Abstract
Purpose
To explore the relationship between sociodemographic and lifestyle variables with health-related quality of life (HRQoL) of a large cohort of ‘healthy’ older individuals.
Methods
The sample included individuals aged 65+ years from Australia (N = 16,703) and the USA (N = 2411) enrolled in the ASPirin in Reducing Events in the Elderly (ASPREE) multicentre placebo-controlled trial study and free of cardiovascular disease, dementia, serious physical disabilities or ‘fatal’ illnesses. The associations with the physical (PCS) and mental component scores (MCS) of HRQoL (SF-12 questionnaire) were explored using multiple linear regression models from data collected at baseline (2010–2014).
Results
The adjusted PCS mean was slightly higher in the USA (49.5 ± 9.1) than Australia (48.2 ± 11.6; p < 0.001), but MCS was similar in both samples (55.7 ± 7.5 and 55.7 ± 9.6, respectively; p = 0.603). Males, younger participants, better educated, more active individuals, or those currently drinking 1–2 alcoholic drinks/day showed a better HRQoL (results more evident for PCS than MCS), while current heavy smokers had the lowest physical HRQoL in both countries. Neither age, walking time, nor alcohol intake was associated with MCS in either cohort.
Conclusions
Baseline HRQoL of ASPREE participants was higher than that reported in population-based studies of older individuals, but the associations between sociodemographic and lifestyle variables were consistent with the published literature. As the cohort ages and develops chronic diseases, ASPREE will be able to document HRQoL changes.

Similar content being viewed by others
References
Salomon, J. A., Wang, H., Freeman, M. K., Vos, T., Flaxman, A. D., Lopez, A. D., & Murray, C. J. L. (2012). Healthy life expectancy for 187 countries, 1990–2010: A systematic analysis for the Global Burden Disease Study 2010. The Lancet, 380(9859), 2144–2162.
Banham, D., Hawthorne, G., Goldney, R., & Ratcliffe, J. (2014). Health-Related Quality of Life (HRQoL) changes in South Australia: Comparison of burden of disease morbidity and survey-based health utility estimates. Health and Quality of Life Outcomes, 12(1), 113.
World Health Organization. (2015). World report on ageing and health. Geneva: World Health Organization. Accessed March 1, 2017, from http://www.who.int/ageing/publications/world-report-2015/en/.
Gonzalez-Chica, D. A., Grande, D., Bowden, E., Musker, J., Hay, M., P., & Stocks, N. (2017). Are we reducing the risk of cardiovascular disease and improving the quality of life through preventive health care? Results of a population-based study in South Australia. PrevMed, 99, 164–170.
Gandek, B., Ware, J. E., Aaronson, N. K., Apolone, G., Bjorner, J. B., Brazier, J. E., Bullinger, M., Kaasa, S., Leplege, A., Prieto, L., & Sullivan, M. (1998). Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. The Journal of Clinical Epidemiology, 51(11), 1171–1178.
Frieling, M. A., Davis, W. R., & Chiang, G. (2013). The SF-36v2 and SF-12v2 health surveys in New Zealand: Norms, scoring coefficients and cross-country comparisons. Australian and New Zealand Journal of Public Health, 37(1), 24–31.
Fryback, D. G., Dunham, N. C., Palta, M., Hanmer, J., Buechner, J., Cherepanov, D., Herrington, S. A., Hays, R. D., Kaplan, R. M., Ganiats, T. G., Feeny, D., & Kind, P. (2007). US norms for six generic health-related quality-of-life indexes from the National Health Measurement Study. Medical Care, 45(12), 1162–1170.
Norman, R., Church, J., van den Berg, B., & Goodall, S. (2013). Australian health-related quality of life population norms derived from the SF-6D. Australian and New Zealand Journal of Public Health, 37(1), 17–23.
