Abstract
Demographic aging puts social insurance systems under immense pressure as frailty risks increase with age. The statutory long-term care insurance in Germany (GPV), whose society has been aging for decades due to low fertility and decreasing mortality, faces massive future pressure. The present study presents a stochastic outlook on long-term care insurance in Germany until 2045 by forecasting the future number of frail persons who could claim insurance services by severity level with theory-based Monte Carlo simulations. The simulations result in credible intervals for age-, sex- and severity-specific care rates as well as the numbers of persons for all combinations of age, sex and severity by definition of the GPV on an annual basis. The model accounts for demographic trends through time series analysis and considers all realistic epidemiological developments by simulation. The study shows that increases in the general prevalence of disabilities, especially for severe disabilities, caused by the demographic development in Germany are unavoidable, whereas the influence of changes in age-specific care risks does not affect the outcome significantly. The results may serve as a basis for estimating the future demand for care nurses and the financial expenses of the GPV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Demographic aging is a phenomenon affecting many industrialized societies. Decreasing mortality risk ceteris paribus (c.p.) leads to a larger share of the population in the old-age group (European Union 2017: 25; Vanella 2017: 550) and consequently to an overall higher number of people in need of care, since frailty risks increase with age (see, e.g., Fuino and Wagner 2018a: 56–57; Kochskämper 2018: 9). As a result, the financial long-term sustainability of care systems is in danger (Majeed and Khan 2019: 183–184; Nguyen et al. 2019: 132; Fuino and Wagner 2020: 151–152).
However, empirical studies investigating the trends in frailty and dementia are very scarce, and thus far, almost no studies have analyzed long-term frailty trends. Nevertheless, projections of the future number of frail persons are of immense value for estimating the future demand for nursery home or ambulant care (Bowles 2015: 94–99). Due to the lack of reliable and consistent data, little research has been conducted on the outlook of persons in need of care based on sound statistical grounds. Moreover, past deterministic projections rely on relatively strong assumptions on morbidity risks and demographic development and do not sufficiently quantify future uncertainty. Different trajectories are commonly based on varying assumptions of the connection between increasing life expectancy and the development of care risks (see Kochskämper 2018: 12–14, among others). Taking Germany as an example, we propose a new and innovative method to project the number of persons in need of care. Germany presents an interesting case study because its population is aging quite rapidly, as is the case for most countries in Europe (United Nations 2019). As the largest country in Europe, Germany deserves investigation.
Statutory long-term care insurance in Germany (GPV) is a special case and is considered a role model in this regard by a group of other European countries (Wild 2010: 13–14). It was introduced in 1995 as a response to the expected future increase in demand for long-term care (Bowles 2015: 189–193). The GPV is organized as a pay-as-you-go social insurance with only partial coverage and is financed by social contributions that amount to 3.05% of the income, of which half is paid by the employer and half by the employeeFootnote 1 (Klie 2005: 39). Services are provided to insured persons who are in need of care as ascertained by official medical personal. In addition, it evaluates how high the demand for care is, which then determines how high the benefits are (Klie 2005: 124). Initially, the amount of care–and, thus, the benefits–were categorized into four care levels (Pflegestufen): I, II, III and level III with hardship. In 2013, care level 0 was added for persons with no physical limitations who suffered dementia or another major mental illness. The decision of whether a person was “officially” in need of care and the allocation to the care level was mainly based on physical limitations in activities of daily living (Richter 2017: 98). These were assessed in four areas: personal hygiene (e.g., showering, brushing teeth, food preparation and consumption (cooking, eating food)), mobility (e.g., using stairs, getting up from bed) and domestic tasks (e.g., groceries, cleaning). The more limited a person is in these four areas, the higher the care level.
In 2016, the Zweites Pflegestärkungsgesetz (PSG II) was introduced. This law significantly changed the definition of the need for care. The major innovation was the acceptance of dementia as a health state qualifying for insurance benefits. Dementia had not been captured in care data bases before 2013. The definition of the severity of frailty has been changed from care levels 0, I, II, III and level III with hardship to “care degrees” (Pflegegrade) 1–5. Allocation to the care degrees is based on the time the caring activity takes. The time is assessed in six areas: mobility (e.g., using stairs, getting up from bed), ability to communicate (e.g., understanding, orientation), psychological problems (e.g., anxiety, aggressive behavior), self-supply (e.g., preparing food, washing), ability to cope with tasks stemming from sickness and disability (e.g., intake of medication, communication with medical staff) and ability to structure daily routine (e.g., initiating contacts with other persons). This reform has obviously led to a structural break in the data, creating difficulties in identifying the long-term trends in the severity of frailty based on its legal definition.
The present study simulates long-term trends in age- and sex-specific care risks by severity type. We use the Pflegestatistik from the micro census for 2017 in combination with population data to quantify the care rates. The age-, sex-, and severity-specific care rates until 2045 are projected by Monte Carlo simulation of Wiener processes, and the uncertainty in the projections is addressed and illustrated via credible intervals (CIs). Thus far, there exists only one stochastic study on the outlook of the GPV (see Sect. 2.3). Otherwise, all studies have been conducted deterministically and therefore have some limitations. First, deterministic projections impose rather hard assumptions about future development. From a statistical point of view, respective trajectories are highly improbable (Keilman et al. 2002: 410). Second, the analysis is limited to a rather small number of scenarios (see, e.g., Rothgang and Schmähl 1995) that do not sufficiently consider the future uncertainty. Third, the specified scenarios are seldom quantified with the likelihood of occurring. Fourth, the projections are not necessarily rooted in statistical data but rather in the judgments of a limited number of experts. These judgments tend to be rather subjective and therefore have some bias because of the personal opinions of the persons interviewed. Even good experts tend to perform worse on judgment-based forecasting than on forecasts that are conducted on solid statistical ground. Moreover, even when experts have good ideas about realistic future developments, they experience difficulties in translating their subjective assessments into probabilities (Lee 1998: 156–170). Furthermore, there is no previous study that projects the future numbers of disabled persons by the new definition of care degrees. Our study addresses both limitations in the literature simultaneously, filling a significant gap.
