Abstract
Purpose
The asthma stepwise treatment approach recommended is based on monitoring patients’ symptoms. The Asthma Research in Children and Adolescents (ARCA) cohort was created to provide evidence about the evolution of persistent asthma. This manuscript describes the development of an electronic health tool, comprising a mobile health application for patients with asthma and its associated online platform for pediatricians to monitor them.
Methods
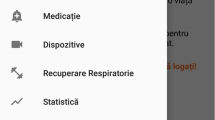
The development process followed 7 phases: the first 5 (Conceptualization, Preparation, Assessment scheduling, Image and user interface, and Technical development) defined and designed the tool, followed by a testing phase (functionality assessment and pilot test with ARCA patients), and a last phase which evaluated usability. Since the target population was aged 6–16 years, three versions were designed within the same smartphone application: parents/proxy, children, and adolescents. The online platform for pediatricians provides real-time information from the application: patients’ responses over time with color-coded charts (red/amber/green, as in traffic lights).
Results
The pilot test through semi-structured phone interviews of the first 50 participants included in the ARCA study (n = 53) detected their misunderstandings. Pediatricians were trained to emphasize that the application is free of charge and requires monthly answers. Median of the System Usability Scale scores (n = 85), ranging 0 (negative)–100 (positive), was > 93 in the three age versions of the application.
Conclusions
Technology has the capability of transforming the use of patient-reported outcomes. Describing all the development phases of a mobile health application for monitoring children and adolescents with asthma may increase the knowledge on how to design applications for young patients.






Similar content being viewed by others
References
World Health Organization. (n.d.). The Global Asthma Report 2018. Retrieved from www.globalasthmanetwork.org.
Asher, I., & Pearce, N. (2014). Global burden of asthma among children. International Journal of Tuberculosis and Lung Disease, 18(11), 1269–1278. https://doi.org/10.5588/ijtld.14.0170.
Global Iniciative for Asthma Management and Prevention. Guide for Health Professionals (for Adults and Children Older than 5 Years). (2019). Retrieved October 24, 2019, from https://ginasthma.org/wp-content/uploads/2019/04/GINA-2019-main-Pocket-Guide-wms.pdf.
Van Ganse, E., Texier, N., Dima, A. L., Laforest, L., Ferrer, M., Hernandez, G., … De Bruin, M. (2015). Assessment of the safety of long-acting β2 -agonists in routine asthma care: The ASTRO-LAB protocol. NPJ Primary Care Respiratory Medicine, 25, 1–5. https://doi.org/10.1038/npjpcrm.2015.40.
Dima, A. L., de Bruin, M., & Van Ganse, E. (2016). Mapping the Asthma care process: Implications for research and practice. Journal of Allergy and Clinical Immunology: In Practice, 4(5), 868–876. https://doi.org/10.1016/j.jaip.2016.04.020.
Mazalovic, K., Jacoud, F., Dima, A. L., Van Ganse, E., Nolin, M., Didier, C., … Group, the A. L. (2018). Asthma exacerbations and socio-economic status in French adults with persistent asthma: A prospective cohort study. Journal of Asthma, 55(10), 1043–1051.https://doi.org/10.1080/02770903.2017.1391280.
de Bruin, M., Dima, A. L., Texier, N., & van Ganse, E. (2018). Explaining the amount and consistency of medical care and self-management support in Asthma: A survey of primary care providers in France and the United Kingdom. Journal of Allergy and Clinical Immunology: In Practice, 6(6), 1916-1925.e7. https://doi.org/10.1016/j.jaip.2018.04.039.
Hernandez, G., Dima, A. L., Pont, À., Garin, O., Martı, M., Alonso, J., … Ferrer, M. (2018). Impact of asthma on women and men : Comparison with the general population using the EQ-5D-5L questionnaire. PLoS ONE, 13(8), 1–18.
Dima, A. L., van Ganse, E., Stadler, G., & de Bruin, M. (2019). Does adherence to inhaled corticosteroids predict asthma-related outcomes over time? A cohort study. European Respiratory Journal. https://doi.org/10.1183/13993003.00901-2019.
Hernandez, G., Garin, O., Dima, A. L., Pont, A., Martí Pastor, M., Alonso, J., … Ferrer, M. (2019). EuroQol (EQ-5D-5L) Validity in assessing the quality of life in adults with Asthma: Cross-sectional study. Journal of Medical Internet Research, 21(1), e10178. https://doi.org/10.2196/10178.
Anderson, L. M., Papadakis, J. L., Vesco, A. T., Shapiro, J. B., Feldman, M. A., Evans, M. A., & Weissberg-Benchell, J. (2019). Patient-reported and parent proxy-reported outcomes in pediatric medical specialty clinical settings: A systematic review of implementation. Journal of Pediatric Psychology. https://doi.org/10.1093/jpepsy/jsz082.
Chen, J., Ou, L., & Hollis, S. J. (2013). A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Services Research, 13(1), 1–24. https://doi.org/10.1186/1472-6963-13-211.
