Abstract
Coercion in psychiatry is associated with several detrimental effects, including in the long term. The effect of past experience of coercion on the perception of subsequent hospitalisations remains less studied. The present study aimed to assess the impact of past experience of coercion on the perception of coercion and satisfaction with subsequent voluntary hospitalisations. A total of 140 patients who were hospitalised on a voluntary basis were included. Fifty-three patients experienced coercion before this hospitalisation and 87 did not. Patients were assessed for treatment satisfaction and perceived coercion. Health status was also evaluated by both patients and carers. Past experience of coercion was the independent variable. Perceived coercion and satisfaction scores were used as different dependent variables in a series of regression models. Results suggested a long-term detrimental impact of past experience of coercion on some aspects of satisfaction and perceived coercion in subsequent voluntary hospitalisations even when controlling for self and carers-rated health status. Overall, this study suggests that special attention should be paid to patients who are voluntarily admitted to hospital but have a history of coercion, as they may still be impacted by their past coercive experiences. Ways to increase satisfaction and reduce perceived coercion of these patients are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of coercion in mental health care remains a sensitive topic since it infringes the bioethical principal of patient’s autonomy and its efficiency is still discussed in the field [1, 2]. In practice, caregivers have the duty to protect patient’s health and safety as well as other people against the danger patient may represent [3]. Despite the will to improve psychiatric treatment and make it more respectful, it is very difficult to completely avoid coercion. Thus, caregivers are struggling between the two bioethical principles of beneficence and autonomy [4].
Patients generally perceive coercion negatively and many studies have highlighted the multiple harmful effects of perceived coercion on them [5, 6]. Formal coercion is a measure imposed against patient's will, without their agreement or knowledge, such as confinement, prohibition of free movement or contact with relatives, seclusion, restrain and forced medication. It differs from informal coercion in the sense that this is based on an official decision. Informal coercion consists of persuasion, interpersonal pressure, inducements, threats and warnings, carried out by careers or relatives without a formal legal decision [3]. Formal coercion has shown a negative impact on patients’ quality of life [7] but also on their clinical course. Indeed, formal coercion reduces satisfaction with care [8] and treatment adherence in the long-term [9]. Perceived coercion (i.e. the feeling of being coerced) increases disengagement from services and negative therapeutic relationships [10,11,12]. This negative impact on health care process can adversely affect patient’s prognosis due to potentially difficult cooperation [6]. Experience of coercion can also be highly stressful [13]. Moreover, according to Jordan and McNeil [14], higher level of perceived coercion during the psychiatric hospital’s admission process increases the risk of suicide attempts after release, potentially endangering the patient’s life. Several studies have also showed the strong impact of the feeling of being coerced on satisfaction with care [15,16,17]. Finally, past coercion (i. e. a previous experience of formal coercion) is also linked to a higher risk of use of formal or informal coercion in the future [18, 19], potentially leading patients into a vicious circle of poor therapeutic collaboration and the deterioration of their situation.
Evidence about the long-term effect of perceived coercion remains scarce but few studies suggested a worsening of the patients’ attitudes towards treatment and mental health care, which constitutes a barrier to the use of psychiatric services [20]. Past involuntary hospitalisation is related to an increased sensitivity over time to the feeling of being coerced to treatment, leading to lower treatment adherence levels [18, 21]. In their two-year follow-up study, Van der Post et al. [21] added support to the hypothesis that there may be an association between patients’ perception of their past compulsive admission and the risk of re-hospitalisation.
Overall, current studies suggest negative effects of coercive measures on patients, although there is no clear evidence of a causal relationship between past coercion and the perception of future readmission. This is an understudied effect and several authors recommended further studies in order to better understand the complex association between perceived coercion and care [22,23,24].