Based on our results, the future financial outlook of the GPV and the demand for care may be derived, among further applications. The remainder of the paper has the following structure: The next section provides an overview of previous studies on the link between mortality risks and morbidity risks, with an emphasis on disabilities and dementia. Moreover, some important past projection studies for the GPV are presented. Section 3 presents the underlying data and proposes a stochastic forecast model that is based on age-, sex- and severity-specific care rates (ASSSCRs), which results in a probabilistic projection of the number of care recipients until 2045. A selection of the model results is then presented in Sect. 4 before we conclude with a discussion of our paper and an outlook for future potential research.
2 Literature review
2.1 Approaches to estimating the connection of disability to mortality risk
There is an ongoing discussion on the impact of mortality changes on morbidityFootnote 2 and how to merge the two concepts to forecast morbidity based on forecasts of mortality. An early approach was proposed by Sullivan (1971: 351), who split life expectancy into healthy and disabled life expectancy.
Since the late 1970s, two theories have been dominant in the discussion. The first is the so-called expansion thesis, originally formulated by Gruenberg in 1977. He hypothesized that medical advances led to an extension of life with disabilities or chronic diseases (Gruenberg 2005: 781). Under this premise, an increase in life expectancy is associated with an increased portion of the lifetime spent with sickness or disability,Footnote 3 while the time lived in full health is unaffected.
The second extreme hypothesis is the compression thesis by Fries (1980: 132–134). Fries stated that factors such as improved nutrition, better hygiene and advanced medical treatment led to a decrease of acute illness and concluded that the life span in disability could be compressed into a time span before death (Fries 1980: 132–134). The consequence is that increases in life expectancy are associated with a pure gain in healthy life expectancy, whereas the portion of life spent with sickness or disability remains constant.
Many studies have tried to find statistical evidence for one theory or the other and have produced ambiguous results. Schoeni et al. point out that these studies rely on very limited data comprising extremely short time series and therefore might reach incorrect conclusions. The authors provide evidence for a positive effect of decreasing mortality on frailty with a combination of graphical and statistical analysis for a cohort study of people over age 75 in the United States using a synthetic dataset derived from various surveys (Schoeni et al. 2001: S206–S216). Manton et al. (2006) use multiple American survey datasets for a projection study of life expectancy and active life expectancy following the Sullivan method. The data provide some evidence that an increasing life expectancy expands the healthy life expectancy but not on a one-to-one basis; this suggests that the real connection between mortality and disability lies between the two fundamental hypotheses.Footnote 4 Perenboom et al. (2004) show positive trends for years lived with disability overall and increasing life expectancy for the Netherlands. Their closer analysis of disability trends separated by disability severity shows strong increases for lower severity, whereas more severe disability rates tend to decrease with higher life expectancy. Lin et al. (2012) conduct an age-period-cohort analysis of American survey data on limitations in performing activities of daily living (ADL) and instrumental activities of daily living (IADL) over the 1982–2009 period. They show a clear age trend in the probabilities of heavier ADL disabilities as well as lighter IADL disabilities, which is unsurprising. Moreover, the period trends are mostly negative until the end of the last millennium. Since then, IADL have stagnated, whereas there is no clear trend for ADL. This result shows shrinking probabilities for lighter disabilities over the time horizon, whereas heavier disabilities do not seem to be affected. The cohort trends are negative for both disability types.
The World Health Organization (WHO) applies Sullivan’s method for calculating life expectancy and health-adjusted life expectancy (HALE) for its member countries. The WHO reports a clear positive correlation between life expectancy and HALE, but the correlation coefficient is smaller than one (Mathers and Ho 2014: 10–14). This gives evidence that in reality, neither the expansion nor the compression theses hold completely. Increases in life expectancy appear to cause increases in healthy as well as unhealthy life expectancy.
The presented studies show that there is still no clear understanding of the real connection between decreasing mortality rates at high ages and frailty risks. This lack of understanding stems from different definitions of disability and limitations in the data and methodology used to date. The slight tendency seems to give the most evidence in support of the dynamic equilibrium hypothesis. Based on the evidence from the literature, we assume that the connection between mortality and morbidity trends to be stochastic, which will be covered via Monte Carlo simulation. This is explained further in Sect. 3 of this study.
2.2 Studies on the link between trends in mortality and dementia
Since the restructuring of the GPV in 2016, dementia has been defined as a disabling state; this designation allows individuals affected by dementia to receive financial compensation for care (Wingenfeld 2017: 39–46). Thus, a forecast of the future financial burden on the GPV needs to take the future development of dementia into account. Similar to the link between classical disabilities and morbidities, the connection between changes in mortality and the risk for dementia must be assessed. Since most studies either do not investigate time trends in dementia or are rather underwhelming methodologically,Footnote 5 a gap in the literature exists. Manton et al. (2005) pooled American survey data on persons aged 65 and older for 1982–1999 and found some evidence for decreasing c.p. trends in severe cognitive impairment. A major limitation of that study is that age is not given in years but rather is split into two age groups: persons aged 65–79 and persons over 79. Therefore, there might be some bias due to the age group structure of the sample. Nevertheless, the results appear plausible.
Satizabal et al. (2016) conducted a more advanced study using panel data to compare four five-year cohorts by their age-specific incidence of dementia and calculating hazard ratios while also considering educational level. They confirmed the results of Manton et al. (2005) but found that the differences in dementia risk were statistically significant only for persons with higher education.Footnote 6 The study implies that an overall decline in age-specific dementia risk does exist but is caused by increases in education rather than by pure increases in life expectancy.Footnote 7
Wu et al. (2014) conducted a review of 70 studies about the age- and sex-specific prevalence of dementia in China, Hong Kong and Taiwan over the period 1980–2012, and they pooled these results to estimate the possible effects of age-, period-, and cohort-effects on this prevalence. In addition to observing the obvious age effect, they concluded that there was a possible cohort effect on dementia, stemming from common life circumstances for the specified cohorts, whereas they did not identify a period effect on dementia. Thus, they could not conclude that there was a general effect of higher life expectancy on the risk of dementia. In a follow-up paper, Wu et al. (2015) conducted another review of international studies on the prevalence of dementia. They concluded that the effect of increasing life expectancy on the age-specific prevalence of dementia strongly depended on the development level of the country and its population. The authors’ observation suggested that countries with a heavily expanding life expectancy, mediocre education, and a weak understanding of healthy lifestyles likely have unhealthy conditions with higher risk of mental disorders. In contrast, countries that already have a very high life expectancy that increases at a lower rate are associated with a very high degree of development. This leads to higher education and a healthier lifestyle, resulting in increases in healthy life expectancy, as expected by the compression thesis. The authors include the Western and Northern countries as well as North America in the latter category. Fastame et al. (2015: 2159–2161) confirmed the mitigating effect of high education on the risk of cognitive disorders in an experimental setting.
