Abstract
Purpose
Collecting patient-reported outcomes is important in informing the well-being of women with breast cancer. Consumer perceptions are important for successful implementation of monitoring systems, but are rarely formally assessed. We compared reactions to two different surveys (assessing psychosocial outcomes and/or Health-related Quality of Life (HrQoL) outcomes) among Australian women with breast cancer.
Methods
Women (18 + years) within 5 years diagnosis of breast cancer were randomly allocated to complete one of two online surveys: (i) minimum HrQoL measures or (ii) minimum HrQoL measures plus psychosocial outcomes (body image, depression, anxiety stress, fear of cancer recurrence, decisional difficulties and unmet need). Participants completed questions regarding their perceptions of the survey, including qualitative feedback.
Results
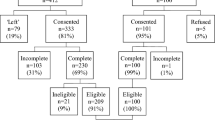
Data were available for 171 participants (n(i) = 89; n(ii) = 82), with 92% (n = 158) providing 95–100% complete data. Perceptions were comparable between survey groups, and high (80–100%) regarding time burden, ease of completion, comprehensible, appropriateness and willingness to participate again and moderately high (67–74%) regarding willingness to answer more questions and relevance. Qualitative feedback indicated gaps across both surveys, including financial/work-related issues, satisfaction with information and care, need for nuanced questions, and impact of side effects/treatment, and from the minimum set only, emotional well-being and support. Impairment in some HrQoL and psychosocial outcomes were observed among participants.
Conclusions
Assessment of HrQoL and psychosocial outcomes was well received by consumers. Results alleviate concern regarding possible patient burden imposed by longer more in-depth surveys. The importance placed on assessment brevity should not outweigh the need to assess outcomes that consumers consider important.
Similar content being viewed by others
Data availability
The data may be available from the authors on reasonable request and with appropriate ethical approval/clearance.
References
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6), 394–424. https://doi.org/10.3322/caac.21492.
Australian Institute of Health and Welfare. (2017). Cancer in Australia. Cancer series no 101. Cat. no. 100. Canberra: AIHW.
Australian Institute of Health and Welfare. (2016). BreastScreen Australia monitoring report 2013–2014. Cancer series no. 100. Cat. no. CAN 99. Canberra: AIHW.
Ong, W. L., Schouwenburg, M. G., van Bommel, A. C. M., Stowell, C., Allison, K. H., Benn, K. E., et al. (2017). A standard set of value-based patient-centered outcomes for breast cancer: The international consortium for health outcomes measurement (ICHOM) initiative. JAMA Oncology, 3(5), 677–685. https://doi.org/10.1001/jamaoncol.2016.4851.
Australian Institute of Health and Welfare. (2012). Breast cancer in Australia: an overview. Cat. no. 71. Canberra: Australian Institute of Health and Welfare.
Hu, K., Ding, P., Wu, Y., Tian, W., Pan, T., & Zhang, S. (2019). Global patterns and trends in the breast cancer incidence and mortality according to sociodemographic indices: An observational study based on the global burden of diseases. British Medical Journal Open, 9(10), e028461. https://doi.org/10.1136/bmjopen-2018-028461.
Bloom, J. R., & Kessler, L. (1994). Emotional support following cancer: A test of the stigma and social activity hypotheses. Journal of Health and Social Behavior, 35(2), 118–133.
Burgess, C., Cornelius, V., Love, S., Graham, J., Richards, M., & Ramirez, A. (2005). Depression and anxiety in women with early breast cancer: Five year observational cohort study. BMJ, 330(7493), 702. https://doi.org/10.1136/bmj.38343.670868.D3.
Przezdziecki, A., Sherman, K. A., Baillie, A., Taylor, A., Foley, E., & Stalgis-Bilinski, K. (2013). My changed body: Breast cancer, body image, distress and self-compassion. Psycho-Oncology, 22(8), 1872–1879. https://doi.org/10.1002/pon.3230.
Montazeri, A. (2008). Health-related quality of life in breast cancer patients: A bibliographic review of the literature from 1974 to 2007. Journal of Experimental and Clinical Cancer Research, 27(1), 32. https://doi.org/10.1186/1756-9966-27-32.
Sharma, N., & Purkayastha, A. (2017). Factors affecting quality of life in breast cancer patients: A descriptive and cross-sectional study with review of literature. Journal of Mid-life Health, 8(2), 75. https://doi.org/10.4103/jmh.JMH_15_17.
