Abstract
Aims
Missing health-related quality of life (HRQOL) data in clinical trials can impact conclusions but the effect has not been thoroughly studied in HIV clinical trials. Despite repeated recommendations to avoid complete case (CC) analysis and last observation carried forward (LOCF), these approaches are commonly used to handle missing data. The goal of this investigation is to describe the use of different analytic methods under assumptions of missing completely at random (MCAR), missing at random (MAR), and missing not at random (MNAR) using HIV as an empirical example.
Methods
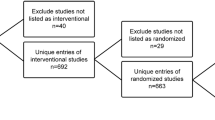
Medical Outcomes Study HIV (MOS-HIV) Health Survey data were combined from two large open-label multinational HIV clinical trials comparing treatments A and B over 48 weeks. Inclusion in the HRQOL analysis required completion of the MOS-HIV at baseline and at least one follow-up visit (weeks 8, 16, 24, 40, 48). Primary outcomes for the analysis were change from week 0 to 48 in mental health summary (MHS), physical health summary (PHS), pain and health distress scores analyzed using CC, LOCF, generalized estimating equations (GEE), direct likelihood and sensitivity analyses using joint mixed-effects model, and Markov chain Monte Carlo (MCMC) multiple imputation. Time and treatment were included in all models. Baseline and longitudinal variables (adverse event and reason for discontinuation) were only used in the imputation model.
Results
A total of 511 patients randomized to treatment A and 473 to treatment B completed the MOS-HIV at baseline and at least one follow-up visit. At week 48, 71% of patients on treatment A and 31% on treatment B completed the MOS-HIV survey. Examining changes within each treatment group, CC and MCMC generally produced the largest or most positive changes. The joint model was most conservative; direct likelihood and GEE produced intermediate results; LOCF showed no consistent trend. There was greater spread for within-group changes than between-group differences (within MHS scores for treatment A: −0.1 to 1.6, treatment B: 0.4 to 2.0; between groups: −0.7 to 0.4; within PHS scores for treatment A: −1.5 to 0.4, treatment B: −1.7 to −0.2; between groups: 0.1 to 1.1). The size of within-group changes and between-group differences was of similar magnitude for the pain and health distress scores. In all cases, the range of estimates was small <0.2 SD (less than 2 points for the summary scores and 5 points for the subscale scores).
Conclusions
Use of the recommended likelihood-based models that do not require assumptions of MCAR was very feasible. Sensitivity analyses using auxiliary information can help to investigate the potential effect that missing data have on results but require planning to ensure that relevant data are prospectively collected.





Similar content being viewed by others
References
Walensky, R. P., Paltiel, A. D., Losina, E., Mercincavage, L. M., Schackman, B. R., Sax, P. E., Weinstein, M. C., & Freedberg, K. A. (2006) The survival benefits of AIDS treatment in the United States. The Journal of Infectious Diseases, 194(1), 11–19.
Sax, P. E., Gathe, J. C. Jr. (2005). Beyond efficacy: The impact of combination antiretroviral therapy on quality of life. AIDS Patient Care STDS, 19(9), 563–576.
Cohen, C., Revicki, D. A., Nabulsi, A., Sarocco, P. W., & Jiang, P. (1998). A randomized trial of the effect of ritonavir in maintaining quality of life in advanced HIV disease. Advanced HIV Disease Ritonavir Study Group. AIDS, 12(12), 1495–1502.
Little, R. J. A., & Rubin, D. B. (1987). Statistical analysis with missing data. New York: John Wiley & Sons.
Donaldson, G. W., & Moinpour, C. M. (2005). Learning to live with missing quality-of-life data in advanced-stage disease trials. Journal of Clinical Oncology, 22(1), 1–5.
Fairclough, D. L. et al. (1998). Comparison of several model-based methods for analysing incomplete quality of life data in cancer clinical trials. Statistics in Medicine, 17, 781–96.
Fairclough, D. L. (2002). Design and analysis of quality of life studies in clinical trials. Boca Raton, Florida: Chapman & Hall/CRC.
Fairclough, D. L. (2004). Patient reported outcomes as endpoints in medical research. Statistical Methods in Medical Research, 13, 115–138.
FDA. (2006). Draft guidance for industry on patient-reported outcome measures: use in medicinal product development to support labeling claims. Federal Register, 71, 5862–5863.
Mallinckrodt, C. H., Christopher, J. Kaiser, C. J., Watkin, J. G., Detke, M. J., Molenberghs, G., & Carroll, R. J. (2004). Type I error rates from likelihood-based repeated measures analyses of incomplete longitudinal data. Pharmaceutical Statistics, 3, 171–186.
Schafer, J. L., & Graham, J. W. (2002). Missing data: our view of the state of the art. Psychological Methods, 7(2), 147–177.