The presented studies show no clear evidence for a direct connection between life expectancy and dementia, and long-term studies are basically non-existent, especially for Germany (Ziegler and Doblhammer 2010: 96). We implicitly model trends in dementia within our probabilistic projection of care rates.
2.3 Projections of demand for long-term care in Germany
Projections of the future demand for long-term care and long-term care insurance in Germany have thus far been conducted almost exclusively by deterministic modeling.
The first projection on the future outlook of the GPV was conducted by Rothgang and Schmähl (1995), who estimated the number of persons in need of care in Germany until the year 2030 directly after the installment of the GPV using the 7th coordinated population projection of the German federal statistical office (Destatis) as the assumed future population. The authors applied age- and sex-specific care risks extracted from a series of survey studies by Infratest (1992, 1993) as well as Krug and Reh (1992). Assuming that 90% of frail persons were covered by the GPV and using three scenarios of claim behavior regarding cash and service transfers, the possible financial expenditure of the GPV was estimated given the regulations on financial benefits. Rothgang and Vogler (1997) elaborated on that approach by adding sensitivity analysis of three scenarios of realistic future population development with different assumptions on migration and mortality. The future development of mortality was estimated using the model by Bomsdorf and Trimborn (1992). Rothgang (2001) developed that approach further using data on GPV beneficiaries from the Pflegestatistik, which was introduced in 1999. In that study, he added further scenarios addressing the future trends in morbidity and the type of care services claimed by persons in need of care. For morbidity, he added a scenario in which the dynamic equilibrium thesis held to the baseline scenario of constant care risks. For each scenario, he multiplied the number of beneficiaries by type of service and severity of disability with the respective costs to estimate the future outlook of the GPV.
Blinkert and Klie (2001) projected the number of persons in need of care based on persons claiming nursing home or domiciliary care services along with future informal care potentialFootnote 8 until 2050 under four different scenarios. The analysis considered demographic development and trends in family networks and in the labor market, especially female labor market participation. Based on their results, the authors derived the potential demand on the labor market for caregivers, as well.
Bowles (2015) proposed a detailed model for simulating the financial demand placed on the GPV until 2080. He stressed that this was not a forecast but rather a demonstration of possible scenarios for the future outlook of the GPV. He projected the population by sex and age under certain assumptions regarding fertility, migration, and mortality. Moreover, he used data from federal health reporting provided by the Robert Koch Institute (RKI) and Destatis on recipients of services in long-term care for 2011 detailed by sex, age group, level of disability (I; II; III), and type of care (domiciliary or stationary) on December 31, 2011, as well as age- and sex-specific population estimates by Destatis for that very same day for calculating care rates differentiated by the mentioned criteria. These rates were then multiplied by the projected population, similar to the method proposed by Rothgang and Schmähl, to simulate the future population in need of care by sex, age, degree of disability, and type of received care through 2080. Future uncertainty was considered to some degree by scenario analyses measuring the sensitivity to changes in the input variables. Mortality changes were included by projecting the future total life expectancy, which was split into healthy life expectancy and life expectancy in need of care, as proposed by Sullivan (1971: 351). Bowles’ approach separated disabled life expectancy into life expectancy in care levels I, II, or III. Regarding morbidity, three scenarios were considered. In baseline scenario 1, Bowles (2015: 151) assumed that the care risks remained constant at their 2011 level. In combination with the Sullivan model, this means that the increase in life expectancy affects only life expectancy under disability and not healthy life expectancy. Therefore, the baseline scenario represented the outcome in the event that the expansion thesis held. Scenario 2 assumed the compression of disabled life expectancy into the last years before death. Thus, increases in life expectancy translated into healthy life expectancy exclusively. Scenario 3 followed the premise that half of the growth in life expectancy would translate into healthy life expectancy, while the other half would be under disability. Finally, Bowles gave a financial outlook of the GPV under the simulated trajectories. To do so, the estimated numbers of age- and sex-specific persons in need of care were multiplied by historic rates of service claims from the GPV and then multiplied by the corresponding financial costs of these services. The simulations were then varied by alternate scenarios, as well.
The presented studies were all deterministic and thus were relatively inflexible and vulnerable to errors. Deterministic projections in general have the limitations of being based on rather strong assumptions and thus have a low individual probability of occurring in the future. Moreover, risk is considered only by scenario analyses, which offer a small number of alternate trajectories of the future and are generally not quantified probabilistically (Lee 1998: 165–167).
Bomsdorf et al. (2008) gave the only stochastic projection of the future number of frail persons in Germany by severity level. They estimated the future population based on the mortality model by Babel et al. (2008), the fertility model by Babel et al. (2006) and a stochastic model for net migration based on the Lee-Carter model for mortality (see Lee and Carter 1992). The authors calculated age- and sex-specific care risks by severity from the Pflegestatistik 1999–2005 and extrapolated the estimated trends into the future. In this way, Bomsdorf et al. (2008) simulated the number of people in need of care through 2050 by severity with 90% prediction intervals. This approach was quite sophisticated but is unfortunately not applicable due to the recent reform of the German care system.
Thus far, no studies have included the effects of PSG II in their future care projections. Our study not only gives a future outlook based on the current long-term care system but does so stochastically. We propose a stochastic model that to some degree builds on the approaches by Rothgang and Vogler (1997) and Bowles (2015).