Mayo, N. (2015). Dictionary of quality of life and health outcomes measurement. Milwaukee: International Society for Quality of Life Research.
Bloom, J. R., Stewart, S. L., Chang, S., & Banks, P. J. (2004). Then and now: Quality of life of young breast cancer survivors. Psycho-Oncology, 13(3), 147–160. https://doi.org/10.1002/pon.794.
Fitzpatrick, T. R., Edgar, L., & Holcroft, C. (2012). Assessing the relationship between physical fitness activities, cognitive health, and quality of life among older cancer survivors. Journal of Psychosocial Oncology, 30(5), 556–572. https://doi.org/10.1080/07347332.2012.703768.
Mitchell, A. J., Chan, M., Bhatti, H., Halton, M., Grassi, L., Johansen, C., et al. (2011). Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncology, 12(2), 160–174. https://doi.org/10.1016/S1470-2045(11)70002-X.
Lagendijk, M., van Egdom, L. S. E., van Veen, F. E. E., Vos, E., Mureau, M., van Leeuwen, N., et al. (2018). Patient-reported outcome measures may add value in breast cancer surgery. Annals of Surgical Oncology, 25(12), 3563–3571. https://doi.org/10.1245/s10434-018-6729-6.
Lagendijk, M., van Egdom, L. S. E., Richel, C., van Leeuwen, N., Verhoef, C., Lingsma, H. F., et al. (2018). Patient reported outcome measures in breast cancer patients. European Journal of Surgical Oncology, 44(7), 963–968. https://doi.org/10.1016/j.ejso.2018.03.009.
Kool, M., van der Sijp, J. R. M., Kroep, J. R., Liefers, G.-J., Jannink, I., Guicherit, O. R., et al. (2016). Importance of patient reported outcome measures versus clinical outcomes for breast cancer patients evaluation on quality of care. The Breast, 27, 62–68. https://doi.org/10.1016/j.breast.2016.02.015.
Sugrue, R., Macgregor, G., Sugrue, M., Curran, S., & Murphy, L. (2013). An evaluation of patient reported outcomes following breast reconstruction utilizing Breast Q. The Breast, 22(2), 158–161. https://doi.org/10.1016/j.breast.2012.12.001.
Ghosh, R. K., Ghosh, S. M., & Ganguly, G. (2010). Health-related quality of life and its growing importance in clinical practice. New Zealand Medical Journal, 123(1313), 99–101.
Wasson, J., Keller, A., Rubenstein, L., Hays, R., Nelson, E., Johnson, D., et al. (1992). Benefits and obstacles of health status assessment in ambulatory settings: The clinician's point of view. Medical Care, 30(5), 42–49.
Wu, A. W., Snyder, C., Clancy, C. M., & Steinwachs, D. M. (2010). Adding the patient perspective to comparative effectiveness research. Journal of Health Affairs, 29(10), 1863–1871.
Van De Poll-Franse, L. V., Horevoorts, N., Eenbergen, M. V., Denollet, J., Roukema, J. A., Aaronson, N. K., et al. (2011). The patient reported outcomes following initial treatment and long term evaluation of survivorship registry: Scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. European Journal of Cancer, 47(14), 2188–2194. https://doi.org/10.1016/j.ejca.2011.04.034.
Kelley, T. A. (2015). International consortium for health outcomes measurement (ICHOM). Trials, 16(3), O4.
Black, N. (2013). Patient reported outcome measures could help transform healthcare. BMJ, 346, f167. https://doi.org/10.1136/bmj.f167.
Hu, E. S., Pusic, A. L., Waljee, J. F., Kuhn, L., Hawley, S. T., Wilkins, E., et al. (2009). Patient-reported aesthetic satisfaction with breast reconstruction during the long-term survivorship period. Plastic and Reconstructive Surgery, 124(1), 1. https://doi.org/10.1097/PRS.0b013e3181ab10b2.
Al-Ghazal, S. K., Fallowfield, L., & Blamey, R. W. (2000). Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. European Journal of Cancer, 36(15), 1938–1943. https://doi.org/10.1016/S0959-8049(00)00197-0.
Rabin, C., Leventhal, H., & Goodin, S. (2004). Conceptualization of disease timeline predicts posttreatment distress in breast cancer patients. Health Psychology, 23(4), 407–412. https://doi.org/10.1037/0278-6133.23.4.407.
