Abstract
Purpose
The impact of stigma on subjective wellbeing was explored in adults living with HIV in Australia and the USA. It was hypothesised that this population would report poorer subjective wellbeing than the general population and that ‘felt’ stigma would contribute significantly to reported levels of subjective wellbeing.
Methods
A total of 274 participants were recruited through Australian AIDS councils and HIV-specific online support groups. Participants completed a composite questionnaire comprising the personal wellbeing index—adult (PWI-A), the HIV version of the unsupportive social interactions inventory (USII) and demographic and health-related items. The PWI-A total score was used to form a personal wellbeing index, ranging from 0 to 100.
Results
Participants reported mean PWI-A total scores of 54.7, considerably below the normative range of 70–80 for Western populations. There was a strong negative correlation between PWI-A total scores and USII total scores with the experience of high levels of unsupportive social interactions being associated with reduced levels of subjective wellbeing.
Conclusions
Our study suggests that despite antidiscrimination legislation, ‘felt’ stigma in the form of unsupportive social interactions continues to exert a negative impact on subjective wellbeing. Reduced subjective wellbeing may increase the risk of adverse health behaviours, such as medication non-adherence, substance abuse, risky sexual behaviours and non-disclosure of HIV serostatus.
Similar content being viewed by others
Introduction
In the early 1980s, the emergence of acquired immune deficiency syndrome (AIDS) in developed nations created an ‘epidemic of stigma’ [1] unprecedented in modern day medicine. Three claims dominated early media coverage of the epidemic: it was invariably fatal, it was spreading fast and it was associated with a number of stigmatised behaviours, in particular the ‘gay lifestyle’, intravenous drug use and paid sex [2]. By 2009, almost 60 million people worldwide had been infected with this disease, resulting in 25 million deaths [3]. The retrovirus responsible—the human immunodeficiency virus (HIV)—remains incurable, but in developed nations, no longer inexorably progresses to the life threatening AIDS, following the development of highly active antiretroviral therapy (HAART) in the mid 1990s [4, 5]. The goal of antiretroviral therapy is to suppress viral loads to barely detectable levels in the body, thus transforming HIV into a serious, but controllable, chronic disease [6]. Based on absence of pathology, wellbeing amongst those with access to HAART should have improved. However, many studies continue to indicate that overall physical and emotional wellbeing amongst people living with HIV remains lower than that of the general population, especially as they face the combined effects of ageing and its accompanying comorbidities, the long-term effects of harbouring the virus within their bodies and side effects from ongoing antiretroviral therapy [7–10]. Reports of ‘invisible’ physical and emotional symptoms such as fatigue, depression, weakness, anxiety, fear, worry and difficulty in concentrating [11] highlight that a person’s HIV-related wellbeing extends beyond their symptomatic/asymptomatic status to include subjective experiences and their resultant impact on day-to-day coping and effective management of the disease. Of particular concern are findings indicating that despite antidiscrimination legislation, HIV retains a stigma that can affect health and wellbeing, as, with improved therapies, infected people live longer [7, 12, 13].
Stigma, according to sociologist Erving Goffman, is a deeply discrediting attribute that reduces a person ‘from a whole and usual person to a tainted, discounted one’ [14, p. 3]. Stigma can take the form of actual discrimination, resulting in the stigmatised person existing on the margins of society, or a person’s ‘felt’ stigma, where they live in fear or anticipation of discrimination and rejection, often resulting in an internal sense of shame [14] and reluctance to disclose the stigmatising condition [4]. Disclosure may induce negative social responses in friends, family and colleagues, such as blame, arguments and embarrassment [15, 16], as well as actual or perceived changes in affection and support [17]. Research suggests that these negative or ‘unsupportive social interactions’, especially from loved ones, may have a stronger influence on psychological adjustment than supportive interactions from the same people [18]. Paradoxically, non-disclosure through shame or fear of discrimination can also promote negative affect, feelings of social isolation and damaged self-image for the person living with HIV [15, 19]. An HIV diagnosis can thus be a life-changing experience with a profound impact on identity [4, 20], especially where a person feels subject to ‘victim blaming’ by others who may perceive HIV transmission as voluntary, controllable and avoidable [21]. These personal feelings and experiences can impose significant psychological burdens, underscoring the importance of adopting a subjective approach to exploring wellbeing amongst people living with HIV.