In order to contribute on this matter, the aim of this study was to assess the impact of past formal coercion experiences on 1) perceived coercion and 2) on satisfaction during voluntary hospitalisation. For methodological reasons, past coercion was defined for the patients as at least one formal experience of confinement, prohibition of free movement or contact with relatives, seclusion, restrain and forced medication. Our goal was to examine how perception of coercion and satisfaction in voluntary hospitalisation can be accounted for by the impact of past coercion experiences. We chose to focus on current voluntary hospitalisation so that patients were in the same context and the only variable that could affect patients' perceptions was the presence of a past experience of coercion, after controlling for self- and carer-rated health status. We hypothesized that long-term detrimental impact of past experience of coercion on satisfaction and perceived coercion could be highlighted in subsequent voluntary hospitalisations.
Material and Methods
Participants
Participants were all hospitalized and were recruited throughout six psychiatric hospitals in the French-speaking part of Switzerland between March 2020 and June 2022. The hospitals were covering several districts in three cantons (Vaud, Neuchâtel, Fribourg) and comprised acute psychiatric wards. Inclusion criteria were to be between 18 and 65 years old, being hospitalised from 7 and 15 days and sufficiently proficient in French to complete the questionnaire. This ensured participants formed a rather homogeneous group in terms of duration of hospitalisation elapsed at the time of assessment. Patients diagnosed with dementia (F00-F09) or intellectual developmental disorders (F70-F79) were excluded. Patients were contacted directly on site to take part in the study on a voluntary basis by trained research assistants. In order to avoid selection bias and to approach more often those patients who are known to be cooperative, each hospital unit drew up a list of eligible patients, who were then selected at random. Approval for this study was granted by the Human Research Ethics Committee of the Canton Vaud, Switzerland (protocol #2016–00,768). Written informed consent was obtained from all participants and all methods were carried out in accordance with the recommendations of the Human Research Ethics Committee of the Canton Vaud and the Declaration of Helsinki.
Measures
Socio-demographic Data
Socio-demographic characteristics such as age, gender, nationality, occurrence of previous psychiatric hospitalisations and main diagnosis were collected through structured questionnaires and medical charts. Past experience of coercion was defined as past involuntary hospitalisation, confinement, prohibition of free movement or contact with relatives, isolation, physical or drug restraint.
The MacArthur Admission Experience Survey (AES) Short Form
The French version of the MacArthur Admission Experience Survey (AES) short form was used to measure patients’ perceived coercion at admission [5]. This 16-item dichotomous (true or false) scale is divided into three subscales and a total score. The Perceived Coercion score focuses on freedom, choice, initiative, control and influence over coming into hospital; the Negative Pressures score focuses on being forced, threatened or physically forced to come into hospital; and the Voice score focuses on having a chance to voice an opinion about coming into hospital. The final item consists of a range of adjectives used to assess the patient’s affective reaction to hospitalisation. Although easy to use and very short, the AES does not cover all aspects of coercion and only refers to the hospital admission process [25].
The Coercion Experience Scale (CES)
The French version of Coercion Experience Scale [CES; 26] was used to measure patients’ perceived coercion during their hospitalisation. The scale consists of 31 items, the first 2 items being 0 to 100 visual analogue scales to assess the extent to which patients remember the coercive measures (item 1) and the extent to which these were considered stressful (item 2). The second part of the questionnaire is based on 29 five-point Likert-type items divided into five subscales: a Humiliation/coercion score, a Physical adverse effects score, an Interpersonal separation score, a Negative environmental influences score and a Fear score.
Satisfaction Regarding Hospitalisation (ANQ)
The Swiss National Association for Quality Development in Hospitals and Clinics (ANQ) has developed a satisfaction measure for patients in psychiatry. The questionnaire includes 6 five-point Likert-type items assessing quality of treatment, information and communication, medication, patient’s implication and discharge preparation [27]. A total score can be computed to assess the global satisfaction of the patient.