Holt, S., Bertelli, G., Humphreys, I., Valentine, W., Durrani, S., Pudney, D., et al. (2013). A decision impact, decision conflict and economic assessment of routine Oncotype DX testing of 146 women with node-negative or pNImi, ER-positive breast cancer in the UK. British Journal of Cancer, 108, 2250–2258. https://doi.org/10.1038/bjc.2013.207.
Martinez, K. A., Li, Y., Resnicow, K., Graff, J. J., Hamilton, A. S., & Hawley, S. T. (2015). Decision regret following treatment for localized breast cancer: Is regret stable over time? Medical Decision Making, 35(4), 446–457. https://doi.org/10.1177/0272989X14564432.
Bower, J. E. (2008). Behavioral symptoms in patients with breast cancer and survivors. Journal of Clinical Oncology, 26(5), 768–777. https://doi.org/10.1200/JCO.2007.14.3248.
Singh, R., Singh, H., Singh, C., & Kaur, K. (2015). Screening of psychological distress in cancer patients during chemotherapy: A cross-sectional study. Indian Journal of Palliative Care, 21(3), 305–310. https://doi.org/10.4103/0973-1075.164887.
Prepared by L&M Policy Research, & LLC under Contract No. 290–2014-00004-C. (2018). EBook addendum to registries for evaluating patient outcomes: A user’s guide. In R. E. Gliklich, N. A. Dreyer, M. B. Leavy, & J. B. Christian (Eds.), Registries for evaluating patient outcomes: A user’s guide (3rd ed.). Rockville, MD: Agency for Healthcare Research and Quality.
Wiering, B., de Boer, D., & Delnoij, D. (2017). Patient involvement in the development of patient-reported outcome measures: A scoping review. Health Expectations, 20(1), 11–23. https://doi.org/10.1111/hex.12442.
Camuso, N., Bajaj, P., Dudgeon, D., & Mitera, G. (2016). Engaging patients as partners in developing patient-reported outcome measures in cancer—A review of the literature. Supportive Care in Cancer, 24(8), 3543–3549.
Mitchell, A. J., Vahabzadeh, A., & Magruder, K. (2011). Screening for distress and depression in cancer settings: 10 lessons from 40 years of primary-care research. Psycho-Oncology, 20(6), 572–584. https://doi.org/10.1002/pon.1943.
Pobiruchin, M., Bochum, S., Martens, U. M., & Schramm, W. (2016). Clinical cancer registries—Are they up for health services research? Studies in Health Technology and Informatics, 228, 242–246.
Parkin, D. M. (2006). The evolution of the population-based cancer registry. Nature Reviews: Cancer, 6, 603. https://doi.org/10.1038/nrc1948.
Rajaram, N., Lim, Z. Y., Song, C. V., Kaur, R., Mohd Taib, N. A., Muhamad, M., et al. (2019). Patient-reported outcome measures among breast cancer survivors: A cross-sectional comparison between Malaysia and high-income countries. Psycho-Oncology, 28(1), 147–153. https://doi.org/10.1002/pon.4924.
Oh, D. D., Flitcroft, K., Brennan, M. E., Snook, K. L., & Spillane, A. J. (2018). Patient-reported outcomes of breast reconstruction in older women: Audit of a large metropolitan public/private practice in Sydney, Australia. Psycho-Oncology, 27(12), 2815–2822. https://doi.org/10.1002/pon.4895.
Qualtrics. (2018). Provo. Utah: Qualtrics.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101.
Harrison Health Research. (2012). The health omnibus survey spring 2012. Adelaide: Harrison Health Research.
Australian Bureau of Statistics (2018). Methods, Classifications, Concepts & Standards. Retrieved February, 2019 from https://www.abs.gov.au/websitedbs/D3310114.nsf/home/Basic+Survey+Design+-+Introduction.
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., et al. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365–376. https://doi.org/10.1093/jnci/85.5.365.
McLachlan, S. A., Devins, G. M., & Goodwin, P. J. (1998). Validation of the European organization for research and treatment of cancer quality of life questionnaire (QLQ-C30) as a measure of psychosocial function in breast cancer patients. European Journal of Cancer, 34(4), 510–517.
Groenvold, M., Klee, M. C., Sprangers, M. A. G., & Aaronson, N. K. (1997). Validation of the EORTC QLQ-C30 quality of life questionnaire through combined qualitative and quantitative assessment of patient-observer agreement. Journal of Clinical Epidemiology, 50(4), 441–450. https://doi.org/10.1016/S0895-4356(96)00428-3.