A subjective approach focuses on understanding a person’s feelings about themself and satisfaction with their own life [22, 23]. According to the theory of subjective wellbeing homoeostasis, which underpins the personal wellbeing index—adult (PWI-A) [22] used in this study, subjective wellbeing is internally maintained and defended by a set of psychological devices that are largely influenced by personality and are manifested in a person’s abstract feeling of satisfaction with their life as a whole [23]. The goal of these homoeostatic processes is to maintain a person’s positive view of their self at an abstract, non-specific and stable level, despite short-term positive or negative fluctuations across one or more of eight broader life domains. When expressed on a scale 0–100, the normative range for the Western subjective wellbeing lies in the very narrow range of 70–80 points [22]. The tendency for members of the Western population to maintain a relatively steady level of subjective wellbeing within this range, even in the face of medical challenges, was demonstrated in the Australian Unity wellbeing index report 16.0 [24]. Subjective wellbeing amongst participants with various health conditions requiring them to visit a doctor on a regular basis ranged from 76.6 (blood pressure), 73 (heart problems), 72.8 (asthma), 72.6 (cancer), 70.6 (arthritis), 69.6 (diabetes), 65 (depression) and 63.1 (anxiety). Cummins et al. [24] commented that reduced subjective wellbeing is most apparent in those conditions likely to cause psychological distress, such as severe and unrelenting pain (arthritis) or anxiety/depression. This concurs with reports of reduced subjective wellbeing amongst females with ‘very severe obesity’ (69.5) [25] and amongst injecting drug users (55.4) [26], two conditions that can expose individuals to both psychological distress and discrimination. Where a chronic and strong negative challenge defeats homoeostasis, individuals may experience the dominance of negative, rather than positive affect, which may in turn be an indicator of depression [27].
Research amongst general populations suggests that life satisfaction, described as a ‘desired subjective feeling indicating general wellbeing’ [28, p. 983], may be an important health predictor, with life dissatisfaction linked to increased mortality, adverse health behaviours (such as smoking, heavy drinking and inactivity), obesity, somatic complaints, and depressive and anxiety symptoms [28, 29]. Amongst HIV-infected individuals, monitoring subjective feelings of wellbeing and life satisfaction may provide an important health risk indicator for adverse behaviours such as alcohol and substance abuse, treatment non-adherence, unsafe sexual behaviour and HIV non-disclosure, all of which have been identified as potential negative impacts on disease burden [9, 11, 13, 17, 30–33].
The sense of urgency and fear synonymous with the epidemic’s early years has abated, leaving behind a HIV-positive population that is both ‘growing and greying’ [34, p. 1] as new infections continue to occur and those previously infected survive and age [10]. According to the UNAIDS Report on the Global AIDS Epidemic 2010 [35], there is strong evidence for a resurgence of HIV in many high-income countries with older epidemics, particularly amongst men who have sex with men. This suggests that despite the availability of increasingly sophisticated medications, understanding subjective wellbeing and potential negative challenges remains clinically and socially important.
The present study
The aim of the present study was to explore subjective wellbeing amongst people living with HIV in two English-speaking developed nations—USA and Australia. Response sets from these groups were pooled after independent-samples t tests conducted on demographics and scales of interest indicated no significant differences. Of particular interest was the impact of HIV-related stigma on reported subjective wellbeing.
It was hypothesised that people living with HIV in Australia and in the USA would report lower subjective wellbeing than members of the general population. It was also hypothesised that, for people living with HIV in Australia and in the USA, ‘felt’ stigma, in the form of unsupportive social interactions, would contribute significantly to reported levels of subjective wellbeing.
Materials and methods
Study population and recruitment
A cross-sectional study was completed amongst 274 people living with HIV in Australia (n = 128) and in the USA (n = 146). This comprised a convenience sample recruited through Australian capital city AIDS councils as well as Australia-based and USA-based HIV-specific online support groups accessed through the social networking services of Facebook and Yahoo Groups. Individuals over the age of 18 years and living with HIV were invited via recruitment flyers and online message boards to complete the anonymous questionnaire in pen-and-paper format or via a web-based service tool.
There were 73 (26.6%) pen-and-paper responders and 201 (73.4%) online responders. Independent-samples t tests on demographics and the variables of interest revealed no significant differences based on questionnaire delivery mode. The final sample comprised 274 participants, aged between 18 and 84 years (M = 47.05, SD = 11.02). Participants reported living with HIV from less than a year up to 30 years (M = 13.54, SD = 7.95). The majority of participants were male (91.2%) and described themselves as homosexual (78.8%), reflecting the over-representation of HIV infections amongst men who have sex with men and the gay communities in many developed nations [35, 36]. Over 80% of participants lived in urban regions, and 54% relied on some form of government income support benefits, especially disability support payments. Non-HIV-related comorbidities were reported in 55.1% of participants, and 43.8% described their health as ‘average’ (29.9%) or ‘poor’ (13.9%). Table 1 shows the characteristics of participants.
Measures
The findings presented in this paper are part of a larger study on wellbeing when living with HIV. The measures examined here are the personal wellbeing index—adult (PWI-A) [22], the HIV version of the unsupportive social interactions inventory (USII) [37], demographics and participants’ self-assessed health status (excellent, good, average, poor).