Matza, L. S., Patrick, D. L., Riley, A. W., Alexander, J. J., Rajmil, L., Pleil, A. M., & Bullinger, M. (2013). Pediatric patient-reported outcome instruments for research to support medical product labeling: Report of the ISPOR PRO good research practices for the assessment of children and adolescents task force. Value in Health, 16(4), 461–479. https://doi.org/10.1016/j.jval.2013.04.004.
Varni, J. W., Thissen, D., Stucky, B. D., Liu, Y., Magnus, B., He, J., … DeWalt, D. A. (2015). Item-level informant discrepancies between children and their parents on the PROMIS® pediatric scales. Quality of Life Research, 24(8), 1921–1937. https://doi.org/10.1007/s11136-014-0914-2.
Jardine, J., Glinianaia, S. V., McConachie, H., Embleton, N. D., & Rankin, J. (2014). Self-reported quality of life of young children with conditions from early infancy: A systematic review. Pediatrics, 134(4), 1129–1148. https://doi.org/10.1542/peds.2014-0352.
Eiser, C., & Morse, R. (2001). A review of measures of quality of life for children with chronic illness. Archives of Disease in Childhood, 84(3), 205–211. https://doi.org/10.1136/adc.84.3.205.
Ofcom. (2016). Communications Market Report 2018. Retrieved from http://www.ofcom.org.uk/research/cm/cmr08/.
Research2Guidance—mHealth Economics 2017—Current Status and Future Trends in Mobile Health. (n.d.). Retrieved October 29, 2019, from https://research2guidance.com/product/mhealth-economics-2017-current-status-and-future-trends-in-mobile-health/.
Farzandipour, M., Nabovati, E., Sharif, R., Arani, M. H., & Anvari, S. (2017). Patient self-management of asthma using mobile health applications: A systematic review of the functionalities and effects. Applied Clinical Informatics, 8(4), 1068–1081. https://doi.org/10.4338/ACI-2017-07-R-0116.
Marcano Belisario, J., Huckvale, K., Greenfield, G., Cat, J., & Gunn, L. (2013). Smartphone and tablet self management apps for asthma. Cochrane Database of Systematic Reviews, (11). https://doi.org/10.1002/14651858.CD010013.pub2.
Chi Yan, H., Robert, W., Brian, M., Tracy, J., Richard, P., & Hilary, P. (2017). The use of mobile applications to support self-management for people with asthma: A systematic review of controlled studies to identify features associated with clinical effectiveness and adherence. Journal of the American Medical Informatics Association, 24(3), 619–632. https://doi.org/10.1093/jamia/ocw143.
Unni, E., Gabriel, S., & Ariely, R. (2018). A review of the use and effectiveness of digital health technologies in patients with asthma. Annals of Allergy, Asthma and Immunology, 121(6), 680–691. https://doi.org/10.1016/j.anai.2018.10.016.
Burbank, A. J., Lewis, S. D., Hewes, M., Schellhase, D. E., Rettiganti, M., Hall-Barrow, J., … Perry, T. T. (2015). Mobile-based asthma action plans for adolescents. Journal of Asthma, 52(6), 583–586.https://doi.org/10.3109/02770903.2014.995307.
Perry, T. T., Marshall, A., Berlinski, A., Rettiganti, M., Brown, R. H., Randle, S. M., … Bian, J. (2017). Smartphone-based vs paper-based asthma action plans for adolescents. Annals of Allergy, Asthma and Immunology, 118(3), 298–303.https://doi.org/10.1016/j.anai.2016.11.028.
Mosnaim, G., Li, H., Martin, M., Richardson, D. J., Belice, P. J., Avery, E., … Powell, L. H. (2015). A tailored mobile health intervention to improve adherence and asthma control in minority adolescents. Journal of Allergy and Clinical Immunology: In Practice, 3(2), 288–290. https://doi.org/10.1016/j.jaip.2014.10.011.
Roberts, C. A., Geryk, L. L., Sage, A. J., Sleath, B. L., Tate, D. F., & Carpenter, D. M. (2016). Adolescent, caregiver, and friend preferences for integrating social support and communication features into an asthma self-management app. Journal of Asthma, 53(9), 948–954. https://doi.org/10.3109/02770903.2016.1171339.
Carpenter, D. M., Geryk, L. L., Sage, A., Arrindell, C., & Sleath, B. L. (2016). Exploring the theoretical pathways through which asthma app features can promote adolescent self-management. Translational Behavioral Medicine, 6(4), 509–518. https://doi.org/10.1007/s13142-016-0402-z.
Merchant, R. K., Inamdar, R., & Quade, R. C. (2016). Effectiveness of population health management using the propeller health asthma platform: A randomized clinical trial. Journal of Allergy and Clinical Immunology: In Practice, 4(3), 455–463. https://doi.org/10.1016/j.jaip.2015.11.022
Zairina, E., Abramson, M. J., McDonald, C. F., Li, J., Dharmasiri, T., Stewart, K., … George, J. (2016). Telehealth to improve asthma control in pregnancy: A randomized controlled trial. Respirology, 21(5), 867–874. https://doi.org/10.1111/resp.12773.