Charalambous, A., Kaite, C. P., Charalambous, M., Tistsi, T., & Kouta, C. (2017). The effects on anxiety and quality of life of breast cancer patients following completion of the first cycle of chemotherapy. SAGE Open Medicine, 5, 1–10. https://doi.org/10.1177/2050312117717507.
Aranda, S., Schofield, P., Weih, L., Yates, P., Milne, D., Faulkner, R., et al. (2005). Mapping the quality of life and unmet needs of urban women with metastatic breast cancer. European Journal of Cancer Care, 14(3), 211–222. https://doi.org/10.1111/j.1365-2354.2005.00541.x.
Sprangers, M. A., Groenvold, M., Arraras, J. I., Franklin, J., te Velde, A., Muller, M., et al. (1996). The European organization for research and treatment of cancer breast cancer-specific quality-of-life questionnaire module: First results from a three-country field study. Journal of Clinical Oncology, 14(10), 2756–2768. https://doi.org/10.1200/JCO.1996.14.10.2756.
Tan, M. L., Idris, D. B., Teo, L. W., Loh, S. Y., Seow, G. C., Chia, Y. Y., et al. (2014). Validation of EORTC QLQ-C30 and QLQ-BR23 questionnaires in the measurement of quality of life of breast cancer patients in Singapore. Asia-Pacific Journal of Oncology Nursing, 1(1), 22–32. https://doi.org/10.4103/2347-5625.135817.
Nguyen, J., Popovic, M., Chow, E., Cella, D., Beaumont, J. L., Chu, D., et al. (2015). EORTC QLQ-BR23 and FACT-B for the assessment of quality of life in patients with breast cancer: A literature review. Journal of Comparative Effectiveness Research, 4, 157–166.
Fallowfield, L. J., Leaity, S. K., Howell, A., Benson, S., & Cella, D. (1999). Assessment of quality of life in women undergoing hormonal therapy for breast cancer: Validation of an endocrine symptom subscale for the FACT-B. Breast Cancer Research and Treatment, 55(2), 189.
Hickey, M., Marino, J. L., Braat, S., & Wong, S. (2016). A randomized, double-blind, crossover trial comparing a silicone-versus water-based lubricant for sexual discomfort after breast cancer. Breast Cancer Research and Treatment, 158(1), 79–90. https://doi.org/10.1007/s10549-016-3865-1.
Marino, J. L., Saunders, C. M., Emery, L. I., Green, H., Doherty, D. A., & Hickey, M. (2013). Nature and severity of menopausal symptoms and their impact on quality of life and sexual function in cancer survivors compared with women without a cancer history. Menopause. https://doi.org/10.1097/GME.0b013e3182976f46.
Kavadas, V., Blazeby, J. M., Conroy, T., Sezer, O., Holzner, B., Koller, M., et al. (2003). Development of an EORTC disease-specific quality of life questionnaire for use in patients with liver metastases from colorectal cancer. European Journal of Cancer, 39(9), 1259–1263. https://doi.org/10.1016/S0959-8049(03)00236-3.
Pusic, A. L., Klassen, A. F., Scott, A. M., Klok, J. A., Cordeiro, P. G., & Cano, S. J. (2009). Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plastic and Reconstructive Surgery, 124(2), 345. https://doi.org/10.1097/PRS.0b013e3181aee807.
Liu, L. Q., Branford, O. A., & Mehigan, S. (2018). BREAST-Q measurement of the patient perspective in oncoplastic breast surgery: A systematic review. Plastic and Reconstructive Surgery Global Open, 6(8), e1904. https://doi.org/10.1097/gox.0000000000001904.
Hopwood, P., Fletcher, I., Lee, A., & Al Ghazal, S. (2001). A body image scale for use with cancer patients. European Journal of Cancer, 37(2), 189–197.
Muzzatti, B., & Annunziata, M. (2017). Body image assessment in oncology: An update review. Supportive Care in Cancer, 25(3), 1019–1029. https://doi.org/10.1007/s00520-016-3538-y.
Tylka, T. L., & Wood-Barcalow, N. L. (2015). The body appreciation scale-2: Item refinement and psychometric evaluation. Body Image, 12(1), 53–67. https://doi.org/10.1016/j.bodyim.2014.09.006.
Alleva, J. M., Tylka, T. L., & Kroon Van Diest, A. M. (2017). The functionality appreciation scale (FAS): Development and psychometric evaluation in U.S. community women and men. Body Image, 23, 28–44. https://doi.org/10.1016/j.bodyim.2017.07.008.