The PWI-A [22] is a 9-item measure of responders’ abstract feeling of satisfaction with ‘life as a whole’ and eight broad life domains: standard of living; personal health; achieving in life; personal relationships; feeling safe; community-connectedness; future security; and spirituality-religion. These eight domains comprise the minimum set of domains that represent the first level of deconstruction of ‘life as a whole’. Responders indicated their satisfaction with each item on a 0–10 Likert response scale ranging from ‘completely dissatisfied’ (0) to ‘completely satisfied’ (10). Data can be used at the level of individual items, or the eight life domains can be aggregated and averaged to form a personal wellbeing index on a scale 0–100. Previous studies report Cronbach’s alpha for this measure to be between 0.70 and 0.85 in Australia and overseas [22]. In this study, Cronbach’s alpha for the PWI-A total was 0.91.
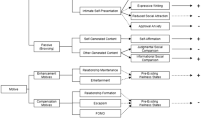
HIV-related unsupportive social interactions were assessed using the HIV-specific version of the USII [37]. Unsupportive social interactions are conceptualised as unhelpful or upsetting responses from other people that a person receives about their HIV status. This scale comprises 24 items, grouped into four factors of six items each. These factors are labelled ‘insensitivity’ reflecting unsupportive behaviours of discomfort, avoidance and lack of empathy; ‘disconnecting’ representing emotional or behavioural disengagement, as well as refusals to provide support; ‘forced optimism’ reflecting attempts to impose a focus on the positive and to ignore or downplay the difficulties of living with HIV; and ‘blaming’ representing criticism, fault-finding and disapproval. Participants were asked to rate the occurrence of events such as After becoming aware of my having HIV, someone avoided me or had less contact than usual, on a five-point Likert scale ranging from ‘Never’ (0) to ‘A lot’ (4). The USII is scored by calculating the mean rating across the items for each subscale. In previous studies, Cronbach’s alpha for the subscales have been between 0.85 and 0.87 for ‘insensitivity’; 0.83–0.84 for ‘disconnecting’; 0.78–0.81 for ‘forced optimism’; and 0.86–0.88 for ‘blaming’ [16, 37]. In this study, Cronbach’s alpha was 0.88, 0.87, 0.88 and 0.87, respectively.
Data screening
Any responders who failed to provide key demographic information or were missing data from entire subscales were excluded (1 pen-and-paper responder and 55 online responders). The percentage of missing data across the two measures used in this paper ranged from 0 to 1.1% and indicated no trends. As recommended by Tabachnick and Fidell [38], group means were used to replace missing values prior to analysis.
The total sample comprised 305 adults living with HIV in the USA (n = 146), Australia (n = 128), United Kingdom (n = 16), Europe (n = 5), Canada (n = 4), Africa (n = 4) and Asia (n = 2). Given that the lived experience of HIV can vary depending on a country’s epidemiological patterns, community attitudes and health system, responders from the latter five areas were excluded due to insufficient numbers for meaningful comparisons. The final sample comprised 128 responders from Australia and 146 responders from the USA. These groups were pooled after independent-samples t tests conducted on demographics, and the two scales of interest indicated no significant differences.
Analyses
The relationship between subjective wellbeing and unsupportive social interactions was investigated using Pearson product–moment correlation coefficient (Table 3), and a series of standard multiple regressions were conducted (Table 4). Potential confounders, including age, years living with HIV and self-assessed health, were controlled for in the analyses. All statistical analyses were performed using IBM SPSS statistics 19 [39].
Results
Range, means (M) and standard deviations (SD) for the measured variables are shown in Table 2. Of particular note is the mean score of 54.7 points for PWI-A total (i.e. aggregate of eight domains), as well as substantially reduced scores in the domains of future security (M = 46.4, SD = 28.6) and community-connectedness (M = 50, SD = 29.9). The mean score for the total USII was 1.54 (SD = 1.05; range, 0–4). The highest level of unsupportive social interactions was reported on the ‘insensitivity’ factor (M = 1.77, SD = 1.05), followed by ‘disconnecting’ (M = 1.59, SD = 0.97), ‘forced optimism’ (M = 0.51, SD = 0.99) and ‘blaming’ (M = 1.29, SD = 0.98). Only six responders (2.2%) from the total sample reported never having experienced HIV-related unsupportive social interactions.
