Abstract
Purpose
Difficulty swallowing, oropharyngeal dysphagia, is widespread among many patient populations (such as stroke and cancer groups) and aged community-dwelling individuals. It is commonly managed with bolus modification: altering food (usually cutting, mashing or puréeing) or fluids (typically thickening) to make them easier or safer to swallow. Although this treatment is ubiquitous, anecdotal evidence suggests patients dislike this management, and this may affect compliance and well-being. This review aimed to examine the impact of bolus modification on health-related quality of life.
Methods
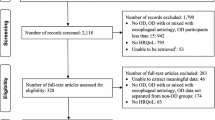
A systematic review of the literature was conducted by speech pathologists with experience in oropharyngeal dysphagia. The literature search was completed with electronic databases, PubMed and Embase, and all available exclusion dates up to September 2012 were used. The search was limited to English-language publications which were full text and appeared in peer-reviewed journals.
Results
Eight studies met the inclusion criteria. Generally, bolus modification was typically associated with worse quality of life. Modifications to foods appeared to be more detrimental than modifications to fluids, but this may be due to the increased severity of dysfunction that is implied by the necessity for significant alterations to foods. The number of studies retrieved was quite small. The diverse nature of methodologies, terminologies and assessment procedures found in the studies makes the results difficult to generalise.
Conclusion
Overall, even though the severity of dysphagia may have been a confounding factor, the impact of bolus modification on health-related quality of life in patients with oropharyngeal dysphagia appears to be negative, with increased modification of food and fluids often correlating to a decreased quality of life. Further, associated disease factors, such as decreased life expectancy, may also have affected health-related quality of life. More research is needed.

Similar content being viewed by others
References
Giudice, E. D., Staiano, A., Capono, G., Romano, A., Florimonte, L., Miele, E., et al. (1999). Gastrointestinal manifestations in children with cerebral palsy. Brain and Development, 21, 307–311.
Langdon, P. C., Lee, A. H., & Binns, C. W. (2007). Dysphagia in acute ischaemic stroke: Severity, recovery and relationship to stroke subtype. Journal of Clinical Neurosciences, 14, 630–634.
Good-Fraturelli, M. D., Curlee, R. F., & Holle, J. L. (2000). Prevalence and nature of dysphagia in VA patients with COPD referred for videofluoroscopic swallow examination. Journal of Communication Disorders, 33, 93–110.
Walker, R. W., Dunn, J. R., & Gray, W. K. (2011). Self-reported dysphagia and its correlates within a prevalent population of people with Parkinson’s Disease. Dysphagia, 26, 92–96.
Aldridge, K., & Taylor, N. (2012). Dysphagia is a common and serious problem for adults with mental illness: A systematic review. Dysphagia, 27, 124–137.
Kawashima, K., Motohashi, Y., & Fujishima, I. (2004). Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia, 19, 266–271.
Chen, P. H., Golub, J., Hapner, E., & Johns, M. (2009). Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia, 24, 1–6.
Holland, G., Jayasekeran, V., Pendleton, N., Horan, M., Jones, M., & Hamdy, S. (2011). Prevalence and symptom profiling of oropharyngeal dysphagia in a community dwelling elderly population: A self-reporting questionnaire survey. Diseases of the Esophagus, 24, 476–480.
Wilkinson, T., & De Picciotto, J. (1998). Swallowing problems in the normal ageing population. The South African journal of communication disorders. Die Suid-Afrikaanse tydskrif vir Kommunikasieafwykings, 46, 55–64.
Meng, N. H., Wang, T. G., & Lien, I. N. (2000). Dysphagia in patients with brainstem stroke: Incidence and outcome. American Journal of Physical Medicine and Rehabilitation, 79(2), 170–175.
Airoldi, M., Garzaro, M., Raimondo, L., Pecorari, G., Giordano, C., Varetto, A., et al. (2011). Functional and psychological evaluation after flap reconstruction plus radiotherapy in oral cancer. Head and Neck, 33(4), 458–468.
Brandāo, D., Nascinmento, J., & Vianna, L. (2010). Functional capacity and quality of life among elderly patients with or without OD after an ischemic stroke. Revista da Associação Médica Brasileira, 56(6), 738–743.
Ward, E. C., Bishop, B., Frisby, J., & Stevens, M. (2002). Swallowing outcomes following laryngectomy and pharyngolaryngectomy. Archives of Otolaryngology-Head and Neck Surgery, 128(2), 181–186.