Cingi, C., Yorgancioglu, A., Cingi, C. C., Oguzulgen, K., Muluk, N. B., Ulusoy, S., … Aksoy, M. A. (2015). The “physician on call patient engagement trial” (POPET): Measuring the impact of a mobile patient engagement application on health outcomes and quality of life in allergic rhinitis and asthma patients. International Forum of Allergy and Rhinology, 5(6), 487–497.https://doi.org/10.1002/alr.21468.
Ryan, D., Price, D., Musgrave, S. D., Malhotra, S., Lee, A. J., Ayansina, D., … Pinnock, H. (2012). Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: Multicentre randomised controlled trial. BMJ (Online), 344(7854), 1–15.https://doi.org/10.1136/bmj.e1756.
Dima, A. L., van Ganse, E., Laforest, L., Texier, N., de Bruin, M., & the ASTRO-LAB group. (2017). Measuring medication adherence in asthma: Development of a novel self-report tool. Psychology and Health, 32(10), 1288–1307. https://doi.org/10.1080/08870446.2017.1290248.
Gray, W. N., Netz, M., McConville, A., Fedele, D., Wagoner, S. T., & Schaefer, M. R. (2018). Medication adherence in pediatric asthma: A systematic review of the literature. Pediatric Pulmonology, 53(5), 668–684. https://doi.org/10.1002/ppul.23966.
Toelle, B. G., Dunn, S. M., & Marks, G. B. (2004). A validated inhaler adherence scale. American Journal of Respiratory and Critical Care Medicine, 169(7 Supp), A325.
Abramson, M. J., Schattner, R. L., Holton, C., Simpson, P., Briggs, N., Beilby, J., … Massie, R. J. (2014). Spirometry and regular follow-up do not improve quality of life in children or adolescents with asthma: Cluster randomized controlled trials. Pediatric Pulmonology, 50(10), 947–954. https://doi.org/10.1002/ppul.23096.
Wood, B. L., Cheah, P. A., Lim, J. H., Ritz, T., Miller, B. D., Stern, T., & Ballow, M. (2007). Reliability and validity of the asthma trigger inventory applied to a pediatric population. Journal of Pediatric Psychology, 32(5), 552–560. https://doi.org/10.1093/jpepsy/jsl043.
Ritz, T., Steptoe, A., Bobb, C., Harris, A. H. S., & Edwards, M. (2006). The Asthma Trigger Inventory: Validation of a questionnaire for perceived triggers of asthma. Psychosomatic Medicine, 68(6), 956–965. https://doi.org/10.1097/01.psy.0000248898.59557.74.
Moss-Morris, R., Weinman, J., Petrie, K., Horne, R., Cameron, L., & Buick, D. (2002). The revised Illness Perception Questionnaire (IPQ-R). Psychology and Health, 17(1), 1–16. https://doi.org/10.1080/08870440290001494.
Pacheco-Huergo, V., Viladrich, C., Pujol-Ribera, E., Cabezas-Peña, C., Núñez, M., Roura-Olmeda, P., … Del Val, J. L. (2012). Percepción en enfermedades crónicas: Validación lingüística del Illness Perception Questionnaire Revised y del Brief Illness Perception Questionnaire para la población española. Atencion Primaria, 44(5), 280–287. https://doi.org/10.1016/j.aprim.2010.11.022.
Broadbent, E., Wilkes, C., Koschwanez, H., Weinman, J., Norton, S., & Petrie, K. J. (2015). A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychology and Health, 30(11), 1361–1385. https://doi.org/10.1080/08870446.2015.1070851.
Horne, R., Weinman, J., & Hankins, M. (1999). The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health, 14(1), 1–24. https://doi.org/10.1080/08870449908407311.
Ahmed, S., Ernst, P., Bartlett, S. J., Valois, M. F., Zaihra, T., Paré, G., … Tamblyn, R. (2016). The effectiveness of web-based asthma self-management system, my asthma portal (MAP): A pilot randomized controlled trial. Journal of Medical Internet Research, 18(12). https://doi.org/10.2196/jmir.5866
Juniper, E. F., Gruffydd-Jones, K., Ward, S., & Svensson, K. (2010). Asthma control questionnaire in children: Validation, measurement properties, interpretation. European Respiratory Journal, 36(6), 1410–1416. https://doi.org/10.1183/09031936.00117509.
Cloutier, M. M., Schatz, M., Castro, M., Clark, N., Kelly, H. W., Mangione-Smith, R., … Gergen, P. (2012). Asthma outcomes: Composite scores of asthma control. Journal of Allergy and Clinical Immunology, 129, 24–33. https://doi.org/10.1016/j.jaci.2011.12.980.
Jia, C. E., Zhang, H. P., Lv, Y., Liang, R., Jiang, Y. Q., Powell, H., … Wang, G. (2013). The asthma control test and asthma control questionnaire for assessing asthma control: Systematic review and meta-analysis. Journal of Allergy and Clinical Immunology, 131(3), 695–703. https://doi.org/10.1016/j.jaci.2012.08.023.