The relationship between subjective wellbeing, as measured by the PWI-A, and unsupportive social interactions, as measured by the USII, was investigated using Pearson product–moment correlation coefficient (see Table 3). There was a negative correlation between the PWI-A abstract feeling of satisfaction with ‘life as a whole’ item and USII total score, r = −0.39, p = 0.000, and between PWI-A total (i.e. aggregate of eight domains) and USII total, r = −0.52, p = 0.000. In both cases, unsupportive social interactions were associated with reduced subjective wellbeing. The four factors of the USII were each significantly associated with PWI-A satisfaction with ‘life as a whole’, PWI-A total and each of the eight individual PWI-A domains. Of the four USII factors, ‘insensitivity’ had the strongest association with: PWI-A satisfaction with ‘life as a whole’, r = −0.38, p = 0.000; PWI-A total, r = −0.54, p = 0.000; and each individual PWI-A domain.
To further examine the relationship between PWI-A and USII, a series of multiple regression analyses were conducted. Firstly, a standard multiple regression on PWI-A total scores was conducted with age, years with HIV, self-rated health and USII total as predictors. The amount of variance in PWI-A total scores explained was 45.3%, F (4, 269) = 57.56, p < 0.001, with USII total accounting for 10% unique variance (see Table 4).
A series of eight multiple regression analyses were conducted for each of the PWI-A domains with age, years with HIV, self-rated health and USII total as predictors. A Bonferroni adjustment was made resulting in an alpha level of 0.006. For all eight PWI-A domains, USII total was a significant predictor at p < 0.001, contributing unique variances of 3% (personal health); 4.7% (spirituality-religion); 5.2% (feeling safe); 5.4% (personal relationships); 5.5% (standard of living); 7.6% (achieving in life); 7.7% (future security); and 11.2% (community-connectedness).
Discussion
Our study indicates that living with HIV in two developed nations, Australia and the USA, is associated with a reported level of subjective wellbeing significantly below the Western normative range of 70–80 points [22], and that increased experiences of HIV-related unsupportive social interactions are predictive of this low level of subjective wellbeing. This supports our hypotheses that people living with HIV in Australia and in the USA would report lower subjective wellbeing than members of the general population and that for this population, ‘felt’ stigma, in the form of unsupportive social interactions, would contribute significantly to reported levels of subjective wellbeing.
These results suggest that living with HIV may undermine the homoeostatic processes that work to maintain a person’s positive view of their self at an abstract, non-specific and stable level, resulting in loss of normal positive affect and the PWI-A providing a potential diagnostic indicator of depression [27]. Living with HIV is not a ‘short-term’ fluctuation across the health or other life domains. Rather, it can result in sufficient distress to substantially reduce subjective wellbeing below many other chronic diseases or conditions, even those causing severe and unrelenting pain (arthritis) or psychological distress (anxiety/depression) [24], and those associated with increased health risks and discrimination (obesity and injecting drug use) [25, 26].
This is valuable information for service providers and public health policy makers in two interrelated areas: (1) identification that some individuals living with HIV are at a risk of loss of positive affect and depression, which may be associated with adverse health behaviours and outcomes; and (2) identification of life domains most affected by the chronic and strong negative challenge of ‘felt’ stigma, thus allowing targeted interventions such as public health initiatives to address the more subtle nuances of HIV-related stigma. These are elaborated below.
Subjective wellbeing, negative affect and depression
There is evidence that individuals with life dissatisfaction, depression or depressive symptomatology may be less likely to tend to their general health and more likely to engage in adverse health behaviours [28, 29, 40]. Importantly, amongst HIV-infected adults, depression and depressive symptomatology have been linked to substance abuse [30, 41–43]; non-adherence to HIV medications [43, 44]; high drop-out rates in HIV-related clinical trials and health-related programmes [45, 46]; and sexual risk behaviours [44, 47], any of which can contribute to less controlled management of the condition and detectable viral loads [43]. Whilst the direct relationship between depression and sexual risk behaviour remains inconsistent and inconclusive [42, 47], there is evidence that depression may indirectly contribute to sexual risk taking by eroding a person’s self-efficacy [47] or increasing the likelihood of alcohol and substance abuse [42, 47, 48]. Directly or indirectly, depression may be a pivotal link to many of the adverse health behaviours associated with HIV, thus highlighting the importance of early recognition of individuals and groups at risk.
There are some estimates that up to half of HIV-positive adults will experience depression or depressive symptomatology at some point in their lifetime [11, 30, 47, 49]. According to Cummins et al. [24], individual scores on the PWI-A below 50 points are indicative of depression, while group mean scores below 70 points indicate that a higher than normal proportion of the sample is depressed. In this study, the group mean score of 54.7 points provides a warning that it is likely that some participants may be at risk of reduced positive affect or depression and therefore susceptible to the aversive health behaviours described above. Service providers could use this knowledge to facilitate timely and targeted interventions.