Thomas, L., Jones, T., Tandon, S., Katre, C., Lowe, D., & Rogers, S. (2008). An evaluation of the University of Washington Quality of Life swallowing domain following oropharyngeal cancer. European Archives of Otorhinolaryngology, 265(S1), S29–S37.
Queija, D., Portas, J., Dedivitis, R., Lehn, C., & Barros, A. (2009). Swallowing and quality of life after total laryngectomy and pharyngolaryngectomy. Brazilian Journal of Otorhinolaryngology, 75(4), 556–564.
Strand, E. A., Miller, R. M., Yorkston, K. M., & Hillel, A. D. (1996). Management of oral-pharyngeal dysphagia symptoms in amyotrophic lateral sclerosis. Dysphagia, 11(2), 129–139.
Hays, N. P., & Roberts, P. B. (2006). The anorexia of aging in humans. Physiology and Behaviour, 88, 257–266.
Berzlanovich, A. M., Fazeny-Dorner, B., Waldhoer, T., Fasching, P., & Keil, W. (2005). Foreign body asphyxia: A preventable cause of death in the elderly. American Journal of Preventative Medicine, 28(1), 65–69.
Langmore, S. E., Terpenning, M. S., Schork, A., Chen, Y., Murray, J. T., Lopatin, D., & Loesche, W. J. (1998). Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia, 13, 69–81.
Ekberg, O., Hamdy, S., Woisard, V., et al. (2002). Social and psychological burden of dysphagia: Its impact on diagnosis and treatment. Dysphagia, 17, 139–146.
Altman, K. W., Yu, G.-P., & Schaeffer, S. D. (2010). Consequence of dysphagia in the hospitalized patient: Impact on prognosis and hospital resources. Archives of Otolaryngology Head and Neck Surgery, 136, 784–789.
Curran, J., & Groher, M. E. (1990). Development and dissemination of an aspiration risk reduction diet. Dysphagia, 5(1), 6–12.
Leder, S. B., Judson, B. L., Sliwinski, E., & Madson, L. (2013). Promoting safe swallowing when puree is swallowed without aspiration but thin liquid is aspirated: Nectar is enough. Dysphagia, 28(1), 58–62.
Lazarus, C. L., Logemann, J. A., Rademaker, A. W., Kahrilas, P. J., Pajak, T., Lazar, R., & Halper, A. (1993). Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Archives of Physical Medicine and Rehabilitation, 74(10), 1066–1070.
Morishita, M., Mori, S., Yamagami, S., & Mizutani, M. (2013). Effect of carbonated beverages on pharyngeal swallowing in young individuals and elderly inpatients. Dysphagia, 29, 1–10.
Martin, A. W. (1991). Dietary management of swallowing disorders. Dysphagia, 6(3), 129–134.
Whelan, K. (2001). Inadequate fluid intakes in dysphagic acute stroke. Clinical Nutrition, 20(5), 423–428.
Finestone, H. M., Foley, N. C., Woodbury, M. G., & Greene-Finestone, L. (2001). Quantifying fluid intake in dysphagic stroke patients; a preliminary comparison of oral and non-oral strategies. Archives of Physical Medicine Rehabilitation, 82(12), 1744–1746.
Ganio, M. S., Armstrong, L. E., Casa, D. J., McDermott, B. P., Lee, E. C., Yamamoto, L. M., et al. (2011). Mild dehydration impairs cognitive performance and mood of men. British Journal of Nutrition, 106(10), 1535.
Armstrong, L. E., Ganio, M. S., Casa, D. J., Lee, E. C., McDermott, B. P., Klau, J. F., et al. (2012). Mild dehydration affects mood in healthy young women. The Journal of Nutrition, 142(2), 382–388.
Bennett, J. A., Thomas, V., & Riegel, B. (2004). Unrecognized chronic dehydration in older adults: Examining prevalence rate and risk factors. Journal of Gerontological Nursing, 30, 22–28.
Yasaka, M., Yamaguchi, T., Oita, J., Sawada, T., Shichiri, M., & Omae, T. (1993). Clinical features of recurrent embolization in acute cardioembolic stroke. Stroke, 24(11), 1681–1685.
Wright, L., Cotter, D., Hickson, M., & Frost, G. (2005). Comparison of energy and protein intakes of older people consuming a texture modified diet with a normal hospital diet. Journal of Human Nutrition & Dietetics, 18(3), 213–219.