Gibeon, D., Heaney, L. G., Brightling, C. E., Niven, R., Mansur, A. H., Chaudhuri, R., … Menzies-Gow, A. N. (2015). Dedicated severe asthma services improve health-care use and quality of life. Chest, 148(4), 870–876. https://doi.org/10.1378/chest.14-3056.
Voorend-Van Bergen, S., Vaessen-Verberne, A. A., De Jongste, J. C., & Pijnenburg, M. W. (2015). Asthma control questionnaires in the management of asthma in children: A review. Pediatric Pulmonology, 50(2), 202–208. https://doi.org/10.1002/ppul.23098.
Szefler, S. J. (2015). Advances in pediatric asthma in 2014: Moving toward a population health perspective. Journal of Allergy and Clinical Immunology, 135(3), 644–652. https://doi.org/10.1016/j.jaci.2014.12.1921.
Linnemann, D., Salas, Hernández, J., Vázquez, García, J., Ortiz, … Be. (2017). Guía Mexicana del Asma: GUIMA 2017. Revista Alergia Mexico, 64(1), 11–128. Retrieved from http://www.revistaalergia.mx.
Nathan, R. A., Sorkness, C. A., Kosinski, M., Schatz, M., Li, J. T., Marcus, P., … Pendergraft, T. B. (2004). Development of the Asthma Control Test: A survey for assessing asthma control. Journal of Allergy and Clinical Immunology, 113(1), 59–65. https://doi.org/10.1016/j.jaci.2003.09.008.
Allen, E. D., Arcoleo, K., Rowe, C., & Long, W. W. (2018). Implementation of a “real world” School-Based Asthma Therapy program targeting urban children with poorly controlled asthma. Journal of Asthma, 55(10), 1122–1130. https://doi.org/10.1080/02770903.2017.1396472.
Hoeksema, L. J., Bazzy-Asaad, A., Lomotan, E. A., Edmonds, D. E., Ramírez-Garnica, G., Shiffman, R. N., & Horwitz, L. I. (2011). Accuracy of a computerized clinical decision-support system for asthma assessment and management. Journal of the American Medical Informatics Association, 18(3), 243–250. https://doi.org/10.1136/amiajnl-2010-000063.
Zemedkun, K., Woldemichael, K., & Tefera, G. (2014). Assessing control of asthma in Jush, Jimma, South West Ethiopia. Ethiopian Journal of Health Sciences, 24(1), 49–58. https://doi.org/10.4314/ejhs.v24i1.7.
Vega, J. M., Badia, X., Badiola, C., López-Viña, A., Olaguíbel, J. M., Picado, C., … Dal-Ré, R. (2007). Validation of the Spanish version of the asthma control test (ACT). Journal of Asthma, 44(10), 867–872.https://doi.org/10.1080/02770900701752615.
Piacentini, G. L., Cattazzo, E., Tezza, G., & Peroni, D. G. (2012). Exhaled nitric oxide in pediatrics: What is new for practice purposes and clinical research in children? Journal of Breath Research. https://doi.org/10.1088/1752-7155/6/2/027103.
Pike, K. C., Levy, M. L., Moreiras, J., & Fleming, L. (2018). Managing problematic severe asthma: Beyond the guidelines. Archives of Disease in Childhood, 103(4), 392–397. https://doi.org/10.1136/archdischild-2016-311368.
Boonsawat, W., & Thinkhamrop, B. (2015). Evaluation of asthma control by inhaled corticosteroids in general practice in Thailand. Asian Pacific Journal of Allergy and Immunology, 33(1), 21–25. https://doi.org/10.12932/AP0435.33.1.2015.
Y Xing, N Li, W Zhou, X Huang, Z H Jiang, L Liu, & H L Bao. (2014). Analysis of the Control Level and the Affecting Factors in 4–11 Years Old Children With Asthma. Beijing Da Xue Xue Bao Yi Xue Ban, 18(46), 936–940. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25512287/.
Heffler, E., Crimi, C., Campisi, R., Sichili, S., Nicolosi, G., Porto, M., … Crimi, N. (2016). Bronchodilator response as a marker of poor asthma control. Respiratory Medicine, 112, 45–50. https://doi.org/10.1016/j.rmed.2016.01.012.
Liu, A. H., Babineau, D. C., Krouse, R. Z., Zoratti, E. M., Pongracic, J. A., O’Connor, G. T., … Busse, W. W. (2016). Pathways through which asthma risk factors contribute to asthma severity in inner-city children. Journal of Allergy and Clinical Immunology, 138(4), 1042–1050. https://doi.org/10.1016/j.jaci.2016.06.060.
Menzies-Gow, A., & Chiu, G. (2017). Perceptions of asthma control in the United Kingdom: a cross-sectional study comparing patient and healthcare professionals’ perceptions of asthma control with validated ACT scores. Npi Primary Care Respiratory Medicine. https://doi.org/10.1038/s41533-017-0050-x.