An important prerequisite of targeted interventions is the ability to pinpoint negative challenges to subjective wellbeing and life domains most affected by those challenges. In this study, living with HIV was found to particularly impact a person’s satisfaction with their future security (46.4 points) and with feeling part of their community (50 points). Amongst people with HIV, ‘uncertainty in illness’ [50], where patients with chronic illness express uncertainty about symptoms and lack of information about the future, has been associated with stress and anxiety and exacerbated by the threat of stigma and social isolation [51]. Stigma and social isolation may, in turn, negatively impact on feelings of community-connectedness. It is therefore noteworthy that this study identified ‘felt’ stigma, in the form of unsupportive social interactions, to be a negative challenge strongly associated with reduced subjective wellbeing.
Subjective wellbeing and ‘felt’ stigma
The concept of stigma is now a recognised component of the social impact of some diseases and conditions, contributing to the burden of illness, influencing clinical outcomes, and associated with symptoms of depression, anxiety and hopelessness [33, 46, 52, 53]. Amongst people with HIV, fear of stigma and exclusionary social processes can create a barrier to HIV testing, interfere with treatment and increase non-disclosure of HIV serostatus [19, 33, 46, 54], all of which may have serious ramifications for the individual, service providers and public health initiatives.
Over 90% of countries globally have programmes in place to reduce HIV-related stigma and discrimination [35]. In many developed nations, this has been formalised into legislation to prevent discrimination, harassment or victimisation by businesses, service providers and employers. Nevertheless, 97.8% of participants in the current study reported experiencing some form of HIV-related unsupportive social interaction. With some research indicating that negative or unsupportive social interactions, especially from personal social networks, can have a stronger influence on psychological adjustment, mood disturbances and depressive symptomatology than supportive interactions [16, 17, 37, 55, 56], the finding that increased experiences of unsupportive social interactions negatively impacted on an individual’s subjective wellbeing, irrespective of their age, years with HIV and self-assessed health status, is not surprising. Many of the USII items elicit information about a person’s experience of intangible upsetting interactions, such as picking up from someone’s tone of voice, expression or body language that they were uncomfortable talking about the person having HIV, feeling that they were avoided or that someone had become ‘cold’ towards them because of their HIV, and feeling that someone was disappointed in them. A variable strongly associated with subjective wellbeing and life satisfaction is ‘satisfaction with self’ [57, p. 62]. Therefore, any events undermining ‘satisfaction with self’, such as the perception that unsupportive social interactions are occurring, irrespective of whether the other person was deliberately, or even actually, acting in this manner, may reduce subjective wellbeing.
Current findings indicate that while unsupportive social interactions were negatively correlated with, and predictive of, all eight domains of the PWI-A, this was most evident in relation to the community-connectedness domain (i.e. How satisfied are you with feeling part of your community?). Many aspects of HIV remain misunderstood by the general population; however, its principal modes of transmission by sexual fluids, blood and intravenous drug use are public knowledge. Fear of contagion and negative attitudes about the behaviours associated with contracting HIV can cause some people to react censoriously [18, 55, 56]. Rules of physical contact may be overtly or covertly reconstructed in ways that leave the person with HIV feeling rejected, fearful, frustrated, hurt, angry and socially isolated from their community [17].
Experiences of HIV-related social rejection have serious implications for disclosure of HIV serostatus. There is evidence of a clear association between stigma and disclosure, with rates of disclosure linked to how much communities stigmatise or accept HIV and how individuals perceive themselves, their identities and their roles in their communities [58]. Fear of negative reactions from others can act as a deterrent to both HIV testing and subsequent disclosure [19, 31, 33, 52, 54, 59]. On a societal level, this may contribute to the continued HIV epidemic through inadvertent transmission of the virus by undiagnosed individuals within the community [46]. On a personal level, this may impact health outcomes by delaying or interfering with treatments, thus increasing the risk of higher viral loads and damage to the immune system [46, 52, 54, 59]. Whilst stigma and disclosure are pertinent to all age groups, there is evidence that some older adults with HIV may perceive greater stigma attached to their condition due to societal attitudes about ageing, sexuality and sexual orientation [52, 55, 60]. Some maintain a ‘protective silence’ [60, p. 787] about their condition, increasing the risk of social isolation and diminished emotional support. This highlights the need to address both HIV-related stigma and ageist attitudes as more members of the HIV population enter old age.
A limitation of this study is that participants were self-selected via recruitment flyers and online message boards. Given the obstacles to HIV testing and disclosure noted earlier, some potential participants may not have been accessed. In addition, the cross-sectional design of this study precludes any causal interpretations. Future longitudinal studies are recommended to gain greater understanding of the relationship between subjective wellbeing and experiences of ‘felt’ stigma throughout the course of the disease.
