Abstract
Background
Myocardial infarction and stroke (arterial thrombosis) comprise the leading killers and sources of disability in the developed world, and incomplete thrombolysis along with high bleeding rates (plus late presentations to cathlabs) have prompted an intensive search for alternative or adjunctive emergency therapies. Transcutaneous ultrasound has been studied in remediation of thrombosis, but has been problematic due to poor penetration, risk of arterial damage, plus the apparent need for a highly skilled approach. Surprisingly there has been no reported studies on the much simpler application of transcutaneous low frequency vibration (well known for its superior penetration and flow enhancing characteristics) to assist arterial thrombolysis. The aim of our experiment therefore was to test the hypothesis whether vibration (i.e. ∼100 Hz, 0.5 mm), when applied across an attenuating barrier, would assist recanulization of a thrombosed flow system held at arterial like pressure.
Methods
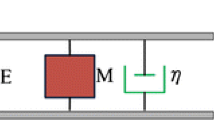
A teddy bear with a 2 cm slab of New York Steak placed upon its chest surface was used as a test subject with an in-dwelling catheter (∼4.0 mm lumen) cannulated through the bear’s thorax. In a series of test runs (n = 30), a 2 h old (or older) blood clot was injected into the catheter such as to occlude it at a stenosis site (∼90% luminal narrowing) created by a clamp placed along the catheter within the teddy’s chest region. A pressurized heparinized IV system was in all cases connected to the catheter such as to yield an “arterial like” lumen pressure proximal the obstruction. For each test run, after a twenty minute observation period to confirm stability of the occlusion, test groups where randomized to receive vibration to the slab of steak upon the teddy’s “chest wall” (generally overlying the site of the thrombotic obstruction), or no vibration for an evaluation period of up to 45 min.
Results
Catheter reflow occurred rapidly (median reflow-time 90 s) in the vibration groups within the evaluation period (i.e. 15/17), while the system remained otherwise blocked in the control groups receiving no vibration (i.e. 0/13). The difference in flow system patency rate for the vibration groups vs. the control groups was statistically significant (P = 0.0000009).
Conclusions
The frequent and generally rapid re-establishment of flow in vibration groups compared to the complete absence of reflow in control groups confirms the hypothesis that vibration applied across a physical barrier assists clearance of a blood clot in a stenosed flow system under systemic levels of pressure.
Abbreviated abstract
We studied the incidence of clearance of a blood clot within a stenosed, heparanized catheter system held at arterial like pressure that was treated with externally delivered low frequency vibration (applied proximate the thrombotic occlusion across an attenuating medium––a 2 cm thick slab of New York Steak––at ∼100 Hz, 0.5 mm), versus no vibration. Reflow in test runs incorporating vibration occurred faster, and resulted in significantly greater recanulization rates in the catheter system versus test runs without vibration (P = 0.0000009). Non-invasive vibration holds potential as an adjunct to pharmacologic therapy in treatment of acute arterial thrombosis. Further study of this technique appears warranted in live animal models.


Similar content being viewed by others
References
Lincoff AM, Topol EJ (1993) Illusion of reperfusion. Does anyone achieve optimal reperfusion during acute myocardial infarction? Circulation 88:1361–1374
The National Institute of Neurological Disorders and Stroke t-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333:1581–1587
Stone GW, Cox D, Garcia E et al (2001) Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction. Circulation 104:636–641
Cannon CP (2001) Importance of TIMI 3 flow. Circulation (Editorial) 104:624–626
Ross AM, Coyne KS, Moreyra E et al (1998) Extended mortality benefit of early postinfarction reperfusion. GUSTO-I Angiopgraphic Investigators. Global Utilization of streptokinase and tissue plasminogen activator for occluded coronary arteries trial. Circulation 97:1549–1556