Gonzalez-Chica, D. A., Adams, R., Dal Grande, E., Avery, J., Hay, P., & Stocks, N. (2017). Lower educational level and unemployment increase the impact of cardiometabolic conditions on the quality of life: Results of a population-based study in South Australia. Quality of Life Research, 26(6), 1521–1530.
Ludt, S., Wensing, M., Szecsenyi, J., van Lieshout, J., Rochon, J., Freund, T., Campbell, S. M., & Ose, D. (2011). Predictors of health-related quality of life in patients at risk for cardiovascular disease in European primary care. PLoS ONE, 6(12), e29334.
Maatouk, I., Wild, B., Herzog, W., Wesche, D., Schellberg, D., Schottker, B., Muller, H., Rothenbacher, D., Stegmaier, C., & Brenner, H. (2012). Longitudinal predictors of health-related quality of life in middle-aged and older adults with hypertension: Results of a population-based study. Journal of Hypertension, 30(7), 1364–1372.
Milte, C. M., Thorpe, M. G., Crawford, D., Ball, K., & McNaughton, S. A. (2015). Associations of diet quality with health-related quality of life in older Australian men and women. Experimental Gerontology, 64, 8–16.
Perales, F., del Pozo-Cruz, J., del Pozo-Cruz, J., & del Pozo-Cruz, B. (2014). On the associations between physical activity and quality of life: Findings from an Australian nationally representative panel survey. Quality of Life Research, 23(7), 1921–1933.
Rosenkranz, R. R., Duncan, M. J., Rosenkranz, S. K., & Kolt, G. S. (2013). Active lifestyles related to excellent self-rated health and quality of life: Cross sectional findings from 194,545 participants in The 45 and Up Study. BMC Public Health, 13(1), 1071.
Chen, G., Iezzi, A., McKie, J., Khan, M. A., & Richardson, J. (2015). Diabetes and quality of life: Comparing results from utility instruments and Diabetes-39. Diabetes Research and Clinical Practice, 109(2), 326–333.
Tapp, R. J., Dunstan, D. W., Phillips, P., Tonkin, A., Zimmet, P. Z., & Shaw, J. E. (2006). Association between impaired glucose metabolism and quality of life: Results from the Australian diabetes obesity and lifestyle study. Diabetes Research and Clinical Practice, 74(2), 154–161.
Naliboff, B. D., Kim, S. E., Bolus, R., Bernstein, C. N., Mayer, E. A., & Chang, L. (2012). Gastrointestinal and psychological mediators of health-related quality of life in IBS and IBD: A structural equation modeling analysis. The American Journal of Gastroenterology, 107(3), 451–459.
Cleland, J., Lee, A., & Hall, S. (2007). Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Family Practice, 24, 217–223.
van der Zee-Neuen, A., Putrik, P., Ramiro, S., Keszei, A., de Bie, R., Chorus, A., & Boonen, A. (2016). Impact of chronic diseases and multimorbidity on health and health care costs: The additional role of musculoskeletal disorders. Arthritis Care & Research (Hoboken), 68(12), 1823–1831.
De Smedt, D., Clays, E., Annemans, L., Doyle, F., Kotseva, K., Pająk, A., Prugger, C., Jennings, C., Wood, D., & De Bacquer, D. (2013). Health related quality of life in coronary patients and its association with their cardiovascular risk profile: Results from the EUROASPIRE III survey. International Journal of Cardiology, 168(2), 898–903.
Gonzalez-Chica, D. A., Mnisi, Z., Avery, J., Duszynski, K., Doust, J., Tideman, P., Murphy, A., Burgess, J., Beilby, J., & Stocks, N. (2016). Effect of health literacy on quality of life amongst patients with ischaemic heart disease in Australian general practice. PLoS ONE, 11(3), e0151079.
Allen, J., Inder, K. J., Harris, M. L., Lewin, T. J., Attia, J. R., & Kelly, B. J. (2013). Quality of life impact of cardiovascular and affective conditions among older residents from urban and rural communities. Health and Quality of Life Outcomes, 11(1), 140.