Lerman, C., Daly, M., Masny, A., & Balshem, A. (1994). Attitudes about genetic testing for breast-ovarian cancer susceptibility. Journal of Clinical Oncology, 12(4), 843–850. https://doi.org/10.1200/JCO.1994.12.4.843.
O'Connor, A. M. (1995). Validation of a decisional conflict scale. Medical Decision Making, 15(1), 25–30. https://doi.org/10.1177/0272989X9501500105.
Kim, S., Lee, Y., Son, Y., Jun, S., Yun, S., Bae, H., et al. (2015). Assessment of breast cancer patients' knowledge and decisional conflict regarding Tamoxifen use. Journal of Korean Medical Science, 30(11), 1604–1610. https://doi.org/10.3346/jkms.2015.30.11.1604.
Brehaut, J. C., O'Connor, A. M., Wood, T. J., Hack, T. F., Siminoff, L., Gordon, E., et al. (2003). Validation of a decision regret scale. Medical Decision Making, 23(4), 281–292. https://doi.org/10.1177/0272989x03256005.
Vickers, A. J. (2017). Decisional conflict, regret, and the burden of rational decision making. Medical Decision Making, 37(1), 3–5. https://doi.org/10.1177/0272989X16657544.
Wang, A. W.-T., Chang, S.-M., Chang, C.-S., Chen, S.-T., Chen, D.-R., Fan, F., et al. (2018). Regret about surgical decisions among early-stage breast cancer patients: Effects of the congruence between patients' preferred and actual decision-making roles. Psycho-Oncology, 27(2), 508–514. https://doi.org/10.1002/pon.4522.
Lovibond, S. H. (1995). Manual for the depression anxiety stress scales. In P. F. Lovibond (Ed.), Manual for the DASS (2nd ed.). Sydney: Psychology Foundation of Australia.
Bener, A., Alsulaiman, R., Lg, D., & Ayoubi Hr, E. (2016). Comparison of reliability and validity of the breast cancer depression anxiety stress scales (DASS-21) with the beck depression inventory-(BDI-II) and Hospital Anxiety and Depression Scale (HADS). International Journal of Behavioral Research & Psychology, 4(4), 197–203. https://doi.org/10.19070/2332-3000-1600035.
Bastien, C., Vallieres, A., & Morin, C. (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2001(2), 297–307.
Reinsel, R., Starr, T., O'Sullivan, B., Passik, S. D., & Kavey, N. (2015). Polysomnographic study of sleep in survivors of breast cancer. Journal of Clinical Sleep Medicine, 11(12), 1361–1370. https://doi.org/10.5664/jcsm.5264.
Savard, J., Ivers, H., Savard, M.-H., & Morin, C. M. (2014). Is a video-based cognitive behavioral therapy for insomnia as efficacious as a professionally administered treatment in breast cancer? Results of a randomized controlled trial. Sleep, 37(8), 1305. https://doi.org/10.5665/sleep.3918.
Desai, K., Mao, J., Su, I., DeMichele, A., Li, Q., Xie, S., et al. (2013). Prevalence and risk factors for insomnia among breast cancer patients on aromatase inhibitors. Supportive Care in Cancer, 21(1), 43–51. https://doi.org/10.1007/s00520-012-1490-z.
Girgis, A., Stojanovski, E., Boyes, A., King, M., & Lecathelinais, C. (2012). The next generation of the supportive care needs survey: A brief screening tool for administration in the clinical oncology setting. Psycho-Oncology, 21(8), 827–835. https://doi.org/10.1002/pon.1973.
Renovanz, M., Hickmann, A.-K., Coburger, J., Kohlmann, K., Janko, M., Reuter, A. K., et al. (2016). Assessing psychological and supportive care needs in glioma patients—Feasibility study on the use of the supportive care needs survey short form (SCNS-SF34-G) and the supportive care needs survey screening tool (SCNS-ST9) in clinical practice. European Journal of Cancer Care, 27(1), e12598. https://doi.org/10.1111/ecc.12598.
Girgis, A., Durcinoska, I., Levesque, J. V., Gerges, M., Sandell, T., Arnold, A., et al. (2017). eHealth system for collecting and utilizing patient reported outcome measures for personalized treatment and care (PROMPT-Care) among cancer patients: Mixed methods approach to evaluate feasibility and acceptability. Journal of Medical Internet Research, 19(10), e330. https://doi.org/10.2196/jmir.8360.