Cohen, C. J., Clumeck, N., Molina, J. M., Thompson, M., Patel, K., Wintfeld, N., & Green, J. (2004). Health-related quality of life with enfuvirtide (ENF; T-20) in combination with an optimized background regimen. Journal of Acquired Immune Deficiency Syndromes, 37(1), 1140–1146.
Revicki, D. A., Swartz, C., Wu, A. W., Haubrich, R., & Collier, A. C. (1999). Quality of life outcomes of saquinavir, zalcitabine and combination saquinavir plus zalcitabine therapy for adults with advanced HIV infection with CD4 counts between 50 and 300 cells/mm3. Antiviral Therapy, 4(1), 35–44.
van Leth, F., Conway, B., Laplume, H., Martin, D., Fisher, M., Jelaska, A., Wit, F. W., Lange, J. M. & 2NN study group. (2004). Quality of life in patients treated with first-line antiretroviral therapy containing nevirapine and/or efavirenz. Antiviral Therapy, 9(5), 721–728.
Casado, A., Badia, X., Consiglio, E., Ferrer, E., Gonzalez, A., Pedrol, E., Gatell, J. M., Azuaje, C., Llibre, J. M., Aranda, M., Barrufet, P., Martinez-Lacasa, J., Podzamczer, D., & COMBINE Study Team. (2004). Health-related quality of life in HIV-infected naive patients treated with nelfinavir or nevirapine associated with ZDV/3TC (the COMBINE-QoL substudy). HIV Clinical Trials, 5(3), 132–139.
Badia, X., Podzamczer, D., Moral, I., Roset, M., Arnaiz, J. A., Lonca, M., Casiro, A., Roson, B., Gatell, J. M., & BestQol Study Group. (2004). Health-related quality of life in HIV patients switching to twice-daily indinavir/ritonavir regimen or continuing with three-times-daily indinavir-based therapy. Antiviral Therapy, 9(6), 979–985.
Hicks, C. B., Cahn, P., Cooper, D. A. et al. (2006). Durable efficacy of tipranavir-ritonavir in combination with an optimised background regimen of antiretroviral drugs for treatment-experienced HIV-1-infected patients at 48 weeks in the randomized evaluation of strategic intervention in multi-drug reSistant patients with tipranavir (RESIST) studies: An analysis of combined data from two randomised open-label trials. Lancet, 36, 466–475.
Revicki, D. A., Sorensen, S., & Wu, A. W. (1998). Reliability and validity of physical and mental health summary scores from the Medical Outcomes Study HIV Health Survey. Medical Care, 38, 126–137.
Wu, A. W., Revicki, D. A., Jacobson, D., & Malitz, F. E. (1997). Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV). Quality of Life Research, 6, 481–493.
Heyting, A., Tolboom, J., & Essers, J. (1992). Statistical handling of dropouts in longitudinal clinical trials. Statistics in Medicine, 11, 2043–2061.
Lavori, P. W., Dawson, R., & Shera, D. (1995). A multiple imputation strategy for clinical trials with truncation of patient data. Statistics in Medicine, 14, 1913–1925.
Mallinckrodt, C. H., Clairk, W. S., Carroll, R. J., & Molenberghs, G. (2003a). Assessing response profiles from incomplete longitudinal clinical trial data under regulatory considerations. Journal of Biopharmaceutical Statistics, 13, 179–190.
Mallinckrodt, C. H., Sanger, T. M., Dube, S., Debrota, D. J., Molenberghs, G., Carroll, R. J., Zeigler Potter, W. M., & Tollefson, G. D. (2003b). Assessing and interpreting treatment effects in longitudinal clinical trials with missing data. Biological Psychiatry, 53, 754–760.
Siddiqui, O., & Ali, M. W. (1998). A comparison of the random-effects pattern mixture model with last observation carried forward (LOCF) analysis in longitudinal clinical trials with dropouts, Journal of Biopharmaceutical Statistics, 8, 545–563.
Laird, N. M., & Ware, J. H. (1982). Random effects models for longitudinal data. Biometrics, 38, 963–974.
Schluchter, M. D. (1992). Methods for the analysis of informatively censored longitudinal data. Statistics in Medicine, 11, 1861–1870.
DeGruttola, V., & Tu, X. M. (1994). Modeling progression of CD4-lymphocyte count and its relationship to survival time. Biometrics, 50(4), 1003–1014.
Rubin, D. B. (1976). Inference and missing data. Biometrika, 63, 581–592.
Rubin, D. B., & Schenker, N. (1986). Multiple imputation for interval estimation from simple random samples with ignorable nonresponse. Journal of the American Statistical Association, 81, 366–374.
Schafer, J. L. (1997). Analysis of incomplete multivariate data. Chapman and Hall, London.
Tanner, M. A., & Wong, W. H. (1987). The calculation of posterior distributions by data augmentation (with discussion). Journal of the American Statistical Association, 82, 528–550.