3 Data and methods
3.1 Data
Our first objective is to simulate the long-term trends in care risks. In the first step, we estimate ASSSCRs. Although we have the care statistics data at hand, it is not feasible to use time series for estimating trends, since changes in legal regulations lead to structural breaks in the data (see introduction). In particular, the change from care levels (Pflegestufen–PS) to care degrees (Pflegegrade–PG) and the inclusion of the definition of dementia as a disability in the legal sense significantly change the number of people in need of care, thus clearly limiting the use of time series methods. To avoid such a structural break, we base our analysis on the care statistics of 2017 (RDC of the Federal Statistical Office and Statistical Offices of the Länder, Pflegestatistik, survey year 2017). The dataset covers all persons receiving benefits from the GPVFootnote 9 (who are thus officially assigned to a care degree) on December 15, 2017, by birth cohort, gender, care degree and type of service they receive, among other variables. The total number of persons in the dataset who can be identified by these criteria is approximately 3.41 million, with the moderate care degrees being more dominant. Among this total number, approximately 1.57 million persons have PG2, 1.02 million have PG3 and 0.55 million are in PG4. The extreme cases of PG5, with less than a quarter million persons, and PG1, with less than 50 thousand, are much less frequent. The data span all ages, with a median age of 81 years. Due to their higher life expectancy (Vanella 2017: 551) and their c.p. higher care risk (see Fig. 3), the share of females in the dataset is quite high at almost 63%. The microdata are cumulated to serve as counts of age-, sex-, and severity-specific care cases. We define age by year (cohort-based) for the age group 60–93. Cases aged 59 and younger are cumulated in one age group, since the care risks in this age group are relatively low and smoothing of the observed data can be prevented in this way. Theoretically, we can assume that care risk increases with age, or mathematically speaking, the curve should be monotonically increasing. This is not strictly the case in observed rates under 60 years, implying that there are stochastic residuals in the data for the year under study. The error arising from our pooling of this age group is negligible, since the overall care risk is small and the slope of the frailty curve over that age group is not steep. The 94+ age group is also cumulated, as the number of cases, especially for PG1, is too small to derive representative estimates for the associated care risks in these age groups from the data.
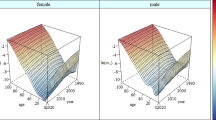
We estimate the ASSSCRs by dividing the specific cases by the corresponding population estimates, which have been downloaded from the Human Mortality Database (2019). The raw population data in the Human Mortality Database (HMD) originate from Destatis, but the published data at the HMD are of higher quality and are more detailed for the old-age population. The official population statistics are truncated above age 100 and are very susceptible to errors from the annual population update, as Scholz et al. (2018: 2–5) have shown. This stems from estimation errors in the census in addition to unregistered migration, which leads to relatively large errors for the old-age population, which is naturally smaller than the younger population. Therefore, estimation errors have a relatively larger impact on the estimates of mortality or disability risks. The HMD data are smoothed for the age group above 80 to account for these problems (Scholz et al. 2018: 4–5). Figure 1 illustrates the ASSSCRs in 2017 for Care Degrees 3, 4 and 5.

Sources: Human Mortality Database (2019); RDC of the Federal Statistical Office and Statistical Offices of the Länder, Pflegestatistik, survey year 2017; own calculation and design
Age- and sex-specific care rates for care degrees 5–3 in 2017.
Obviously, the age-specific care risk increases with increasing age, as one would expect. Figure 2 visualizes the prevalence of PG1 and PG2.

Sources: Human Mortality Database (2019); RDC of the Federal Statistical Office and Statistical Offices of the Länder, Pflegestatistik, survey year 2017; own calculation and design
Age- and sex-specific care rates for care degrees 2 and 1 in 2017.
In contrast, these “less severe” care risks show decreasing prevalence for the oldest people. This appears plausible, as in this age group, the worsening of already present frail conditions is probable and associated with the transition into a higher PG (Fuino and Wagner 2018a: 56–69, b: 329).
The ASSSCRs diverge after the eighth decade of life, with females’ risks becoming much larger than males’. This trend becomes even clearer considering the estimates of the overall care rates, which are the sums of the rates from Figs. 1 and 2 by sex and age, as illustrated in Fig. 3.

Sources: Human Mortality Database (2019); RDC of the Federal Statistical Office and Statistical Offices of the Länder, Pflegestatistik, survey year 2017; own calculation and design
Care rates in 2017 by age and sex.
This phenomenon is also observed in other investigations (e.g., Fuino and Wagner 2018a: 57; Kochskämper 2018: 9) and may be associated with the fact that the female partner in a married couple is commonly younger than the male partner (GENESIS-Online Datenbank 2019). Combined with the lower life expectancy of males in comparison to females (Vanella 2017: 550–552), we conclude that females in most cases survive their spouses. Thus, a male who becomes frail is often cared for by his spouse (Hank and Stuck 2008: 1288; Cheema 2013: 2406). This may lead to a tendency of underestimating care risks in the statistics, since it is realistic that not all persons giving informal care claim financial support for doing so. Those persons will not appear in the statistics. Since frailty for females often appears when they are already widows or their husbands are too old to care for them, women have a higher tendency to claim professional help (Destatis 2018a: 9). Moreover, on average, females have a higher c.p. life expectancy than males but tend to live under worse health than males at the same age, as other studies have shown (Nguyen et al. 2019: 137–140).
3.2 Methods
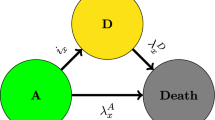
After having estimated the baseline data for our analysis, the forecast of the ASSSCRs is conducted. Due to the absence of valid time series on the ASSSCRs (see Sect. 1), we estimate the prevalence trends following the idea of the Sullivan method presented in Sect. 2. The literature overviewed in that section postulates a non-negative correlation between increases in life expectancy and increases in life expectancy with disability; however, the results of the studies do not give a conclusive picture of the real connection between the two variables. Nevertheless, some conclusions can be drawn from the literature. The two extreme hypotheses of expansion and compression give a plausible frame for a realistic connection. Moreover, much of the literature proposes that the two classical hypotheses do not fully apply; rather, some kind of dynamic equilibrium in between gives the real correlation between mortality and morbidity.
From these observations, our approach is inspired by a Bayesian approach to apply so-called non-informative prior distributions; i.e., we know little or nothing about the actual probabilities of certain outcomes or the true parameter, and we therefore do not impose heavy assumptions on the true distribution of the parameter (Lynch 2007: 55). Knowing that a decrease in mortality leads to some c.p. decrease in morbidity, we can assume that a decrease in the mortality risk by d % for males aged x in year y is associated with a decrease in the care risk for males in that very same age and year by 0% to d %. Generally speaking, the correlation coefficient between mortality risk m and care risk c for persons aged x years of gender g in year y is
with \(U\left( {0,1} \right)\) indicating a uniform distribution with minimum 0 and maximum 1 (Lynch 2007: 55). A uniform distribution with these limits states that the probability of the random variable taking a certain value in that interval is equal for all values. This is why the term non-informative is used frequently because there is no pre-defined modus for the distribution of the variable. Figure 4 presents the probability density function of \(\rho_{m,c,x,g,y}\) to illustrate this principle.