O’Neil, A., Stevenson, C. E., Williams, E. D., Mortimer, D., Oldenburg, B., & Sanderson, K. (2013). The health-related quality of life burden of co-morbid cardiovascular disease and major depressive disorder in Australia: Findings from a population-based, cross-sectional study. Quality of Life Research, 22(1), 37–44.
Gonzalez-Chica, D. A., Hill, C. L., Gill, T. K., Hay, P., Haag, D., & Stocks, N. (2017). Individual diseases or clustering of health conditions? Association between multiple chronic diseases and health-related quality of life in adults. Health and Quality of Life Outcomes, 15(1), 244.
ASPREE Investigator Group. (2013). Study design of ASPirin in Reducing Events in the Elderly (ASPREE): A randomized, controlled trial. Contemporary Clinical Trials, 36(2), 555–564.
McNeil, J. J., Woods, R. L., Nelson, M. R., Murray, A. M., Reid, C. M., Kirpach, B., Storey, E., Shah, R. C., Wolfe, R. S., Tonkin, A. M., Newman, A. B., Williamson, J. D., Lockery, J. E., Margolis, K. L., Ernst, M. E., Abhayaratna, W. P., Stocks, N., Fitzgerald, S. M., Trevaks, R. E., Orchard, S. G., Beilin, L. J., Donnan, G. A., Gibbs, P., Johnston, C. I., & Grimm, R. H. (2017). Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. The Journals of Gerontology: Series A, 72(11), 1586–1593.
Antithrombotic Trialists, C., Baigent, C., Blackwell, L., Collins, R., Emberson, J., Godwin, J., Peto, R., Buring, J., Hennekens, C., Kearney, P., Meade, T., Patrono, C., Roncaglioni, M. C., & Zanchetti, A. (2009). Aspirin in the primary and secondary prevention of vascular disease: Collaborative meta-analysis of individual participant data from randomised trials. The Lancet, 373(9678), 1849–1860.
Berger, J. S., Roncaglioni, M. C., Avanzini, F., Pangrazzi, I., Tognoni, G., & Brown, D. L. (2006). Aspirin for the primary prevention of cardiovascular events in women and men: A sex-specific meta-analysis of randomized controlled trials. JAMA, 295(3), 306–313.
Rothwell, P. M., Price, J. F., Fowkes, F. G., Zanchetti, A., Roncaglioni, M. C., Tognoni, G., Lee, R., Belch, J. F., Wilson, M., Mehta, Z., & Meade, T. W. (2012). Short-term effects of daily aspirin on cancer incidence, mortality, and non-vascular death: Analysis of the time course of risks and benefits in 51 randomised controlled trials. The Lancet, 379(9826), 1602–1612.
Ware, J. E. J., KosinskiI, M., & Keller, S. D. (1996). A 12-item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
Australian Bureau of Statistics. (2011). Census of population and housing: Socio-Economic Indexes for Areas (SEIFA). Canberra: Australian Bureau of Statistics, Australia. Accessed March 5, 2015, from http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001.
Gandek, B., Ware, J., Aaronson, N., Apolone, G., Bjorner, J., Brazier, J., Bullinger, M., Kaasa, S., Leplege, A., Prieto, L., & Sullivan, M. (1998). Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: Results from the IQOLA Project. Journal of Clinical Epidemiology, 51, 1171–1178.
König, H.-H., Heider, D., Lehnert, T., Riedel-Heller, S. G., Angermeyer, M. C., Matschinger, H., Vilagut, G., Bruffaerts, R., Haro, J. M., de Girolamo, G., de Graaf, R., Kovess, V., & Alonso, J. (2010). Health status of the advanced elderly in six European countries: Results from a representative survey using EQ-5D and SF-12. Health and Quality of Life Outcomes, 8(1), 143.
Der-Martirosian, C., Cordasco, K. M., & Washington, D. L. (2013). Health-related quality of life and comorbidity among older women veterans in the United States. Quality of Life Research, 22(10), 2749–2756.