Thijs, H., Molenberghs, G., Michiels, B., Verbeke, G., & Curran, D. (2002). Strategies to fit pattern-mixture models, Biostatistics, 3, 245–265.
Dempster, A. P., & Rubin, D. B. (1983). Overview. In W. G. Madow, I. Olkin, & D. B. Rubin (Eds.), Incomplete data in sample surveys (Vol. II). Theory and annotated bibliography. New York: Academic Press (pp. 3–10).
Vonesh, E. F., Green, T., & Schluchter, M. D. (2006) Shared parameter models for the joint analysis of longitudinal data and event times. Statistics in Medicine, 25, 143–163.
Guo, X., Carlin, B. P. (2004). Separate and joint modeling of longitudinal and event time data using standard computer packages. The American Statistician, 58, 16–24.
Acknowledgments
We especially thank all the participants in the two trials. We also thank Dietmar Neubacher and Pek-Ju Hu of Boehringer Ingelheim for assistance in obtaining the trial data used for this analysis. Funding for this study was provided by Boehringer Ingelheim GmbH, Germany
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
-
Endpoint models: Last change score:
$$ (Y_{{{\text{ij}}}} - Y_{{{\text{i0}}}} ) = \beta _{0} + \beta _{1} TRT + \varepsilon _{{\text{i}}} $$where \( \varepsilon_{{\text{i}}} \,\sim\, N (0,\sigma ^{2} ) \) Y i0 is the baseline score and Y ij is the 48-week or last observed score for the ith patient.
TRT = 1 if treatment A, 0 otherwise.
-
Repeated measures models: Repeated change scores:
$$ (Y_{{{\text{ij}}}} - Y_{{i0}} ) = \beta _{{{\text{0j}}}} + \beta _{{{\text{1j}}}} TRT + \varepsilon _{{{\text{ij}}}} , $$where \( \varepsilon _{{{\text{ij}}}} \,\sim\,{}N(0,\Upsigma ) \)
Y i0 is the baseline score and Y ij is the observed score at the j = 8, 16, 24, 40, and 48 week assessment for the ith patient.
TRT = 1 if treatment A, 0 otherwise.
-
Growth curve models (piecewise linear models with knots at 8 and 16 weeks): Scores:
$$ Y_{{{\text{ij}}}} = \beta _{0} + \beta _{1} WEEK_{{{\text{ij}}}} + \beta _{2} WEEK_{{{\text{ij}}}} ^{ * } TRT + \beta _{3} WEEK8_{{{\text{ij}}}} + \beta _{4} WEEK8_{{{\text{ij}}}} ^{ * } TRT + \beta _{5} WEEK16_{{{\text{ij}}}} + \beta _{6} WEEK16_{{{\text{ij}}}} ^{ * } TRT + \varepsilon _{{{\text{ij}}}} $$where ε ij ∼ N(0, Z ij DZ ij + σ 2 I), Zij = (1 WEEKij) and D is the variance of the random effects.
Y ij is the observed score at the j = 8, 16, 24, 40, and 48 week assessment for the ith patient.
WEEKij is time from randomization to the jth MOS-HIV assessment
WEEK8ij = max(WEEKij − 8, 0); WEEK16ij = max(WEEKij − 16, 0);
TRT = 1 if treatment A, 0 otherwise.
-
Joint model:
$$ \begin{array}{*{20}c} {{Y_{{{\text{ij}}}} = X_{{{\text{ij}}}} \beta + Z_{{{\text{ij}}}} d_{{\text{i}}} + \varepsilon _{{{\text{ij}}}} }} \\ {{T_{{\text{i}}} = M_{{\text{i}}} \mu + r_{{\text{i}}} }} \\ \end{array} ,{\left[ {\begin{array}{*{20}c} {{d_{{\text{i}}} }} \\ {{r_{{\text{i}}} }} \\ {{\varepsilon _{{{\text{ij}}}} }} \\ \end{array} } \right]} \approx N{\left[ {{\left( {\begin{array}{*{20}c} {0} \\ {0} \\ {0} \\ \end{array} } \right)},{\left( {\begin{array}{*{20}c} {D} & {{\sigma ^{'}_{{{\text{dt}}}} }} & {0} \\ {{\sigma _{{{\text{dt}}}} }} & {{\sigma ^{2}_{{\text{t}}} }} & {0} \\ {0} & {0} & {{\sigma ^{2}_{{\text{e}}} }} \\ \end{array} } \right)}} \right]} $$where T i is the log time to the last MOS-HIV assessment.
Rights and permissions
About this article
Cite this article
Fairclough, D.L., Thijs, H., Huang, IC. et al. Handling missing quality of life data in HIV clinical trials: what is practical?. Qual Life Res 17, 61–73 (2008). https://doi.org/10.1007/s11136-007-9284-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-007-9284-3