Conclusion
In summary, our study has important clinical and social implications. Firstly, by using the PWI-A, a sensitive and non-confrontational instrument underpinned by theory and research, we identified that living with HIV can be associated with reduced subjective wellbeing, which in turn may be a potential diagnostic indicator of depression. This can leave some individuals susceptible to adverse health behaviours, such as medication non-adherence, substance abuse and risky sexual behaviours. Early identification of at-risk individuals could facilitate targeted health promotion initiatives to strengthen and maintain a person’s ‘satisfaction with self’ and coping skills.
Secondly, our study draws attention to the subtle and nuanced stigmatising behaviours perceived in others that may be a strong negative challenge to subjective wellbeing. Whilst it is not feasible to legislate against ‘felt’ stigma and unsupportive social interactions, service providers and policy makers can incorporate this knowledge into existing education and health promotion initiatives promoting safe and comfortable HIV disclosure. Simultaneously, our results support the ongoing need for public education initiatives to combat lingering erroneous perceptions about living and ageing, with HIV in the twenty-first century.
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- HIV:
-
Human immunodeficiency virus
- HAART:
-
Highly active antiretroviral therapy
- PWI-A:
-
Personal wellbeing index—adult
- USII:
-
Unsupportive social interactions inventory
References
Herek, G., & Glunt, E. (1988). An epidemic of stigma: Public reactions to AIDS. American Psychologist, 43, 886–891.
Curran, J. W. (2006). Reflections on AIDS: Lessons for the future. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 83(1), 1–2.
UNAIDS. (2009). AIDS epidemic update. http://data.unaids.org/pub/FactSheet/2009/20091124_FS_global_en.pdf. Accessed Jan 5, 2011.
Green, G. (2009). The end of stigma? Changes in the social experience of long term illness. Oxford: Routledge.
Murdaugh, C., Moneyham, L., Jackson, K., Phillip, K., & Tavakoli, A. (2006). Predictors of quality of life in HIV-infected rural women: Psychometric test of the chronic illness quality of life ladder. Quality of Life Research, 15, 777–789.
Long, M. C., King, J. R., & Acosta, E. P. (2009). Pharmacologic aspects of new antiretroviral drugs. Current HIV/AIDS Reports, 6, 43–50.
O’Cleirigh, C., & Safren, S. A. (2006). Domains of life satisfaction among patients living with HIV: A factor analytic study of the quality of life inventory. AIDS and Behavior, 10, 53–58.
Hansen, N. B., Vaughan, E. L., Cavanaugh, C. E., Connell, C. M., & Sikkema, K. J. (2009). Health-related quality of life in bereaved HIV-positive adults: Relationships between HIV symptoms, grief, social support, and axis II indication. Health Psychology, 28, 249–257.
Kohli, R., Klein, R. S., Schoenbaum, E. E., Anastos, K., Minkoff, H., & Sacks, H. S. (2006). Aging and HIV infection. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 83, 31–42.
Murray, J. M., McDonald, A., & Law, M. (2009). Rapidly ageing HIV epidemic among men who have sex with men in Australia. Sexual Health, 6, 83–86.
Willard, S., Holzemer, W. L., Wantland, D. J., Cuca, Y. P., Kirksey, K. M., Portillo, C. J., et al. (2009). Does “asymptomatic” mean without symptoms for those living with HIV infection? AIDS Care, 21, 322–328.
Bunn, J. Y., Solomon, S. E., Miller, C., & Forehand, R. (2007). Measurement of stigma in people with HIV: A reexamination of the HIV stigma scale. AIDS Education and Prevention, 19, 198–208.
Harding, R., & Molloy, T. (2008). Positive futures? The impact of HIV infection on achieving health, wealth and future planning. AIDS Care, 20, 565–570.
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster, Inc.
Sandelowski, M., Lambe, C., & Barroso, J. (2004). Stigma in HIV-positive women. Journal of Nursing Scholarship, 36, 122–128.
Song, Y. S., & Ingram, K. M. (2002). Unsupportive social interactions, availability of social support, and coping: Their relationship to mood disturbance among African Americans living with HIV. Journal of Social and Personal Relationships, 19, 67–85.
Zukoski, A. P., Thorburn, P. H., & Thorburn, S. (2009). Experiences of stigma and discrimination among adults living with HIV in a low HIV-prevalence context: A qualitative analysis. AIDS Patient Care and STDs, 23, 267–276.
Schrimshaw, E. W. (2003). Relationship-specific unsupportive social interactions and depressive symptoms among women living with HIV/AIDS: Direct and moderating effects. Journal of Behavioral Medicine, 26, 297–313.
Petrak, J. A., Doyle, A.-M., Smith, A., Skinner, C., & Hedge, B. (2001). Factors associated with self-disclosure of HIV serostatus to significant others. British Journal of Health Psychology, 6, 69–79.