Liu, A. H., Zeiger, R., Sorkness, C., Mahr, T., Ostrom, N., Burgess, S., … Manjunath, R. (2007). Development and cross-sectional validation of the Childhood Asthma Control Test. Journal of Allergy and Clinical Immunology, 119(4), 817–825. https://doi.org/10.1016/j.jaci.2006.12.662.
Arakawa, H., Hamasaki, Y., Kohno, Y., Ebisawa, M., Kondo, N., Nishima, S., … Morikawa, A. (2017). Japanese guidelines for childhood asthma 2017. Allergology International, 66(2), 190–204. https://doi.org/10.1016/j.alit.2016.11.003.
Carroll, W. (2013). Limitations of asthma control questionnaires in the management and follow up of childhood asthma. Paediatric Respiratory Reviews, 14(4), 229–231. https://doi.org/10.1016/j.prrv.2013.06.007.
Pedersen, S. (2016). Asthma control in children: Is it important and can we measure it? Paediatric Respiratory Reviews, 17, 36–38. https://doi.org/10.1016/j.prrv.2015.08.009.
Verkleij, M., Beelen, A., van Ewijk, B. E., & Geenen, R. (2016). Multidisciplinary treatment in children with problematic severe asthma: A prospective evaluation. Pediatric Pulmonology, 52(5), 588–597. https://doi.org/10.1002/ppul.23623.
Lee, S. C., Yang, Y. H., Chuang, S. Y., Huang, S. Y., & Pan, W. H. (2013). Reduced medication use and improved pulmonary function with supplements containing vegetable and fruit concentrate, fish oil and probiotics in asthmatic school children: A randomised controlled trial. British Journal of Nutrition, 110(1), 145–155. https://doi.org/10.1017/S0007114512004692.
Murphy, K. R., Zeiger, R. S., Kosinski, M., Chipps, B., Mellon, M., Schatz, M., … Ramachandran, S. (2009). Test for Respiratory and Asthma Control in Kids (TRACK): A caregiver-completed questionnaire for preschool-aged children. Journal of Allergy and Clinical Immunology, 123(4), 833-839.e9. https://doi.org/10.1016/j.jaci.2009.01.058.
Szefler, S. J. (2012). Advances in pediatric asthma in 2011: Moving forward. Journal of Allergy and Clinical Immunology, 129(1), 60–68. https://doi.org/10.1016/j.jaci.2011.11.011.
Horner, S. D., Kieckhefer, G. M., & Fouladi, R. T. (2006). Measuring asthma severity: Instrument refinement. Journal of Asthma, 43(7), 533–538. https://doi.org/10.1080/02770900600857192.
Horner, S. D., Brown, A., Brown, S. A., & Rew, D. L. (2016). Enhancing Asthma self-management in rural school-aged children: A randomized controlled trial. Journal of Rural Health, 32(3), 260–268. https://doi.org/10.1111/jrh.12150.
Guyatt, G. H., Norman, G. R., Juniper, E. F., & Griffith, L. E. (2002). A critical look at transition ratings. Journal of Clinical Epidemiology, 55(9), 900–908. https://doi.org/10.1016/S0895-4356(02)00435-3.
Kamper, S. J., Maher, C. G., & Mackay, G. (2009). Global rating of change scales: A review of strengths and weaknesses and considerations for design. Journal of Manual and Manipulative Therapy, 17(3), 163–170. https://doi.org/10.1179/jmt.2009.17.3.163.
McQuaid, E. L., Penza-Clyve, S. M., Nassau, J. H., Fritz, G. K., Klein, R., O’Connor, S., … Gavin, L. (2001). The Asthma Responsibility Questionnaire: Patterns of Family Responsibility for Asthma Management. Children’s Health Care, 30(3), 183–199. https://doi.org/10.1207/S15326888CHC3003.
Rajmil, L., Roizen, M., Psy, A. U., Hidalgo-Rasmussen, C., Fernández, G., & Dapueto, J. J. (2012). Health-related quality of life measurement in children and adolescents in Ibero-American countries, 2000 to 2010. Value in Health, 15(2), 312–322. https://doi.org/10.1016/j.jval.2011.11.028.
Valderas, J. M., Ferrer, M., Mendívil, J., Garin, O., Rajmil, L., Herdman, M., & Alonso, J. (2008). Development of EMPRO: A tool for the standardized assessment of patient-reported outcome measures. Value in Health, 11(4), 700–708. https://doi.org/10.1111/j.1524-4733.2007.00309.x.
Gibbons, E., & Fitzpatrick, R. (2009). A structured review of patient-reported outcome measures (PROMs) for asthma. The University of Oxford. Retrieved October 12, 2019, from https://phi.uhce.ox.ac.uk/pdf/PROMs_Oxford_Asthma_17092010.pdf.
