Abstract
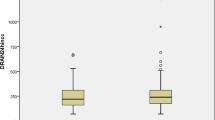
Background Aspirin administered early after coronary artery bypass grafting surgery (CABG) improves graft patency and patients survival. However, the antiplatelet effect of aspirin seems to be variable and aspirin resistance is currently still being discussed. The aim of the study was to assess aspirin efficacy in the early postoperative period. Methods Forty patients undergoing elective CABG surgery (20 in on-pump and 20 in off-pump) were enrolled in the study. Functional and biochemical responses to aspirin were evaluated by arachidonic acid (ARA)-induced platelet aggregation and urine 11-dehydro Thromboxane B2 metabolite excretion. Samples were collected before surgery (baseline; ≥7 days after aspirin withdrawal) and on days 1, 2 and 5 after surgery. Results Median baseline ARA aggregability was 55%. On day 1, platelet aggregability decreased (12%, P < 0.001). On day 2, despite the aspirin administration, platelet aggregability exceeded the values from day 1 (38%, P < 0.001). Only on day 5, sufficient inhibition of platelet aggregation was achieved (8%, P < 0.001). Median preoperative urine concentration of 11-dehydroTxB2 was 106 ng/mmol of creatinine. On day 1, the concentration decreased only slightly and insignificantly (97 ng/ml, P = NS), similarly as on day 2 (86 ng/ml, P = NS). Only on day 5, significant decrease in concentration of thromboxane metabolite was achieved compared to preoperative values (46 ng/ml, P = 0.001). Conclusion Aspirin did not sufficiently inhibit platelet aggregation and thromboxane formation in the early postoperative period. Thus, antiplatelet treatment strategy should be intensified or modified in patients early after bypass surgery.


Similar content being viewed by others
References
Mangano DT (2002) Aspirin and mortality from coronary bypass surgery. N Engl J Med 347:1309–1317
Stein PD, Schunemann HJ, Dalen JE et al (2004) Antithrombotic therapy in patients with saphenous vein and internal mammary artery bypass grafts: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 126:600S–608S
Zimmermann N, Kienzle P, Weber AA et al (2001) Aspirin resistance after coronary artery bypass grafting. J Thorac Cardiovasc Surg 121:982–984
Zimmermann N, Wenk A, Kim U et al (2003) Functional and biochemical evaluation of platelet aspirin resistance after coronary artery bypass surgery. Circulation 108:542–547
Lordkipanidze M, Pharand C, Schampaert E et al (2007) A comparison of six major platelet function tests to determine the prevalence of aspirin resistance in patients with stable coronary artery disease. Eur Heart J 28:1702–1708
Cattaneo M (2007) Laboratory detection of ‘aspirin resistance’: what test should we use (if any)? Eur Heart J 28:1673–1675
Muriithi EW, Belcher PR, Day SP et al (2000) Heparin-induced platelet dysfunction and cardiopulmonary bypass. Ann Thorac Surg 69:1827–1832
DiChiara J, Bliden KP, Tantry US et al (2007) The effect of aspirin dosing on platelet function in diabetic and nondiabetic patients: an analysis from the aspirin-induced platelet effect (ASPECT) study. Diabetes 56:3014–3019
FitzGerald GA, Reilly IA, Pedersen AK (1985) The biochemical pharmacology of thromboxane synthase inhibition in man. Circulation 72:1194–1201
Fritsma GA, Ens GE, Alvord MA et al (2001) Monitoring the antiplatelet action of aspirin. JAAPA 14:57–58, 61–62
Catella F, FitzGerald GA (1987) Paired analysis of urinary thromboxane B2 metabolites in humans. Thromb Res 47:647–656
Eikelboom JW, Hirsh J, Weitz JI et al (2002) Aspirin-resistant thromboxane biosynthesis and the risk of myocardial infarction, stroke, or cardiovascular death in patients at high risk for cardiovascular events. Circulation 105:1650–1655
Vane JR, Bakhle YS, Botting RM (1998) Cyclooxygenases 1 and 2. Ann Rev Pharmacol Toxicol 38:97–120
Maree AO, Fitzgerald DJ (2007) Variable platelet response to aspirin and clopidogrel in atherothrombotic disease. Circulation 115:2196–2207
Acknowledgement
The study was supported by Research grant no. 8526-3/2005 from the Internal Grant Agency of the Ministry of Health of the Czech Republic.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bednar, F., Osmancik, P., Hlavicka, J. et al. Aspirin is insufficient in inhibition of platelet aggregation and thromboxane formation early after coronary artery bypass surgery. J Thromb Thrombolysis 27, 394–399 (2009). https://doi.org/10.1007/s11239-008-0225-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-008-0225-y