Fife, B. L., Scott, L. L., Fineberg, N. S., & Zwickl, B. E. (2008). Promoting adaptive coping by persons with HIV disease: Evaluation of a patient/partner intervention model. Journal of the Association of Nurses in AIDS Care, 19(1), 75–84.
Swendeman, D., Rotheram-Borus, M. J., Comulada, S., Weiss, R., & Ramos, M. E. (2006). Predictors of HIV-related stigma among young people living with HIV. Health Psychology, 25(4), 501–509.
International Wellbeing Group. (2006). Personal wellbeing index (4th ed.). Melbourne: Australian Centre on Quality of Life, Deakin University.
Cummins, R. A., Lau, A. L. D., & Stokes, M. (2004). HRQOL and subjective well-being: Noncomplementary forms of outcome measurement. Expert Review of Pharmacoeconomics and Outcomes Research, 4, 413–420.
Cummins, R. A., Lau, A. L. D., Mellor, D., & Stokes, M. A. (2009). Encouraging governments to enhance the happiness of their nation: Step 1: Understand subjective wellbeing. Social Indicators Research, 91, 21–36.
Mead, R., & Cummins, R. A. (2008). Australian Unity wellbeing index: Report 18.2: What makes us happy? Melbourne: Australian Unity and Deakin University.
Dietze, P., Stoove, M., Miller, P., Kinner, S., Bruno, R., Alati, R., et al. (2010). The self-reported personal wellbeing of a sample of Australian injecting drug users. Addiction, 105, 2141–2148.
Cummins, R. A. (2010). Subjective wellbeing, homeostatically protected mood and depression: A synthesis. Journal of Happiness Studies, 11, 1–17.
Koivumaa-Honkanen, H., Honkanen, R., Vinamaki, H., Heikkila, K., Kaprio, J., & Koskenvuo, M. (2000). Self-reported life satisfaction and 20-year mortality in health Finnish adults. American Journal of Epidemiology, 152(10), 983–991.
Strine, T. W., Chapman, D. P., Balluz, L. S., Moriarty, D. G., & Mokdad, A. H. (2008). The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviours among US community-dwelling adults. Journal of Community Health, 33, 40–50.
Lemstra, M., Rogers, M., Thompson, A., Moraros, J., & Buckingham, R. (2011). Risk indicators of depressive symptomatology among injection drug users and increased HIV risk behaviour. Canadian Journal of Psychiatry, 56(6), 358–366.
Derlega, V. J., Winstead, B. A., Greene, K., Serovich, J., & Elwood, W. N. (2004). Reasons for HIV disclosure/nondisclosure in close relationships: Testing a model of HIV-disclosure decision making. Journal of Social and Clinical Psychology, 23(6), 747–767.
Remien, R. H., Exner, T. M., Morin, S. F., Ehrhardt, A. A., Johnson, M. O., Correale, J., et al. (2007). Medication adherence and sexual risk behaviour among HIV-infected adults: Implications for transmission of resistant virus. AIDS and Behavior, 11, 663–675.
Courtenay-Quirk, C., Wolitski, R. J., Parsons, J. T., Gomez, C. A., & the Seropositive Urban Men’s Study Team. (2006). Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV-positive men who have sex with men. AIDS Education and Prevention, 18(1), 56–67.
Karpiak, S. E., & Brennan, M. (2009). The emerging population of older adults with HIV and introduction to ROAH the research study. In M. Brennan, S. E. Karpiak, R. A. Shippy, & M. H. Cantor (Eds.), Older adults with HIV: An in-depth examination of an emerging population (pp. 1–12). New York: Nova Science Publishers, Inc.
UNAIDS (2010). Global report: UNAIDS report on the global AIDS epidemic 2010. http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2010/20101123_globalreport_en.pdf. Accessed May 11, 2011.
Grierson, J., Power, J., Pitts, M. Croy, S., Clement, T., Thorpe, R. et al. (2009). HIV Futures 6: Making positive lives count. Monograph series number 74. Melbourne: The Australian Research Centre in Sex, Health and Society, LaTrobe University.
Ingram, K. M., Jones, D. A., Fass, R. J., Neidig, J. L., & Song, Y. S. (1999). Social support and unsupportive social interactions: Their association with depression among people living with HIV. AIDS Care, 11, 313–329.
Tabbachnick, B. G., & Fidell, L. S. (2001). Using multivariate statistics (4th ed.). Needham Heights: Allyn & Bacon.
IBM. (2010). IBM SPSS Statistics 19. Chicago: Author.
Allgower, A., Wardle, J., & Steptoe, A. (2001). Depressive symptoms, social support, and personal health behaviours in young men and women. Health Psychology, 20(3), 223–227.
Sherbourne, C. D., Hays, R. D., Fleishman, J. A., Vitiello, B., Magruder, K. M., Bing, E. G., et al. (2000). Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. The American Journal of Psychiatry, 157(2), 248–254.