Health of the Nation Outcome Scales (HoNOS-F)
The French version of the Health of the Nation Outcome Scales (HoNOS-F) is a routine clinical tool used in order to assess the health and social functioning of people with mental illness [28]. In Switzerland, the HoNOS is routinely used and rated by clinicians for every hospital admission and discharge. The measure has originally been developed in the UK between 1992 and1995 and has since been translated and validated in different languages. In this study, we used the French version translated and validated by Lauzon et al. [29] which it is composed of twelve 5-point Likert-scale items. Several scoring structures have been proposed for the HoNOS scales, some of which were deemed unsatisfactory for the French version. Therefore, as recommended in a large sample study on the French version [28], scores were selected at the item-level and all twelve scores were used.
Self-reported Health
One subscale of the ANQ satisfaction regarding hospitalisation short questionnaire is a self-reported five-point Likert-type item about the patient self-perceived global health.
Statistical Analysis
In order to estimate the relationship between past coercive experiences and satisfaction and perceived coercion during voluntary hospitalisation, we used a series of linear multiple regressions. Past experience of coercion was introduced as the independent variable. All HoNOS items and self-reported health were also introduced in order to control for patients’ health. Age, gender, Swiss nationality, occurrence of previous psychiatric hospitalisation and diagnostic were also controlled for. Coercion and satisfaction scores were used as different dependent variables. All statistical analyses were performed using IBM SPSS Statistics 27.
Results
A total of 140 voluntarily admitted psychiatric patients took part in this study. 53 patients (37.9%) experienced coercion before this hospitalisation and 77 patients (55.0%) were women. Age ranged from 18 to 63 years old (M = 39.26, SD = 14.15). All patients were French-speakers, and the large majority (75.0%; n = 105) was Swiss. Primary diagnosis, based on the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) are presented in Table 1. 71.4% (n = 100) reported at least one previous psychiatric hospitalisation.
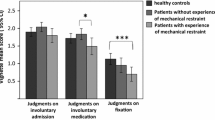
Relationships between past experience of coercion, perceived coercion and satisfaction scores were estimated (Table 2). The AES perceived negative pressures score (β = 0.272, p = 0.016) was significantly predicted by past experience of coercion. The CES perceived fear score (β = 0.220, p = 0.037) was also significantly predicted by past experience of coercion).
One aspect of self-reported satisfaction with treatment (ANQ) was also negatively related to past experience of coercion: asking questions (β = -0.219, p = 0.036). Relationship between dependent variables and covariates are presented in Table 3.
Discussion
Our study examined the relationship between past coercion and future voluntary hospitalisations. Our results suggested a significant detrimental association between past coercion experiences and perceived negative pressure and fear as well as treatment satisfaction for being able to ask questions during hospitalisation after controlling for patients’ self-rated and carer-rated level of health and functioning.
Our findings suggested that patients with a history of coercion are more likely to perceive negative pressure and fear during re-admission and hospitalisation and also be less satisfied with treatments and information, i.e., the ability to ask questions. This is important because it suggests that past coercion negatively affects patients’ subsequent hospitalisation even when these are voluntary. Studies have shown that past coercion can be highly stressful [30, 31]. The relationship between past coercion experience and fear highlight the difference between “objective” and “perceived” coercion and reminds the concept of “coercive shadow”: a patient’s perception of threat, even where no threat may be intended, and the fear of patients that non-compliance may lead to the use of coercion. Patients therefore commonly agree to treatment, including “voluntary” hospital admission to avoid the humiliation and stigma of a compulsory order [32]. Without going that far, past experiences of coercion certainly play a role in the patient's perception of psychiatric care during subsequent voluntary hospitalisations. It also has been shown that fear of treatment can be detrimental to therapeutic alliances and impact health [33]. There are several clinical implications: voluntary patients with a past coercion experience are less likely to adhere to treatment and more likely to have a negative experience of voluntary hospitalisations. Thus, special consideration should be given to patients who have a history of coercion in order to mitigate this potential negative impact from the past.