\(\rho_{m,c,x,g,y} = 0\) would signify no connection between the two variables; thus, increases in life expectancy (i.e., decreases in age-specific mortality rates) would not result in decreasing care rates, thus increasing the frail life expectancy. This scenario would follow the expansion thesis. In the other extreme scenario, a correlation coefficient of 1 would be associated with decreases in care rates according to mortality rates. Therefore, increases in life expectancy would be lived completely disability-free, following the compression thesis. Values between the two boundary values would represent some mixture of life expectancy in good and poor health, according to the dynamic equilibrium thesis. For the projection, 10,000 random numbers are drawn annually from a uniform distribution according to (1). These are taken as trajectories of the Sullivan parameter.
Age- and sex-specific mortality rates (ASSMRs) are simulated until 2045 according to Vanella’s (2017) version of the Lee-Carter model for both genders. The model proposes applying principal component analysis to the variance matrix of the time series of the logistically transformed age- and sex-specific survival rates of a collection of countries. Lee and Carter (1992: 662–663) used a similar approach to American mortality rates to show that the first principal component explains a large share of the mortality development because mortality improvements involve common factors such as advances in the understanding of hygiene (Pötzsch and Rößger 2015: 34) and medical technologies (World Health Organization 2015: 51). The entire population benefits from these improvements. Therefore, many have identified the approach as the Lee-Carter model. Vanella extended the Lee-Carter model by identifying the second principal component as some type of behavioral index that explains different mortality improvements between both genders to some extent (Vanella 2017: 547–548). Moreover, that study addressed the major limitation of the Lee-Carter model, which is the systematic underestimation of future uncertainty, resulting in overly narrow prediction intervals. Figure 5 presents the loadings of the first two principal components, which can be interpreted as the correlation coefficients between the ASSSRs and the respective principal component.
Parametric functions are fit by OLS to the time series of these two principal components to estimate their long-term trends. Autoregressive Integrated Moving Average models present the remaining nuisance.Footnote 10 This procedure results in forecast models of the first two principal components, which are then simulated 10,000 times annually as Wiener processes to estimate 10,000 trajectories for their future development. The theoretical mean forecasts with 90% prediction intervals for the two principal components until 2045 are illustrated in Fig. 6.
The forecast in the mean shows a decreasing overall mortality trend (the Lee-Carter Index is negatively correlated to the ASSSRs, and thus decreases in it mean increases in the ASSSRs) and a convergence of male ASSSRs to female ones, although this connection is highly stochastic, as the width and direction of the prediction interval indicate.Footnote 11 The remaining principal components are assumed random walk processes and simulated as such. The resulting 10,000 trajectories of all principal components are then transformed back into 10,000 trajectories of the logit-ASSSRs and finally ASSSRs.
From these trajectories, the relative change in some ASSMR in trajectory t can be computed:
From (1) and (2) follows the relative change in the ASSSCRs in year y in trajectory t and with PG p:
from which the ASSSCRs in trajectory t in year y
result.
The ASSSCRs are then multiplied with the trajectories of a probabilistic age and sex-specific population forecast for Germany generated based on a stochastic cohort-component algorithm proposed by Vanella and Deschermeier (2020). In this way, we derive stochastic age-, sex- and severity-specific care numbers by 2045:
with \(N_{x,g,p,y,t}\) being the number of persons in care aged x years of sex g with care degree p at the end of year y in trajectory t and \(B_{x,g,y,t}\) being the population in Germany of persons of the same age and sex in the same year and trajectory.
The results of our analysis are reported in Sect. 4.
4 Results
Following (2), the simulated ASSMRs are used to compute 10,000 trajectories of the future relative change in the ASSMRs. The median trajectories for a selection of years are given in “Appendix A”. These trajectories are then multiplied with 10,000 random draws from a uniform distributed density for \(\rho\), as explained in (3). The relative change in the ASSSCRs simulated in this way is then plugged into (4) to derive the corresponding ASSCRs in that period. This process is then reiterated annually, starting with the baseline year 2017. In this way, we derive 10,000 trajectories of each ASSSCR in each year until 2045, the end of the forecast horizon. These trajectories can be used to estimate CIsFootnote 12 for every variable non-parametrically. Because of the magnitude of the results, we present only a small portion of the results here.
“Appendix B” compares the ASSSCRs in 2017 to their respective median trajectories and the estimated 90% CIs in 2045.Footnote 13 Basically, small overall improvements in age-specific care risks can be expected due to improvements in mortality. Due to realistic increases in ASSMRs, the ASSSCRs might also increase in the future, although decreasing risks are more probable. Figure 7 illustrates the estimated overall care rates (i.e., the sums of all age–specific care rates over all care degrees) by sex as observed in the data for 2017 compared to the median trajectory with 90% CIs in 2045.
While overall frailty risk remains almost constant for the younger ages (i.e., under age 70), slight decreases are probable until approximately age 90, as further improvements in mortality are likely to be reached by this age group. As mortality trends for the oldest persons in the past do not show clear trends, the ASSMRs in the mean and the median will not change much in the future. In general, we see broadening CIs with increasing age, representing higher uncertainty with regard to future development.
In addition to the development of age-specific care prevalence, the overall development of the size and age structure of the population is another important determinant of overall frailty prevalence. Vanella and Deschermeier (2020) conducted a probabilistic forecast of the age- and sex-specific population in Germany until 2045. We borrow their results for our study. A slight increase in the population size to almost 85 million persons by 2040 is predicted in the median. Even more important than the population size is the age structure of the population. For both genders, we observe an almost certain increase in the population size from age 70 onwards, which is the age group in which the risk of being in need of care starts to increase significantly, as illustrated in Fig. 7. “Appendix C” gives the forecast of the sizes of two old-age groups to illustrate the increase in the population size in these age groups, which are very susceptible to care risks.