Bath, P. M. W., Bath, F. J., & Smithard, D. G. (2000). Interventions for dysphagia in acute stroke. Cochrane Database System Review 4.
Andersen, U. T., Beck, A. M., Kjaersgaard, A., Hansen, T., & Poulsen, I. (2013). Systematic review and evidence based recommendations on texture modified foods and thickened fluids for adults (≥18 years) with oropharyngeal dysphagia. e-SPEN Journal, 8(4), e127–e134.
Colodny, N. (2005). Dysphagia independent feeders’ justifications for noncompliance with recommendations by a speech-language pathologist. American Journal of Speech-Language Pathology, 14, 61–70.
Garcia, J. M., Chambers, E., & Molander, M. (2005). Thickened liquids: Practice patterns of speech-language pathologists. American Journal of Speech Language Pathology, 14, 4–13. doi:10.1044/1058-0360(2005/003.
Pelletier, C. A. (1997). A comparison of consistency and taste of five commercial thickeners. Dysphagia, 12(2), 74–78.
Macqueen, C. E., Taubert, S., Cotter, D., Stevens, S., & Frost, G. S. (2003). Which commercial thickening agent do patients prefer? Dysphagia, 18(1), 46–52.
World Health Organization. (2005). The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science and Medicine, 41(10), 1403–1409.
World Health Organisation. (1997). WHOQOL: Measuring quality of life. http://www.who.int/mental_health/media/68.pdf. Accessed 24 March 2014.
Siwek, J., Gourlay, M. L., Slawson, D. C., & Shaughnessy, A. F. (2002). How to write an evidence-based clinical review article. American Family Physician, 65(2), 251–259.
Rofes, L., Arreola, V., Almirall, J., Cabré, M., Campins, L., García-Peris, P., et al. (2011). Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterology Research and Practice,. doi:10.1155/2011/818979.
Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19–22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
Ferrans, C. E., Zerwic, J. J., Wilbur, J. E., & Larson, J. L. (2005). Conceptual model of health-related quality of life. Journal of Nursing Scholarship, 37(4), 336–342.
Carlaw, C., Finlayson, H., Beggs, K., Visser, T., Marcoux, C., Coney, D., & Steele, C. (2012). Outcomes of a pilot water protocol project in a rehabilitation setting. Dysphagia, 27, 297–306.
Karagiannis, M. J., Chivers, L., & Karagiannis, T. C. (2011). Effects of oral intake of water in patients with oropharyngeal dysphagia. BMC Geriatrics, 11(1), 9.
Wong, D. L., & Baker, C. M. (1988). Pain in children: Comparison of assessment scales. Pediatric Nursing, 14(1), 9–17.
Carlsson, S., Rydén, A., Rudberg, I., Bove, M., & Bergquist, H. (2012). Validation of the Swedish M. D. Anderson OD Inventory (MDADI) in patients with head and neck cancer and neurologic swallowing disturbances. Dysphagia, 27, 361–369.
Finizia, C., Rudberg, I., Bergqvist, H., & Rydén, A. (2012). A cross-sectional validation study of the Swedish version of SWAL-QOL. Dysphagia, 27(3), 325–335.
McHorney, C., Robbins, J., Lomax, K., Rosenbek, J., Chignell, K., Kramer, A., & Bricker, D. (2002). The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia, 17, 97–114.
Vanderwegen, J., Van Nuffelen, G., & De Bodt, M. (2013). The validation and psychometric properties of the Dutch version of the Swallowing Quality-of-Life Questionnaire (DSWAL-QOL). Dysphagia, 28, 11–23.
Zuydam, A. C., Ghazali, N., Lowe, D., Skelly, R., & Rogers, S. N. (2013). Evaluation of the limitations of using the University of Washington Quality of Life swallowing domain alone to screen patients in the routine clinical setting. British Journal of Oral and Maxillofacial Surgery, 51(7), e148–e154.
Timmerman, A. A., Speyer, R., Heijnen, B. J., & Klijn-Zwijnenberg, I. R. (2014). Psychometric characteristics of health-related quality of life questionnaires in oropharyngeal dysphagia. Dysphagia, 9(2), 183–198.
Acknowledgments
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Swan, K., Speyer, R., Heijnen, B.J. et al. Living with oropharyngeal dysphagia: effects of bolus modification on health-related quality of life—a systematic review. Qual Life Res 24, 2447–2456 (2015). https://doi.org/10.1007/s11136-015-0990-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-015-0990-y