Anderson JL, Karagounis LA, Becker LC, Sorensen SG, Menlove RL (1993) TIMI perfusion grade 3 but not grade 2 results in improved outcome after thrombolytisis for myocardial infarction. Ventriculographic, enzymatic, and electrocardiographic evidence from the TEAM 3 Study. Circulation 87:1829–1839
Llevadot J, Giugliano RP, Antman EM (2001) Bolus fibrionolytic therapy in acute myocardial infarction. J Am Med Assoc 286(4):442–449
Molina CA, Ribo M, Rubiera M et al (2006) Microbubble administration accelerates clot lysis during continuous 2-MHz ultrasound monitoring in stroke patients treated with intravenous tissue plasminogen activator. Stroke 37(2):425–429
Saver JL (2006) Time is brain-quantified. Stroke 37(1):263–266
Jacobs AK. Speedy angioplasty urged for more heart attack patients. American Heart Association Consensus Statement. 2006; Report, http://www.americanheart.org
Woo MA (1992) Clinical management of the patient with an acute myocardial infarction. Nurs Clin North Am 27(1):189–203
NG KY, Liu Y (2002) Therapeutic ultrasound: its application in drug delivery. Med Res Rev 22(2):204–223
Alexandrov AV, Molina CA, Grotta JC (CLOTBUST Investigators) et al (2004) Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med 351(21):2170–2178
Cohen MG, Tuero E, Bluguermann J et al (2003) Transcutaneous ultrasound-facilitated coronary thrombolysis during acute myocardial infarction. Am J Cardiol 92(4):454–457
Daffertshofer M, Gass A, Ringleb P et al (2005) Transcranial low-frequency ultrasound-mediated thrombolysis in brain ischemia: increased risk of hemorrhage with combined ultrasound and tissue plasminogen activator: results of a phase II clinical trial. Stroke 36(7):1441–1446
Wells PM (1975) Review. Absorption and dispersion of ultrasound in biological tissue. Ultrasound Med Biol 1:369–376
Pfaffenberger S, Devcic-Kuhar B, Kollmann C et al (2005) Can a commercial diagnostic ultrasound device accelerate thrombolysis? An in vitro skull model. Stroke 36(1):124–128
Frizzel LA, Miller DL, Nyborg WL (1986) Ultrasonically induced intravascular streaming and thrombus formation adjacent to a micropipette. Ultrasound Med Biol 12(3):217–221
Kornowski R, Meltzer R (1994) Does external ultrasound accelerate thrombolysis? Results from a rabbit model. Circulation 89:339–344
Mukherjee D, Wong J, Griffin B (2000) Ten fold augmentation of endothelial uptake of vascular endothelial growth factor with ultrasound after systemic administration. J Am Coll Cordiol 35(6):1678–1686
Riggs PN, Francis CW, Bartos SR, Penney DP (1997) Ultrasound enhancement of rabbit femoral artery thrombolysis. Cardiovasc Surg 5(2):201–207
Nishioka T, Luo H, Fishbein MC et al (1997) Dissolution of thrombotic arterial occlusion by high intensity, low frequency ultrasound and dodecafluoropentane emulsion: an in vitro and in vivo study. J Am Coll Cordiol 30(2):561–568
Luo H, Nishioka T, Fishbein MC et al (1996) Transcutaneous ultrasound augments lysis of arterial thrombi in vivo. Circulation 94:775–778
Kerr CL, Gregory DW, Chan KK, Wattmough DJ, Wheatly DN (1989) Ultrasound-induced damage of veins in pig ears, as revealed by scanning electron microscopy. Ultrasound Med Biol 15:45–52
Koiwa Y, Honda H, Takagi T, Kikuchi J, Hoshi N, Takishima T (1997) Modification of human left ventricular relaxation by small-amplitude, phase–controlled mechanical vibration on the chest wall. Circulation 95:156–162
Thomas J, Cook DJ, Brooks D (1995) Chest physical therapy management of patients with cystic fibrosis: a meta analysis. Am J Respir Crit Care Med 151:846–850
Koiwa Y, Hashiguchi R, Ohyama T et al (1986) Measurement of instantaneous viscoelastic properties by impedance-frequency curve of the ventricle. Am J Physiol 250:H672–H684
Hashiguchi R, Koiwa Y, Ohyama T et al (1988) Dependence of instantaneous transfer function on regional ischemic myocardial volume. Circ Res 63:1003–1011
Smith D, Ishimitsu T, Craige E (1984) Mechanical vibration transmission characteristics of the left ventricle. implication with regard to auscultation and phonocardiography. J Am Coll Cordiol 4(3):517–521
Farber JJ, Purvis JH (1963) Conduction of cardiovascular sound along arteries. Circ Res 12:308–316
Wobser E, Stumpff U (1978) Intragastral disintegration of blood coagula by mechanical vibration. Endoscopy 10:15–19