Multiplying the 10,000 annual trajectories for the age- and sex-specific population provided by Vanella and Deschermeier (2020) with the 10,000 trajectories for the ASSSCRs estimated by us, we follow (5) and derive 10,000 trajectories of the number of persons claiming care services by age (−59,60,…,93,94+), sex and care degree. Figures 8 and 9 illustrate the future development of the number of persons claiming care insurance services by care degree, without discriminating by sex and age, with 90% CIs.
The number of persons in PG1 is rather negligible, whereas the number of persons in PG2, PG3 and PG4 will increase significantly, as given in Table 1.
The increase in PG5 is not as strong. This can be explained first by the overall smaller risk of being classified into PG5 rather than into a less severe state. Second, we see from “Appendix B” that the risk of suffering from severe disability after age 80 increases strongly. Since the size of the population decreases heavily at that point, the part of the population at severe risk of these kinds of disabilities is rather small. Hence, the resulting number of persons in PG5 remains relatively small.
5 Discussion and outlook
The present study showed the effect of future demographic development in Germany on the number of frail persons claiming services from the GPV. Due to the aging process, we expect these numbers to increase heavily until 2045, especially for the moderately severe care degrees 2–4, with no mitigation of this trend in sight. This development implies large increases in the financial pressure on the GPV and in the demand for nurses to care for those in need. Furthermore, this development will probably strain the possibilities of reconciling work and care for many employed caregivers, as approximately 70 percent of caring in Germany is done in families (Ehrlich et al. 2019: 1)
Using theory-based Monte Carlo simulation, we estimated median trajectories for the future number of persons claiming benefits of the GPV by severity of disability, and we derived 90% CIs. We thus provide a realistic frame for future development as a sound basis for future planning in politics and business.
When interpreting the results of our study, limitations must be acknowledged. The definition of severity in the framework of insurance changed significantly in 2016 with the change from care levels to care degrees and the inclusion of dementia in the specification of disability severity. As statistics before 2013 did not include measurements of dementia and the new care degree 1 has no predecessor, it is not possible to construct valid time series for the care prevalence in Germany. Therefore, it is not possible to estimate autocorrelations for the time series or cross-correlations among the time series of the various prevalence rates, making more sophisticated analyses not yet feasible. Hence, we had to make simplifying assumptions based on the theoretical connection between mortality and morbidity. Future studies should be able to address this issue better when time series for the problem under study are available. We stress that the intervals presented in our study cannot account for the correlations mentioned above to the full extent; therefore, we labeled them “credible intervals” instead of the more common term “prediction intervals”. Moreover, the reader should keep in mind that our study exclusively covers persons receiving care insurance benefits. Therefore, we might underestimate the total prevalence in the population to some degree, as persons who have claimed services but have not been assigned a specific care degree are not included in the study. Moreover, some persons might be frail but do not claim services, as their family members care for them without receiving any compensation for doing so. Finally, long-term care policies in Germany are undergoing several reforms currently, and thus, the institutional framework and regulations of who is official defined of being in the need of care might change yet again.
However, our study provides an informative and detailed outlook from which scientific as well as societal implications can be drawn. Based on our results, further studies regarding the future demand for care nurses and the financial expenses of long-term care insurance in Germany should be conducted. In addition, our methodological approach could be applied to other countries with comparable long-term care systems. From a societal perspective, policy makers, employers, trade-unions, providers of long-term care and other stakeholders must acknowledge the challenges stemming from the extremely likely increasing need for professional care nurses and financial expenses for the GPV. They have to develop strategies and measures on the national, regional and local level to tackle these challenges.
Change history
13 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11135-021-01248-x
Notes
There are some exceptions: self-employed people and pensioners pay the full 3.05% themselves, and those without children pay an additional contribution of 0.25% (Richter 2017, 17).
A disability is a limiting health condition of either physical or mental nature (CDC 2019). Therefore, being disabled always means being morbid, whereas morbidity is not necessarily connected to disability.
This case is also known as dynamic equilibrium (Crimmins and Beltrán-Sánchez 2010: 75–76).
See Prince et al. (2015: 13–15) on this.
Defined by having received a high school diploma.
There is strong evidence for higher education leading to higher c.p. life expectancy, as well (Meara et al. 2008: 354).
Persons who provide home care services, identified from the personal networks of care recipients.
Including persons living abroad.
We recommend Shumway and Stoffer (2016: 77–137) for further reading on this model family.
For more details on the interpretation of the index and its forecast, see Vanella (2017: 547–552).
We refer to CIs as in Bayesian statistics rather than using the common term prediction intervals from frequentist statistics. In doing so, we stress that the uncertainty in care risk is not derived from time series data but rather estimated from theory. Therefore, we find the presented intervals “credible” based on our analysis while not knowing the real intervals.
This is not done graphically, since the differences are quite small and would be difficult to identify in a graphical representation.
