai TT, Evangelista A, Nienaber CA, Myrmel T, Meinhardt G, Cooper JV, Smith DE, Suzuki T, Fattori R, Llovet A et al (2007) Partial thrombosis of the false lumen in patients with acute type B aortic dissection. N Engl J Med 357(4):349–359
Tamori Y, Akutsu K, Kasai S, Sakamoto S, Okajima T, Yoshimuta T, Yokoyama N, Ogino H, Higashi M, Nonogi H et al (2009) Coexistent true aortic aneurysm as a cause of acute aortic dissection. Circ J 73(5):822–825
Fraker TD Jr, Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, Ferguson TB Jr, Fihn SD et al (2007) 2007 chronic angina focused update of the ACC/AHA 2002 Guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 Guidelines for the management of patients with chronic stable angina. Circulation 116(23):2762–2772
Wagner GS, Macfarlane P, Wellens H, Josephson M, Gorgels A, Mirvis DM, Pahlm O, Surawicz B, Kligfield P, Childers R et al (2009) AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part VI: acute ischemia/infarction: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation 119(10):e262–e270
Swain S, Turner C, Tyrrell P, Rudd A (2008) Diagnosis and initial management of acute stroke and transient ischaemic attack: summary of NICE guidance. BMJ 337:a786
Nagaoka K, Sadamatsu K, Yamawaki T, Shikada T, Sagara S, Ohe K, Morishige K, Tanaka E, Tashiro H (2010) Fibrinogen/fibrin degradation products in acute aortic dissection. Intern Med 49(18):1943–1947
Ohlmann P, Faure A, Morel O, Kindo M, Jesel L, Radulescu B, Billaud P, Meyer N, Petit H, Trinh A et al (2009) Lower circulating Sta-Liatest D-Di levels in patients with aortic intramural hematoma compared with classical aortic dissection. Crit Care Med 37(3):899–901
Mohr-Kahaly S, Erbel R, Kearney P, Puth M, Meyer J (1994) Aortic intramural hemorrhage visualized by transesophageal echocardiography: findings and prognostic implications. J Am Coll Cardiol 23(3):658–664
Erbel R, Oelert H, Meyer J, Puth M, Mohr-Katoly S, Hausmann D, Daniel W, Maffei S, Caruso A, Covino FE et al (1993) Effect of medical and surgical therapy on aortic dissection evaluated by transesophageal echocardiography. Implications for prognosis and therapy. The European Cooperative Study Group on Echocardiography. Circulation 87(5):1604–1615
Stellwag-Carion C, Pollak S (1978) Idiopathic aortic rupture as a cause of sudden death. Beitr Gerichtl Med 36:307–317
Shingu Y, Myojin K, Ishibashi Y, Ishii K, Kawasaki M (2005) Conservative therapy for thrombosed acute aortic dissection. J Jpn Coll Angiol 45:941–944
Paparella D, Malvindi PG, Scrascia G, de Ceglia D, Rotunno C, Tunzi F, Cicala C, de Luca Tupputi Schinosa L (2009) D-dimers are not always elevated in patients with acute aortic dissection. J Cardiovasc Med (Hagerstown) 10(2):212–214
Vilacosta I, San Roman JA, Ferreiros J, Aragoncillo P, Mendez R, Castillo JA, Rollan MJ, Batlle E, Peral V, Sanchez-Harguindey L (1997) Natural history and serial morphology of aortic intramural hematoma: a novel variant of aortic dissection. Am Heart J 134(3):495–507
Noda M, Yamada E, Ikejiri N et al (2009) Study on the clinical utility of D-dimer in diagnosis of DIC. Int J Lab Hematol 10(2):189–195
Acknowledgments
We would like to thank the staff of our department for their support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hagiwara, A., Shimbo, T., Kimira, A. et al. Using fibrin degradation products level to facilitate diagnostic evaluation of potential acute aortic dissection. J Thromb Thrombolysis 35, 15–22 (2013). https://doi.org/10.1007/s11239-012-0779-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-012-0779-6