Yeatts, K. B., Stucky, B., Thissen, D., Irwin, D., Varni, J. W., Dewitt, E. M., … DeWalt, D. (2010). Construction of the Pediatric Asthma Impact Scale (PAIS) for the Patient-Reported Outcomes Measurement Information System (PROMIS). Journal of Asthma, 47(3), 295–302. https://doi.org/10.3109/02770900903426997.Construction.
Roncada, C., Mattiello, R., Pitrez, P. M., & Sarria, E. E. (2013). Specific instruments to assess quality of life in children and adolescents with asthma. Jornal de Pediatria, 89(3), 217–225. https://doi.org/10.1016/j.jped.2012.11.010.
Worth, A., Hammersley, V., Knibb, R., Flokstra-de-Blok, B., DunnGalvin, A., Walker, S., … Sheikh, A. (2014). Patient-reported outcome measures for asthma: A systematic review. NPJ Primary Care Respiratory Medicine, 26(24), 1–7. https://doi.org/10.1038/npjpcrm.2014.20.
Juniper, E. F., Guyatt, G. H., Feeny, D. H., Ferrie, P. J., Griffith, L. E., & Townsend, M. (1996). Measuring quality of life in children with asthma. Quality of Life Research, 5(1), 35–46. https://doi.org/10.1016/S0091-6749(98)70380-X.
Gomersal, T., Harnan, S., Essat, M., Tappenden, P., Wong, R., Lawson, R., … Everard, M. L. (2016). A systematic review of fractional exhaled nitric oxide in the routine management of childhood asthma. Pediatric Pulmonology, 51(3), 316–328. https://doi.org/10.1002/ppul.23371.
Pulgaron, E. R., Salamon, K. S., Patterson, C. A., & Barakat, L. P. (2010). Paediatric—A problem-solving intervention for children with persistent asthma: A pilot of a randomized trial at a pediatric summer camp. Journal of Asthma, 47(9), 1031–1039. https://doi.org/10.1080/02770903.2010.514633.
Cicutto, L., To, T., & Murphy, S. (2013). A Randomized Controlled Trial of a Public Health Nurse-Delivered Asthma Program to. Journal of School Health, 83(12), 876–884.
Juniper, E. F., Guyatt, G. H., Cox, F. M., Ferrie, P. J., & King, D. R. (1999). Development and validation of the Mini Asthma Quality of Life Questionnaire. Clinical and Experimental Allergy, 14(1), 32–38. https://doi.org/10.1034/j.1399-3003.1999.14a08.x.
Gillette, C., Rockich-Winston, N., Kuhn, J. B. A., Flesher, S., & Shepherd, M. (2016). Inhaler technique in children with Asthma: A systematic review. Academic Pediatrics, 16(7), 605–615. https://doi.org/10.1016/j.acap.2016.04.006.
Mahon, J., Fitzgerald, A., Glanville, J., Dekhuijzen, R., Glatte, J., Glanemann, S., & Torvinen, S. (2017). Misuse and/or treatment delivery failure of inhalers among patients with asthma or COPD: A review and recommendations for the conduct of future research. Respiratory Medicine, 129, 98–116. https://doi.org/10.1016/j.rmed.2017.05.004.
Skinner, E. A., Diette, G. B., Algatt-Bergstrom, P. J., Nguyen, T. T. H., Clark, R. D., Markson, L. E., & Wu, A. W. (2004). The asthma therapy assessment questionnaire (ATAQ) for children and adolescents. Disease Management, 7(4), 305–313. https://doi.org/10.1089/dis.2004.7.305.
Ortega, A. N., Belanger, K. D., Bracken, M. B., & Leaderer, B. P. (2001). A childhood asthma severity scale: Symptoms, medications, and health care visits. Annals of Allergy, Asthma and Immunology, 86(4), 405–413. https://doi.org/10.1016/S1081-1206(10)62486-6.
Mishra, A. K., Sengupta, A., & Kumar, K. (2012). Environmental measures in domicilliary interventions of asthmatic children. Indian Journal of Pediatrics, 79(9), 1169–1175. https://doi.org/10.1007/s12098-011-0674-8.
Rodríguez Martínez, C., & Sossa, M. P. (2005). Validation of an asthma knowledge questionnaire for use in parents or guardians of children with asthma. Archivos de Bronconeumologia, 41(8), 419–424. https://doi.org/10.1157/13077952.
Saini, B., LeMay, K., Emmerton, L., Krass, I., Smith, L., Bosnic-Anticevich, S., … Armour, C. (2011). Asthma disease management-Australian pharmacists’ interventions improve patients’ asthma knowledge and this is sustained. Patient Education and Counseling, 83(3), 295–302. https://doi.org/10.1016/j.pec.2011.05.001.
Brodzinsky, D. M., Elias, M. J., Steiger, C., Simon, J., Gill, M., & Hitt, J. C. (1992). Coping scale for children and youth: Scale development and validation. Journal of Applied Developmental Psychology, 13(2), 195–214. https://doi.org/10.1016/0193-3973(92)90029-H.