Regarding the reduction of the feeling of coercion, recent work has identified procedural justice i.e., the feeling of being treated with respect and receiving a fair decision, as an important mean [10, 20]. Silva et al. [34] findings also support this conclusion showing that perceived fairness plays an important positive role in satisfaction and is therefore a key ingredient to improve care.
Additionally, as suggested by the work on patient-centred care, which advocates for care respectful of individual patient preferences, values, and needs, active patient participation in the process is essential to improve satisfaction with care [10, 15, 20, 35, 36]. Within this framework, shared decision-making is the primary means to promote a balanced patient-physician relationship that distances itself from the patriarchal model and promotes changes that address the needs identified in the present study such as voice and access to understandable and quality information [35]. Enhancing the use of shared decision making is therefore a crucial matter to work on in order to increase patients’ satisfaction.
These two propositions are intrinsically linked since the feeling of fairness stems from the feeling of being considered, notably through involvement in care as proposed by the shared decision-making model. In line with the goals of patient-centred care, tools such as the Joint Crisis Plan [JPC; 37] are available to put these propositions into practice. Other possibilities for future research need to be explored, such as identifying modifiable variables that are associated with satisfaction and perception of coercion during voluntary hospitalisations for patients with a history of coercion. We could for example explore the choice of location (distance from home and relatives, contact with other patients, painful history related to location) or the life trajectory (hospitalisation at a turning point in life).
Our study has some limitations. First, our sample size was modest and further research should replicate our results in larger samples. Second, despite our attempt to reduce the selection bias by approaching randomly selected patients, we cannot exclude that the decision to participate or not may have had an impact on our results. Indeed, some patients with a rather negative treatment experience might have avoided participation in our study or, on the contrary, dissatisfied patients might have felt a great need to share their negative experience. Third, we did not have a complete inventory of past coercion experiences or past hospitalisation for each patient and relied on a self-rated indication. Being rather coarse (yes/no), we were not able to estimate whether a dose–response effect of past coercion could be highlighted. This matter should be further investigated in future studies.
Conclusions
Overall, this study indicated that patients with a history of coercion are less satisfied with some aspects of care and are more likely to perceive negative pressures and fear in subsequent voluntary admissions and hospitalisations. This relationship between past coercion and satisfaction was evident even after controlling for patient’s self- and carers-rated level of health and functioning. Therefore, special attention should be paid to patients who are voluntarily admitted to hospital but have a history of coercion as they may still be impacted by their past coercive experiences. This study highlights the necessity to further develop patient-centred care in order to increase long-term satisfaction with psychiatric care.
References
Morandi S, Silva B, Mendez Rubio M, Bonsack C, Golay P. Mental health professionals' feelings and attitudes towards coercion. Int J Law Psychiatry. 2021;74:101665. https://doi.org/10.1016/j.ijlp.2020.101665.
Silva B, Gholam M, Golay P, Bonsack C, Morandi S. Predicting involuntary hospitalization in psychiatry: A machine learning investigation. Eur Psychiatry. 2021;64(1):e48. https://doi.org/10.1192/j.eurpsy.2021.2220.
Szmukler G, Appelbaum PS. Treatment pressures, leverage, coercion, and compulsion in mental health care. J Ment Health. 2008;17(3):233–44. https://doi.org/10.1080/09638230802052203.
Beauchamp TL, Childress JF. Principles of biomedical ethics. New York: Oxford University Press; 1979.
Golay P, Semlali I, Beuchat H, Pomini V, Silva B, Loutrel L, et al. Perceived coercion in psychiatric hospital admission: validation of the French-language version of the MacArthur Admission Experience Survey. BMC Psychiatry. 2017;17(1):357. https://doi.org/10.1186/s12888-017-1519-4.