References
Babel, B., Bomsdorf, R., Schmidt, R.: Future trends and dynamics of the occurrence of Down’s Syndrome and Still-births. Discussion papers in statistics and econometrics 03/06. Köln: University of Cologne, Faculty of Management, Economics and Social Sciences, Institute of Econometrics and Statistics (2006)
Babel, B., Bomsdorf, E., Schmidt, R.: Forecasting German mortality using panel data procedures. J. Popul. Econ. 21(3), 541–555 (2008)
Blinkert, B., Klie, T.: Zukünftige Entwicklung des Verhältnisses von professioneller und häuslicher Pflege bei differierenden Arrangements und privaten Ressourcen bis zum Jahr 2050. Expertise im Auftrag der Enquéte-Kommission Demographischer Wandel des Deutschen Bundestages. Albert-Ludwigs-Universität Freiburg, Institut für Soziologie, Freiburg (2001)
Bomsdorf, E., Babel, B., Schmidt, R.: Zur Entwicklung der Bevölkerung, der Anzahl der Schüler, der Studienanfänger und der Pflegebedürftigen. Sozialer Fortschritt [German Review of Social Policy] 10(5), 125–132 (2008)
Bomsdorf, E., Trimborn, M.: Sterbetafel 2000. Modellrechnungen der Sterbetafel. German J. Risk Insur. 81(3), 457–485 (1992)
Bowles, D.: Finanzentwicklung der sozialen Pflegeversicherung. Modellrechnungen unter Berücksichtigung demografischer, ökonomischer, gesundheitlicher und sozialrechtlicher Rahmenbedingungen. Baden-Baden: Nomos Verlagsgesellschaft (2015)
CDC: Principles of epidemiology in public health practice. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office of Workforce and Career Development (2012)
Cheema, A.N.: Upcoming picture of ageing population: Pakistan. Qual Quant Int. J. Methodol. 47(5), 2399–2413 (2013)
Crimmins, E.M., Beltrán-Sánchez, H.: Mortality and morbidity trends: Is there compression of morbidity? J. Gerontol. Soc. Sci. 66B(1), 75–86 (2010)
Destatis: Pflegestatistik 2017. Pflege im Rahmen der Pflegeversicherung. Deutschlandergebnisse. Wiesbaden: Statistisches Bundesamt (2018a)
Destatis: S 09 Gestorbene 2016 nach Alters- und Geburtsjahren. Data provided on 29 March 2018 (2018b)
Destatis: S 09 Gestorbene 2017 nach Alters- und Geburtsjahren. Data provided on 19 March 2019 (2019)
Ehrlich, U., Minkus, L., Heß, M.: Einkommensrisiko Pflege?. Zeitschrift für Gerontologie und Geriatrie. Der Zusammenhang von familiärer Pflege und Lohn. https://doi.org/10.1007/s00391-019-01666-5 (2019)
European Union: The 2018 ageing report. Underlying assumptions & projection methodologies. Publications Office of the European Union, Luxembourg (2017)
Fastame, M.C., Hitchcott, P.K., Penna, M.P.: Does education influence visuo-spatial and verbal immediate serial recall in healthy older adults? Qual. Quant. Int. J. Methodol. 49(5), 2155–2167 (2015)
Fries, J.F.: Aging, natural death, and the compression of morbidity. N. Eng. J. Med. 303(3), 130–135 (1980)
Fuino, M., Wagner, J.: Long-term care models and dependence probability tables by acuity level: new empirical evidence from Switzerland. Insur. Math. Econ. 81, 51–70 (2018a)
Fuino, M., Wagner, J.: Old-age care prevalence in Switzerland: drivers and future development. Eur. Actuar. J. 8(2), 321–362 (2018b)
Fuino, M., Wagner, J.: Duration of long-term care: socio-economic factors, type of care interactions and evolution. Insur. Math. Econ. 90, 151–168 (2020)
GENESIS-Online Datenbank: Eheschließungen: Deutschland, Jahre, Alter der Ehefrau, Alter des Ehemannes. https://www-genesis.destatis.de/genesis/online/data. Data Accessed 2 April 2019 (2019)
Gruenberg, E.M.: The failures of success. Milbank Q. 83(4), 779–800 (2005)
Hank, K., Stuck, S.: Volunteer Work, informal help, and care among the 50 + in Europe: Further evidence for ‘linked’ productive activities at older ages. Soc. Sci. Res. 37(4), 1280–1291 (2008)
Human Mortality Database: Germany, Population Size (abridged). University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). www.mortality.org or www.humanmortality.de. Accessed 7 July 2019 (2019)
Infratest: Hilfe- und Pflegebedarf in Deutschland. Schnellbericht zur Repräsentativerhebung im Rahmen des Forschungsprojekts “Möglichkeiten und Grenzen selbständiger Lebensführung.“ München: Bundesministerium für Familie und Senioren (1992)
Infratest: Hilfe- und Pflegebedarf in Deutschland. Endbericht zur Repräsentativerhebung im Rahmen des Forschungsprojekts “Möglichkeiten und Grenzen selbständiger Lebensführung.“ München: Bundesministerium für Familie und Senioren (1993)
Keilman, N., Dinh, Q.P., Hetland, A.: Why population forecasts should be probabilistic—llustrated by the case of Norway. Demogr. Res. 6(15), 409–454 (2002)
Klie, T.: Pflegeversicherung. Einführung, Lexikon, Gesetzestexte, Nebengesetze, Materialien. Vincentz Network, Hannover (2005)
Kochskämper, S.: Die Entwicklung der Pflegefallzahlen in den Bundesländern: Eine Simulation bis 2035. IW-Report 33/18 (2018)
Krug, W., Reh, G.: Pflegebedürftige in Heimen. Statistische Erhebungen und Ergebnisse. Kohlhammer, Stuttgart, Berlin (1992)
Lee, R.D.: Probabilistic approaches to population forecasting. Popul. Dev. Rev. 24, 156–190 (1998)
Lee, R.D., Carter, L.R.: Modeling and forecasting US mortality. J. Am. Stat. Assoc. 87(419), 659–671 (1992)
Lin, S.F., Beck, A.N., Finch, B.K., Hummer, R.A., Master, R.K.: Trends in US older adult disability: exploring age, period, and cohort effects. Am. J. Public Health 102(11), 2157–2163 (2012)
Lynch, S.M.: Introduction to applied bayesian statistics and estimation for social scientists. Springer Business + Media, New York (2007)
Majeed, M.T., Khan, F.N.: Do information and communication technologies (ICTs) contribute to health outcomes? An empirical analysis. Qual. Quant. Int. J. Methodol. 53(1), 183–206 (2019)
Manton, K.G., Gu, X.L., Lamb, V.L.: Long-term trends in life expectancy and active life expectancy in the United States. Popul. Dev. Rev. 32(1), 81–105 (2006)
Manton, K.G., Gu, X.L., Ukraintseva, S.V.: Declining prevalence of dementia in the U.S. elderly population. Uspechi Gerontologii 16(1), 30–37 (2005)
Mathers, C., Ho, J.: WHO methods for life expectancy and healthy life expectancy. Global Health Estimates Technical paper WHO/HIS/HIS/GHE/2014.5. Genève: World Health Organization, Department of Health Statistics and Information Systems (2014)