Ekim, A., & Ocakci, A. F. (2013). Perceptions of parents and children regarding asthma management responsibilities. Journal for Specialists in Pediatric Nursing, 18(4), 289–296. https://doi.org/10.1111/jspn.12037.
Bruzzese, J. M., Reigada, L. C., Lamm, A., Wang, J., Li, M., Zandieh, S. O., & Klein, R. G. (2016). Association of youth and caregiver anxiety and Asthma care among urban young adolescents. Academic Pediatrics, 16(8), 792–798. https://doi.org/10.1016/j.acap.2016.03.009.
Murillo, M., Bel, J., Pérez, J., Corripio, R., Carreras, G., Herrero, X., … Rajmil, L. (2017). Health-related quality of life (HRQOL) and its associated factors in children with Type 1 Diabetes Mellitus (T1DM). BMC Pediatrics, 10, 2–9. https://doi.org/10.1186/s12887-017-0788-x.
Mayoral, K., Rajmil, L., Murillo, M., Garin, O., Pont, A., Alonso, J., … Ferrer, M. (2019). Measurement Properties of the Online EuroQol-5D-Youth Instrument in Children and Adolescents With Type 1 Diabetes Mellitus: Questionnaire Study. Journal of medical Internet research, 21(11), 14947.https://doi.org/10.2196/14947.
Haute Autorité de Santé - Good practice guidelines on health apps and smart devices (mobile health or mhealth). (2016). Retrieved February 27, 2020, from https://www.has-sante.fr/jcms/c_2681915/en/good-practice-guidelines-on-health-apps-and-smart-devices-mobile-health-or-mhealth.
Kaufman, J. (2016). Apteligent Principles of Mobile App Design. Retrieved February 27, 2020, from https://www.apteligent.com/wp-content/uploads/2016/07/PRINCIPLES-MOBILE-APP-DESIGN-WP.pdf.
Themes—iOS—Human Interface Guidelines—Apple Developer. (n.d.). Retrieved March 2, 2020, from https://developer.apple.com/design/human-interface-guidelines/ios/overview/themes/.
International Standard ISO 9241-11. (1998). Retrieved October 28, 2019, from https://www.sis.se/api/document/preview/611299/.
Lewis, J. R., & Sauro, J. (2009). The factor structure of the system usability scale. Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics), 5619 LNCS (pp. 94–103). Berlin: Springer. https://doi.org/10.1007/978-3-642-02806-9_12.
Bangor, A., Kortum, P. T., & Miller, J. T. (2008). An empirical evaluation of the system usability scale. International Journal of Human-Computer Interaction, 24(6), 574–594. https://doi.org/10.1080/10447310802205776.
Rudin, R. S., Fanta, C. H., Qureshi, N., Duffy, E., Edelen, M. O., Dalal, A. K., & Bates, D. W. (2019). A clinically integrated mHealth app and practice model for collecting patient-reported outcomes between visits for Asthma patients: Implementation and feasibility. Applied Clinical Informatics, 10(5), 783–793. https://doi.org/10.1055/s-0039-1697597.
Odom, L., & Christenbery, T. (2016). There is an “app” for that: Designing mobile phone technology to improve asthma action plan use in adolescent patients. Journal of the American Association of Nurse Practitioners, 28(11), 583–590. https://doi.org/10.1002/2327-6924.12375.
Wang, J., Wang, Y., Wei, C., Yao, N., Yuan, A., Shan, Y., & Yuan, C. (2014). Smartphone interventions for long-term health management of chronic diseases: An integrative review. Telemedicine and e-Health, 20(6), 570–583. https://doi.org/10.1089/tmj.2013.0243.
Lydick, E., & Epstein, R. S. (1993). Interpretation of quality of life changes. Quality of Life Research, 2(3), 221–226. https://doi.org/10.1007/BF00435226.
Marquis, P., Chassany, O., & Abetz, L. (2004). A comprehensive strategy for the interpretation of quality-of-life data based on existing methods. Value in Health, 7(1), 93–104. https://doi.org/10.1111/j.1524-4733.2004.71217.x.
Rudin, R. S., Fanta, C. H., Predmore, Z., Kron, K., Edelen, M. O., Landman, A. B., … Bates, D. W. (2017). Core components for a clinically integrated mHealth app for asthma symptom monitoring. Applied Clinical Informatics, 8(4), 1031–1043. https://doi.org/10.4338/ACI-2017-06-RA-0096.
Kim, J. H., Kwon, S. S., Shim, S. R., Sun, H. Y., Ko, Y. M., Chun, D. Il, … Song, Y. S. (2014). Validation and reliability of a smartphone application for the international prostate symptom score questionnaire: A randomized repeated measures crossover study. Journal of Medical Internet Research, 16(2), 1–13. https://doi.org/10.2196/jmir.3042.
Zhang, S., Wu, Q., Van Velthoven, M. H. M. M. T., Chen, L., Car, J., Rudan, I., … Scherpbier, R. W. (2012). Smartphone versus pen-and-paper data collection of infant feeding practices in rural China. Journal of Medical Internet Research, 14(5), 1–13. https://doi.org/10.2196/jmir.2183.