Avery, J., Grande, D. E., & Taylor, A. (2004). Quality of life in South Australia as measured by the SF-12 Health Status Questionnaire: Population norms for 2003: Trends from 1997 to 2003. South Australia: Department of Human Services, Population Research and Outcome Studies Unit. ISBN 0730893294. Accessed April 3, 2017, from http://www.health.adelaide.edu.au/pros/docs/reports/general/qol_quality_of_life_sf_12.pdf.
Gault, M. L., & Willems, M. E. (2013). Aging, functional capacity and eccentric exercise training. Aging Disease, 4(6), 351–363.
MacNee, W., Rabinovich, R. A., & Choudhury, G. (2014). Ageing and the border between health and disease. European Respiratory Journal, 44(5), 1332–1352.
Glisky, E. L. (2007). Changes in cognitive function in human aging. In D. R. Riddle (Ed.), Brain aging: Models, methods, and mechanisms. Boca Raton, FL: CRC Press/Taylor Francis.
Kremen, W. S., Lachman, M. E., Pruessner, J. C., Sliwinski, M., & Wilson, R. S. (2012). Mechanisms of age-related cognitive change and targets for intervention: Social interactions and stress. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 67(7), 760–765.
Mishra, G., & Schofield, M. (1998). Norms for the physical and mental health component summary scores of the SF-36 for young, middle aged and older Australian women. Qual Life Res, 7, 215–220.
Sattelmair, J., Pertman, J., Ding, E. L., Kohl, H. W., Haskell, W., & Lee, I. M. (2011). Dose response between physical activity and risk of coronary heart disease: A meta-analysis. Circulation, 124(7), 789–784.
Wolin, K. Y., Glynn, R. J., Colditz, G. A., Lee, I. M., & Kawachi, I. (2007). Long-term physical activity patterns and health-related quality of life in U.S. women. The American Journal of Preventive Medicine, 32(6), 490–499.
Orfila, F., Ferrer, M., Lamarca, R., Tebe, C., Domingo-Salvany, A., & Alonso, J. (2006). Gender differences in health-related quality of life among the elderly: The role of objective functional capacity and chronic conditions. Social Science & Medicine, 63(9), 2367–2380.
The World Bank. (2015). GINI index (World Bank estimate). Accessed April 3, 2017, from http://data.worldbank.org/indicator/SI.POV.GINI.
Schneider, E. C., Sarnak, D. O., Squires, D., Shah, A., & Doty, M. M. (2017). Mirror, Mirror 2017: International comparison reflects flaws and opportunities for better U.S. Health Care. Accessed November 10, 2017, from http://www.commonwealthfund.org/interactives/2017/july/mirror-mirror/.
Blendon, R. J., Schoen, C., DesRoches, C. M., Osborn, R., Scoles, K. L., & Zapert, K. (2002). Inequities in health care: A five-country survey. Health Affairs (Millwood), 21(3), 182–191.
Stringhini, S., Carmeli, C., Jokela, M., Avendano, M., McCrory, C., d’Errico, A., Bochud, M., Barros, H., Costa, G., Chadeau-Hyam, M., Delpierre, C., Gandini, M., Fraga, S., Goldberg, M., Giles, G. G., Lassale, C., Kenny, R. A., Kelly-Irving, M., Paccaud, F., Layte, R., Muennig, P., Marmot, M. G., Ribeiro, A. I., Severi, G., Steptoe, A., Shipley, M. J., Zins, M., Mackenbach, J. P., Vineis, P., Kivimaki, M., & for the LIFEPATH Consortium. (2018). Socioeconomic status, non-communicable disease risk factors, and walking speed in older adults: Multi-cohort population based study. BMJ, 360, k1046.
Ross, C., & Van Willigen, M. (1997). Education and the subjective quality of life. Journal of Health and Social Behavior, 38(3), 275–297.