Golay P, Morandi S, Silva B, Devas C, Bonsack C. Feeling coerced during psychiatric hospitalization: Impact of perceived status of admission and perceived usefulness of hospitalization. Int J Law Psychiatry. 2019;67:101512. https://doi.org/10.1016/j.ijlp.2019.101512.
Rusch N, Muller M, Lay B, Corrigan PW, Zahn R, Schonenberger T, et al. Emotional reactions to involuntary psychiatric hospitalization and stigma-related stress among people with mental illness. Eur Arch Psychiatry Clin Neurosci. 2014;264(1):35–43. https://doi.org/10.1007/s00406-013-0412-5.
Nyttingnes O, Ruud T, Rugkasa J. 'It's unbelievably humiliating'-Patients' expressions of negative effects of coercion in mental health care. Int J Law Psychiatry. 2016;49(Pt A):147–53. https://doi.org/10.1016/j.ijlp.2016.08.009.
de Haan L, van Amelsvoort T, Dingemans P, Linszen D. Risk factors for medication non-adherence in patients with first episode schizophrenia and related disorders; a prospective five year follow-up. Pharmacopsychiatry. 2007;40(6):264–8. https://doi.org/10.1055/s-2007-992141.
Katsakou C, Marougka S, Garabette J, Rost F, Yeeles K, Priebe S. Why do some voluntary patients feel coerced into hospitalisation? A mixed-methods study. Psychiatry Res. 2011;187(1–2):275–82. https://doi.org/10.1016/j.psychres.2011.01.001.
Lidz C, Mulvey EP, Hoge SK, Kirsch B, Monahan J, Eisenberg M, et al. Factual sources of psychiatrice patients' perceptions of coercion in the hospital admission process. Am J Psychiatry. 1998;155(9):1254–60.
Theodoridou A, Schlatter F, Ajdacic V, Rossler W, Jager M. Therapeutic relationship in the context of perceived coercion in a psychiatric population. Psychiatry Res. 2012;200(2–3):939–44. https://doi.org/10.1016/j.psychres.2012.04.012.
Kinner SA, Harvey C, Hamilton B, Brophy L, Roper C, McSherry B, et al. Attitudes towards seclusion and restraint in mental health settings: findings from a large, community-based survey of consumers, carers and mental health professionals. Epidemiol Psychiatry Sci. 2017;26(5):535–44. https://doi.org/10.1017/S2045796016000585.
Jordan JT, McNiel DE. Perceived coercion during admission into psychiatric hospitalization increases risk of suicide attempts after discharge. Suicide Life Threat Behav. 2020;50(1):180–8. https://doi.org/10.1111/sltb.12560.
Katsakou C, Bowers L, Amos T, Morriss R, Rose D, Wykes T, Priebe S. Coercion and treatment satisfaction among involuntary patients. Psychiat Serv. 2010;61(3):286–92. https://doi.org/10.1176/ps.2010.61.3.286
Strauss JL, Zervakis JB, Stechuchak KM, Olsen MK, Swanson J, Swartz MS, et al. Adverse impact of coercive treatments on psychiatric inpatients' satisfaction with care. Community Ment Health J. 2013;49(4):457–65. https://doi.org/10.1007/s10597-012-9539-5.
Svensson B, Hansson L. Patient satisfaction with inpatient psychiatric care. The influence of personality traits, diagnosis and perceived coercion. Acta Psychiatr Scand. 1994;90(5):379–84. https://doi.org/10.1111/j.1600-0447.1994.tb01610.x.
Jaeger S, Pfiffner C, Weiser P, Langle G, Croissant D, Schepp W, et al. Long-term effects of involuntary hospitalization on medication adherence, treatment engagement and perception of coercion. Soc Psychiatry Psychiatr Epidemiol. 2013;48(11):1787–96. https://doi.org/10.1007/s00127-013-0687-x.