Chan, Y. F. Y., Bot, B. M., Zweig, M., Tignor, N., Ma, W., Suver, C., … Wang, P. (2018). Data Descriptor: The asthma mobile health study, smartphone data collected using ResearchKit. Scientific Data, 5, 1–11. https://doi.org/10.1038/sdata.2018.96.
Rasmussen, L. M., Phanareth, K., Nolte, H., & Backer, V. (2005). Internet-based monitoring of asthma: A long-term, randomized clinical study of 300 asthmatic subjects. Journal of Allergy and Clinical Immunology, 115(6), 1137–1142. https://doi.org/10.1016/j.jaci.2005.03.030.
Wisniewski, J. A., McLaughlin, A. P., Stenger, P. J., Patrie, J., Brown, M. A., El-Dahr, J. M., … Heymann, P. W. (2016). A comparison of seasonal trends in asthma exacerbations among children from geographic regions with different climates. Allergy and Asthma Proceedings, 37(6), 475–481. https://doi.org/10.2500/aap.2016.37.3994.
Bantug, E. T., Coles, T., Smith, K. C., Snyder, C. F., Rouette, J., & Brundage, M. D. (2016). Graphical displays of patient-reported outcomes (PRO) for use in clinical practice: What makes a pro picture worth a thousand words? Patient Education and Counseling, 99(4), 483–490. https://doi.org/10.1016/j.pec.2015.10.027.
Instituto Nacional de Estadística. Encuesta sobre Equipamiento y Uso de Tecnologías de Información y Comunicación en los Hogares, Año 2019. (n.d.). Retrieved January 28, 2020, from https://www.ine.es/prensa/tich_2019.pdf.
La Biblioteca Pública ante la brecha digital: Oportunidades y retos. (2005). Bibliotecas y nuevas tegnologías. Retrieved October 22, 2020, from https://gredos.usal.es/handle/10366/119981.
Acknowledgements
The authors would like to acknowledge the technical group “STARTCAT APP DEVELOPMENT, S.L.” in charge of the development of the mobile application ARCA, and Aurea Martin for her contributions in discussing on digital divide in Spain with the authors, helping in the English editing, proofreading process, figure creation, and translation, and finalizing this manuscript.
ARCA Group
Montse Ferrer, Yolanda Pardo, Àngels Pont, Olatz Garin, Karina Mayoral, Catalina Lizano, Víctor Zamora (IMIM, Institut Hospital del Mar d’Investigacions Mèdiques); Maria Araceli Caballero, Sara Calpe (Pediatric service. Hospital del Mar); Gimena Hernandez (CAP Vila Olimpica); Manuel Praena (Centro de Salud la Candelaria); Alberto Bercedo (Centro de Salud Dobra); Jose Antonio Castillo (Hospital Infantil Universitario Miguel Servet); Olga Cortés (Centro de Salud Canillejas); Isabel Moneo (Centro de Salud Torre Ramona); Ines de Mir (Hospital Vall d’Hebron); Laura Valdesoiro (Parc Taulí Hospital Universitario); Pilar Ortiz (Centro de Salud Dos de Mayo); María Ángeles Carrasco (Centro de Salud Villa del Prado); Alexandra L. Dima, Eric van Ganse (University Claude Bernard Lyon), Marijn de Bruin (Radboud University Medical Center, Radboud Institute for Health Sciences, IQ Healthcare).
Funding
Financial support for this study was provided through grants by the Instituto de Salud Carlos III FEDER: Fondo Europeo de Desarrollo Regional (PI15/00449 and FI16/00071), University of Costa Rica (OAICE-85-2019), and Generalitat de Catalunya (2017 SGR 452). The funding agreements ensure the authors’ independence in designing the study, interpreting the data, and writing and publishing the report.
Author information
Authors and Affiliations
Consortia
Contributions
KM contributed to the conception and design of the article and wrote the article; OG contributed to the conception and design of the article, M-AC, MP, AB, GH, and JC participated in the design of the study and carried out the fieldwork; CL and YP revised important intellectual content and the draft versions of the manuscript; and MF oversaw all aspects, conceived the study, contributed to the conception and design of the article, and contributed to the writing of the article. All the co-authors critically revised the manuscript and approved the final draft before submission and can attest to the validity and legitimacy of the data in the manuscript and agree to be named as author of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Ethical approval
The study has the approval of the Parc de Salut Mar ethical committee of clinical research (nº 2015/62/12l), and it was conducted in accordance with the ethical standards of the institutional research committee and the 2000 revision of the Declaration of Helsinki. Informed consent was obtained from the parents or legally authorized representatives of participants, as well as from the children or adolescents.
Transparency
The lead authors (KM and MF) affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of ARCA group were included in acknowledgements section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mayoral, K., Garin, O., Caballero-Rabasco, M.A. et al. Smartphone App for monitoring Asthma in children and adolescents. Qual Life Res 30, 3127–3144 (2021). https://doi.org/10.1007/s11136-020-02706-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02706-z