Raggi, A., Corso, B., Minicuci, N., Quintas, R., Sattin, D., De Torres, L., Chatterji, S., Frisoni, G. B., Haro, J. M., Koskinen, S., Martinuzzi, A., Miret, M., Tobiasz-Adamczyk, B., & Leonardi, M. (2016). Determinants of quality of life in ageing populations: Results from a cross-sectional study in Finland, Poland and Spain. PLoS ONE, 11(7), e0159293.
Coste, J., Quinquis, L., D’Almeida, S., & Audureau, E. (2014). Smoking and health-related quality of life in the general population. independent relationships and large differences according to patterns and quantity of smoking and to gender. PLoS ONE, 9(3), e91562.
McClave, A. K., Dube, S. R., Strine, T. W., & Mokdad, A. H. (2009). Associations between health-related quality of life and smoking status among a large sample of U.S. adults. Preventive Medicine, 48(2), 173–179.
Wilson, D., Parsons, J., & Wakefield, M. (1999). The health-related quality-of-life of never smokers, ex-smokers, and light, moderate, and heavy smokers. Preventive Medicine, 29(3), 139–144.
Vogl, M., Wenig, C. M., Leidl, R., & Pokhrel, S. (2012). Smoking and health-related quality of life in English general population: Implications for economic evaluations. BMC Public Health, 12(1), 203.
Zale, E. L., Maisto, S. A., & Ditre, J. W. (2015). Interrelations between pain and alcohol: An integrative review. Clinical Psychology Review, 37, 57–71.
Acknowledgements
The authors thank Dr Jodie Avery for her support in the interpretation of the results and review of this manuscript. We acknowledge the dedicated and skilled staff in Australia and the USA for the conduct of the trial. The authors also are most grateful to the ASPREE participants, who so willingly volunteered for this study, and the general practitioners and medical clinics who support the participants in the ASPREE study. We also appreciate the support of the collaborating/supporting organisations listed on http://www.aspree.org.
Funding
The work was mainly supported by the National Institute on Aging and the National Cancer Institute at the National Institutes of Health (grant number U01AG029824), the National Health and Medical Research Council of Australia (grant numbers 334047 and 1127060), Monash University, and the Victorian Cancer Agency. Other funding resources and collaborating organisations of the ASPREE study are listed on http://www.aspree.org.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Research involving human participants
This study was conducted in accordance with the Declaration of Helsinki 1964 as revised in 2008, the NHMRC Guidelines on Human Experimentation, the federal patient privacy (HIPAA) law and ICH-GCP guidelines and the International Conference of Harmonisation Guidelines for Good Clinical Practice. We also follow the Code of Federal Regulations as it relates to areas of clinical research. Multiple Institutional Review Board approvals were obtained in Australia and the USA.
Additional information
ASPREE Investigator Group listed on www.aspree.org.
Electronic supplementary material
Below is the link to the electronic supplementary material.
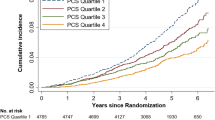
11136_2018_2040_MOESM2_ESM.tif
Online Resource 2 Physical and Mental component summary scores of health-related quality of life among individuals ≥ 65 years in Australia (N=16,703) and the United States (N = 2,411). ASPREE study, baseline (2010–2014) (TIF 835 KB)
11136_2018_2040_MOESM3_ESM.tif
Online Resource 3 Scatter plot of the relationship between age and the Physical (Fig. 2a) and Mental (Fig. 2b) component summary scores of health-related quality of life among individuals ≥ 65 years in Australia (N = 16,703) and the United States (N = 2411). ASPREE study, baseline (2010–2014). (TIF 2004 KB)
Rights and permissions
About this article
Cite this article
Stocks, N.P., González-Chica, D.A., Woods, R.L. et al. Quality of Life for 19,114 participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study and their association with sociodemographic and modifiable lifestyle risk factors. Qual Life Res 28, 935–946 (2019). https://doi.org/10.1007/s11136-018-2040-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-2040-z