Australian Institute of Health and Welfare. (2018). Analysis of breast cancer outcomes and screening behaviour for BreastScreen Australia. (Vol. Cancer series no. 113. Cat. no. CAN 118). Canberra: AIHW.
Howes, B. H. L., Watson, D. I., Xu, C., Fosh, B., Canepa, M., & Dean, N. R. (2016). Quality of life following total mastectomy with and without reconstruction versus breast-conserving surgery for breast cancer: A case-controlled cohort study. Journal of Plastic, Reconstructive & Aesthetic Surgery, 69(9), 1184–1191. https://doi.org/10.1016/j.bjps.2016.06.004.
Bidstrup, P. E., Christensen, J., Mertz, B. G., Rottmann, N., Dalton, S. O., & Johansen, C. (2015). Trajectories of distress, anxiety, and depression among women with breast cancer: Looking beyond the mean. Acta Oncologica, 54(5), 789–796. https://doi.org/10.3109/0284186X.2014.1002571.
Corsini, N., Fish, J., Ramsey, I., Sharplin, G., Flight, I., Damarell, R., et al. (2017). Cancer survivorship monitoring systems for the collection of patient-reported outcomes: A systematic narrative review of international approaches. Journal of Cancer Survivorship, 11(4), 486–497. https://doi.org/10.1007/s11764-017-0607-2.
Chan, R. J., Gordon, L. G., Tan, C. J., Chan, A., Bradford, N. K., Yates, P., et al. (2019). Relationships between financial toxicity and symptom burden in cancer survivors: A systematic review. Journal of Pain and Symptom Management, 57(3), 646–660.e641. https://doi.org/10.1016/j.jpainsymman.2018.12.003.
Gordon, L. G., Merollini, K. M. D., Lowe, A., & Chan, R. J. (2017). A systematic review of financial toxicity among cancer survivors: We can’t pay the co-pay. The Patient Patient-Centred Outcomes Research, 10(3), 295–309. https://doi.org/10.1007/s40271-016-0204-x.
De Souza, J. A., Yap, B. J., Hlubocky, F. J., Wroblewski, K., Ratain, M. J., Cella, D., et al. (2014). The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer, 120(20), 3245–3253. https://doi.org/10.1002/cncr.28814.
Boyes, A., Girgis, A., & Lecathelinais, C. (2009). Brief assessment of adult cancer patients' perceived needs: Development and validation of the 34-item Supportive Care Needs Survey (SCNS-SF34). Journal of Evaluation in Clinical Practice, 15(4), 602–606. https://doi.org/10.1111/j.1365-2753.2008.01057.x.
Lee, T. S., Kilbreath, S. L., Refshauge, K. M., Pendlebury, S. C., Beith, J. M., & Lee, M. J. (2008). Quality of life of women treated with radiotherapy for breast cancer. Supportive Care in Cancer, 16(4), 399–405. https://doi.org/10.1007/s00520-007-0328-6.
Active internet users as a percentage of the total population in Australia 2015 to 2018. (2018). Retrieved April 14, 2020 from https://www.statista.com/statistics/680142/australia-internet-penetration/.
Perry, S., Kowalski, T. L., & Chang, C. H. (2007). Quality of life assessment in women with breast cancer: Benefits, acceptability and utilization. Health and Quality of Life Outcomes, 5, 24. https://doi.org/10.1186/1477-7525-5-24.
Acknowledgements
We acknowledge the contribution of all of the women who participated in this research, including those from Breast Cancer Network Australia's (BCNA) Review and Survey group, a national online group of Australian women living with breast cancer who are interested in receiving invitations to participate in research.
Funding
This work was supported by a grant from the National Breast Cancer Foundation. The funders had no role in study design, collection, analysis and interpretation of data, in the writing of the report or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
KE conceptualised and led the study with substantial contributions from IP, KGS, KW, CM and DR. JC and KGS undertook data cleaning and scoring, and KE conducted analyses and drafted the paper. All the authors reviewed drafts and contributed to interpretation of the results.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the University of Adelaide Human Research Ethics Committee (H-2018–072).
Consent to participate
Participants were informed that completing the online survey was considered providing consent.
Consent for publication
Participants were informed of all potential use(s) of the data, including publication prior to providing consent to participate in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ettridge, K., Caruso, J., Roder, D. et al. A randomised online experimental study to compare responses to brief and extended surveys of health-related quality of life and psychosocial outcomes among women with breast cancer. Qual Life Res 30, 407–423 (2021). https://doi.org/10.1007/s11136-020-02651-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02651-x