Meara, E.R., Richards, S., Cutler, D.M.: the gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff. 27(2), 350–360 (2008)
Nguyen, T.T., Le, N.B., Vu, L.H., Le, A.V.: Quality of life and its association among older people in rural Vietnam. Qual. Quant. Int. J. Methodol. 53(1), 131–141 (2019)
Perenboom, R.J.M., Van Herten, L.M., Boshuizen, H.C., Van Den Bos, G.A.M.: Trends in disability-free life expectancy. Disabil. Rehabil. 26(7), 377–386 (2004)
Pötzsch, O., Rößger, F.: Germany’s population by 2060: results of the 13th coordinated population projection. Destatis, Wiesbaden (2015)
Prince, M., Wimo, A., Guerchet, M., Ali, G.C., Wu, Y.T., Prina, M.: World Alzheimer report 2015. The global impact of dementia. An analysis of prevalence, incidence, cost and trends. Alzheimer’s Disease International, London (2015)
PSG II. Zweites Pflegestärkungsgesetz. Bundesgesetzblatt Teil I 2015, vol 54, pp. 2424–2463. Bonn: Bundesanzeiger Verlag (2015)
RDC of the Federal Statistical Office and Statistical Offices of the Länder, Pflegestatistik, survey year 2017. Accessed 22 August 2019. Hannover: Landesamt für Statistik Niedersachsen. https://doi.org/10.21242/22411.2017.00.00.1.1.0
Richter, R.: Die neue soziale Pflegeversicherung—PSG I, II und III: Pflegebegriff, Vergütungen, Potenziale. Nomos Verlagsgesellschaft, Baden-Baden (2017)
Rothgang, H.: Finanzwirtschaftliche und strukturelle Entwicklungen in der Pflegeversicherung bis 2040 und mögliche alternative Konzepte. Endbericht zu einer Expertise für die Enquete-Kommission „Demographischer Wandel“ des Deutschen Bundestags. Bremen: University of Bremen, Centre for Social Policy Research (2001)
Rothgang, H., Schmähl, W.: The long-term costs of public long-term care insurance in Germany. Some Guesstimates. ZeS-Arbeitspapier 9/95. Bremen: University of Bremen, Centre for Social Policy Research (1995)
Rothgang, H., Vogler, A.: Die zukünftige Entwicklung der Zahl der Pflegebedürftigen bis zum Jahre 2040 und ihre Einflußgrößen. ZeS-Arbeitspapier 06/1997. Bremen: University of Bremen, Centre for Social Policy Research (1997)
Satizabal, C.L., Beiser, A.S., Chouraki, V., Chêne, G., Dufouil, C., Seshadri, S.: Incidence of dementia over three decades in the framingham heart study. N. Engl. J. Med. 374(6), 523–532 (2016)
Schoeni, R.F., Freedman, V.A., Wallace, R.B.: Persistent, consistent, widespread, and robust? another look at recent trends in old-age disability. J. Gerontol. Soc. Sci. 56B(4), S206–S218 (2001)
Scholz, R., Jdanov, D., Kibele, E., Grigoriev, P., Klüsener, S.: About mortality data for Germany. Retrieved from the HMD webpage at https://www.mortality.org/hmd/DEUTNP/InputDB/DEUTNPcom.pdf. Accessed 4 December 2018 (2018)
Schröder, E., Würtz, S.: Bacteria. In: Mara, D., Horan, N. (eds.) The handbook of water and wastewater microbiology, pp. 57–68. Elsevier, London (2003)
Shumway, R.H., Stoffer, D.S.: Time series analysis and ist applications. With R examples. Springer International Publishing, Basel (2016)
Sullivan, D.F.: A single index of mortality and morbidity. HSMHA Health Rep. 86(4), 347–354 (1971)
United Nations: World population prospects 2019. File POP/5: Median Age by region, subregion and country, 1950–2100 (years). Estimates 1950–2020. New York: United Nations, Department of Economic and Social Affairs, Population Division. https://population.un.org/wpp/Download/Standard/Population/. Accessed 11 December 2019 (2019)
Vanella, P.: A principal component model for forecasting age- and sex-specific survival probabilities in Western Europe. German J. Risk Insur. 106(5), 539–554 (2017)
Vanella, P., Deschermeier, P.: A probabilistic cohort–component model for population forecasting—the case of Germany. J. Popul. Aging. https://doi.org/10.1007/s12062-019-09258-2 (2020)
Wild, F.: Die Pflegeversicherung und die Pflegeausgaben im internationalen Vergleich. WIP-Diskussionspapier 2/10. Wissenschaftliches Institut der der PKV, Köln (2010)
Wingenfeld, K.Der: neue Pflegebedürftigkeitsbegriff. In: Bechtel, P., Smerdka-Arhelger, I., Lipp, K. (eds.) Pflege im Wandel gestalten—Eine Führungsaufgabe. Lösungsansätze, Strategien, Chancen, pp. 39–46. Springer, Berlin (2017)
World Health Organization: World report on ageing and health. World Health Organization, Luxembourg (2015)
Wu, Y.T., Brayne, C., Matthews, F.E.: Prevalence of dementia in East Asia: a synthetic review of time trends. Int. J. Geriatr. Psychiatry 30(8), 793–801 (2015)
Wu, Y.T., Lee, H.Y., Norton, S., Prina, A.M., Fleming, J., Matthews, F.E., Brayne, C.: Period, birth cohort and prevalence of dementia in mainland China, Hong Kong and Taiwan: a meta-analysis. Int. J. Geriatr. Psychiatry 29(12), 1212–1220 (2014)
Ziegler, U., Doblhammer, G.: Projections of the number of people with dementia in Germany 2002 through 2047. In: Doblhammer, G., Scholz, R. (eds.) Ageing, care need and quality of life, pp. 94–111. VS Verlag für Sozialwissenschaften, Wiesbaden (2010)
Acknowledgements
Open Access funding provided by Projekt DEAL. We thank the Institute for Risk and Insurance at the Gottfried Wilhelm Leibniz Universität Hannover for funding our study. Moreover, we appreciate the helpful and timely remarks by the anonymous reviewers of this contribution.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Patrizio Vanella currently works at the Helmholtz Centre for Infection Research. The study was mainly conducted during his time at the University of Hannover.
The original online version of this article was revised: Abstract was included in the html version.
Appendices
Appendix A
Appendix B
See Table 4.
Appendix C
See Fig. 10.

Sources: Human Mortality Database (2019); own calculation and design
Old-age population by 2045 by age group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vanella, P., Heß, M. & Wilke, C.B. A probabilistic projection of beneficiaries of long-term care insurance in Germany by severity of disability. Qual Quant 54, 943–974 (2020). https://doi.org/10.1007/s11135-020-00968-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11135-020-00968-w