Dubrul WR, Evans MA (2001) Motion catheter. US Patent 6,287,271
Folts J (1991) An in vivo model of experimental arterial stenosis, intimal damage, and periodic thrombosis. Circulation 83(IV):IV-3–IV-14
Folts J (2000) Contemporary cardiology vascular disease and injury preclinical research (Chap. 11). Humana Press Inc., Totowa, NJ, pp 127–145
Antman EM, Anbe DT, Armstrong PW et al (2004) ACC/AHA guidelines for the management of patient’s with STEMI: executive summary. J Am Coll Cardiol 44(3):671–719
Lindblad LE, Lorenz RR, Shepherd JT, Vanhoutte PM (1986) Effect of vibration on canine cutaneous artery. Heart Circ Physiol 19:H519–H523
Ljung B, Silvertsson R (1975) Vibration-induced inhibition of vascular smooth muscle contraction. Blood Vessels 12:38–52
Hudlicka O, Wright A (1978) The effect of vibration on blood flow in skeletal muscle in rabbit. Clin Sci Mol Med 55:471–476
Koiwa Y, Honda H, Hoshi N, Naya T, Kamada E. The effect of diastolic vibration on the coronary flow rate in the canine heart with ischemia. J Cardiovasc Diagn Procedures 1994; Abstract (FRI – POS 05)12:110
Naya T, Koiwa Y, Honda H et al Diastolic vibration from the precordium increases coronary blood flow in humans. J Cardiovasc Diagn Procedures 1994; Abstract (FRI – POS07) 12:110
Bozeman WP, Kleiner DM, Ferguson KL (2006) Empiric tenecteplase is associated with increased return of spontaneous circulation and short term survival in cardiac arrest patients unresponsive to standard interventions. Resuscitation 69(3):399–406
Takashima H, Tsuruta H, Higashi T, Watanabe M, Isomoto A, Tyuma I. Effects of mechanical force on blood fibrinolytic activity. Thromb Haemost 1987; Abstract 58:550
Tarnay TJ, Rohr PR, Davidson AG, Stevenson MM, Byars EF, Hopkins GR (1980) Pneumatic calf compression, fibrinolysis, and the prevention of deep venous thrombosis. Surgery 88(4):489–496
Adams JA, Bassuk J, Dongmei W, Grana M, Kurlansky P, Sackner M (2005) Periodic acceleration: effects on vasoactive, fibrinolytic, and coagulation factors. J Appl Physiol 98:1083–1090
Takagi T, Koiwa Y, Kikuchi J et al (1992) Diastolic vibration improves systolic function in cases of incomplete relaxation. Circulation 86:1955–1964
Koiwa Y, Takagi T, Kikuchi H, Honda H, Hoshi N, Takishima T (1989) The improvement of systolic function of depressed left ventricle by external vibration at diastole. Tohoku J Exp Med 159:169–170
Silver MC, Baroldi G, Marian F (1980) The relationship between acute occlusive coronary thrombi and myocardial infarction studied in 100 consecutive patients. Circulation 61(2):219–227
Hackett D, Davies G, Chierchia S, Maseri A (1987) Intermittent coronary occlusion in acute myocardial infarction. N Engl J Med 317(17):1055–1059
Dalen JE, Ockene IS, Alpert JS (1982) Coronary spasm, coronary thrombosis, and myocardial infarction: a hypothesis concerning the pathophysiology of acute myocardial infarction. Am Heart J 104(5):1119–1124
Oliva PB, Breckinridge JC (1977) Arteriographic evidence of coronary arterial spasm in acute myocardial infarction. Circulation 56(3):367–374
Maseri A, L’Abbate A, Baroldi G et al (1978) Coronary vasospasm as a possible cause of myocardial infarction. N Engl J Med 299(23):1271–1277
Marder VJ, Chute DJ, Starkman S et al (2006) Analysis of thrombi retrieved from cerebral arteries of patients with acute ischemic stroke. Stroke 37(8):2086–2093
Acknowledgements
The author gratefully thanks Dr. C. Michael Gibson for his peer review and Dr. Dante Manyari for his advice in the drafting of this manuscript. Also, many thanks to the Royal Columbian (Cardiac Cath Lab) and Surrey Memorial Hospital (Laboratory) for the loan and donation of select equipment and supplies and assistance in blood collection which made this study possible. This study was otherwise sponsored by Ahof Biophysical Systems Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yohannes, F.G., Hoffmann, A.K. Non-invasive low frequency vibration as a potential emergency adjunctive treatment for heart attack and stroke. An in vitro flow model. J Thromb Thrombolysis 25, 251–258 (2008). https://doi.org/10.1007/s11239-007-0054-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-007-0054-4