Comulda, W. S., Rotheram-Borus, M. J., Weiss, R. E., Desmond, K. A., Remien, R. H., Weinhardt, L. S., et al. (2010). Relationships over time between mental health symptoms and transmission risk among persons living with HIV. Psychology of Addictive Behaviors, 24(1), 109–118.
Mellins, C. A., Havens, J. F., McDonnell, C., Lichtenstein, C., Uldall, K., Chesney, M., et al. (2009). Adherence to antiretroviral medications and medical care in HIV-infected adults diagnosed with mental and substance abuse disorders. AIDS Care, 21(2), 168–177.
Heckman, T. G., Heckman, B. D., Kochman, A., Sikkema, K. J., Suhr, J., & Goodkin, K. (2002). Psychological symptoms among persons 50 years of age and older living with HIV disease. Aging and Mental Health, 6(2), 121–128.
Johnson, M. O., Dilworth, S. E., Neilands, T. B., Chesney, M. A., Rotheram-Borus, M. J., Remien, R. H., et al. (2008). Predictors of attrition among high risk HIV-infected participants enrolled in a multi-site prevention trial. AIDS and Behavior, 12, 974–977.
Vanable, P. A., Carey, M. P., Blair, D. C., & Littlewood, R. A. (2006). Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS and Behavior, 10(5), 473–482.
Alvy, L. M., McKirnan, D. J., Mansergh, G., Koblin, B., Colfax, G. N., Flores, S. A., et al. (2011). Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS and Behavior, 15, 1171–1179.
Gaynes, B. N., Pence, B. W., Eron, J. J., & Miller, W. C. (2008). Prevalence and comorbidity of psychiatric diagnoses based on reference standard in an HIV+ population. Psychosomatic Medicine, 70, 505–511.
Appelbaum, A., & Brennan, M. (2009). Mental health and depression. In M. Brennan, S. E. Karpiak, R. A. Shippy, & M. H. Cantor (Eds.), Older adults with HIV: An in-depth examination of an emerging population (pp. 27–42). New York: Nova Science Publishers, Inc.
Neville, K. L. (2003). Uncertainty in illness: An integrative review. Orthopaedic Nursing, 22(3), 206–214.
Brashers, D. E., Neidig, J. L., Russell, J. A., Cardillo, L. W., Haas, S. M., Dobbs, L. K., et al. (2003). The medical, personal, and social causes of uncertainty in HIV illness. Issues in Mental Health Nursing, 24, 497–522.
Emlet, C. A. (2007). Experiences of stigma in older adults living with HIV/AIDS: A mixed methods analysis. AIDS Patient Care and STDs, 21(10), 740–752.
Weiss, M. G., Ramakrishna, J., & Somma, D. (2006). Health-related stigma: Rethinking concepts and interventions. Psychology, Health and Medicine, 11(3), 277–287.
Wallace, S. A., McLellan-Lemal, E., Harris, M. J., Townsend, T. G., & Miller, K. S. (2011). Why take an HIV test? Concerns, benefits, and strategies to promote HIV testing among low-income heterosexual African American young adults. Health Education Behavior, 38, 462–470.
Schrimshaw, E. W., & Siegel, K. (2003). Perceived barriers to social support from family and friends among older adults with HIV/AIDS. Journal of Health Psychology, 8, 738–752.
Siegel, K., Raveis, V. H., & Karus, D. (1997). Illness-related support and negative network interactions: Effects on HIV-infected men’s depressive symptomatology. American Journal of Community Psychology, 25, 395–420.
Cummins, R. A., & Nistico, H. (2002). Maintaining life satisfaction: The role of positive cognitive bias. Journal of Happiness Studies, 3, 37–69.
Arnold, M. E., Rice, E., Flannery, D., & Rotheram-Borus, J. (2008). HIV disclosure among adults living with HIV. AIDS Care, 20(1), 80–92.
Peretti-Watel, P., Spire, B., Pierret, J., Lert, F., Obadia, Y., & the Vespa Group. (2006). Management of HIV-related stigma and adherence to HAART: Evidence from a large representative sample of outpatients attending French hospitals (ANRS-EN12-VESPA 2003). AIDS Care, 18(3), 254–261.
Emlet, C. A. (2006). “You’re awfully old to have this disease”: Experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. The Gerontologist, 46(6), 781–790.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study has been approved by the Monash University Standing Committee on Ethics in Research Involving Humans (Approval Number CF09/1014-2009000505).
Rights and permissions
About this article
Cite this article
Hutton, V.E., Misajon, R. & Collins, F.E. Subjective wellbeing and ‘felt’ stigma when living with HIV. Qual Life Res 22, 65–73 (2013). https://doi.org/10.1007/s11136-012-0125-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-012-0125-7