Kalisova L, Raboch J, Nawka A, Sampogna G, Cihal L, Kallert TW, et al. Do patient and ward-related characteristics influence the use of coercive measures? Results from the EUNOMIA international study. Soc Psychiatry Psychiatr Epidemiol. 2014;49(10):1619–29. https://doi.org/10.1007/s00127-014-0872-6.
Jaeger M, Rossler W. Enhancement of outpatient treatment adherence: Patients' perceptions of coercion, fairness and effectiveness. Psychiatry Res. 2010;180(1):48–53. https://doi.org/10.1016/j.psychres.2009.09.011.
Van der Post LF, Peen J, Visch I, Mulder CL, Beekman AT, Dekker JJ. Patient perspectives and the risk of compulsory admission: the Amsterdam Study of Acute Psychiatry V. Int J Soc Psychiatry. 2014;60(2):125–33. https://doi.org/10.1177/0020764012470234.
Luciano M, Sampogna G, Del Vecchio V, Pingani L, Palumbo C, De Rosa C, et al. Use of coercive measures in mental health practice and its impact on outcome: a critical review. Expert Rev Neurother. 2014;14(2):131–41. https://doi.org/10.1586/14737175.2014.874286.
Murphy R, McGuinness D, Bainbridge E, Brosnan L, Felzmann H, Keys M, et al. Service Users' Experiences of Involuntary Hospital Admission Under the Mental Health Act 2001 in the Republic of Ireland. Psychiatr Serv. 2017;68(11):1127–35. https://doi.org/10.1176/appi.ps.201700008.
O’Donoghue B, Roche E, Shannon S, Creed L, Lyne J, Madigan K, et al. Longer term outcomes of voluntarily admitted service users with high levels of perceived coercion. Psychiatry Res. 2015;229(1–2):602–5. https://doi.org/10.1016/j.psychres.2015.07.013.
Bergk J, Flammer E, Steinert T. "Coercion Experience Scale" (CES) - validation of a questionnaire on coercive measures. BMC Psychiatry. 2010;10(1):5. https://doi.org/10.1186/1471-244X-10-5.
Golay P, Favrod J, Morandi S, Bonsack C. Psychometric properties of the French-language version of the Coercion Experience Scale (CES). Ann Gen Psychiatry. 2019;18:4. https://doi.org/10.1186/s12991-019-0230-x.
Köhn S, Oedekoven M, Bernert S, Spyra K. Swiss National Association for Quality development in hospitals and clinics (ANQ) Enquête nationale de l'ANQ sur la satisfaction en soins aigus, en psychiatrie et en réadaptation: Étude de test scientifique du nouveau questionnaire succint de l'ANQ sur la satisfaction des patients, rapport final parties 1 et 2. Bern; 2018.
Golay P, Basterrechea L, Conus P, Bonsack C. Internal and predictive validity of the french health of the nation outcome scales: need for future directions. PLoS ONE. 2016;11(8):e0160360. https://doi.org/10.1371/journal.pone.0160360.
Lauzon S, Corbière M, Bonin J-P, Bonsack C, Lesage AD, Ricard N. Validation de la version française du Health of the Nation Outcome Scales (HoNOS-F). Can J Psychiatry. 2001;46(9):841–6. https://doi.org/10.1177/070674370104600908.
Andreasson E, Skarsater I. Patients treated for psychosis and their perceptions of care in compulsory treatment: basis for an action plan. J Psychiatr Ment Health Nurs. 2012;19(1):15–22. https://doi.org/10.1111/j.1365-2850.2011.01748.x.
Frueh BC, Knapp RG, Cusack KJ, Grubaugh AL, Sauvageot JA, Cousins VC, et al. Patients' reports of traumatic or harmful experiences within the psychiatric setting. Psychiat Serv. 2005;56(9).
Szmukler G. Compulsion and “coercion” in mental health care. World Psychiatry. 2015;14(3):259.
Hayes SL, Segal SP. Fear of adverse mental health treatment experiences: Initial psychometric properties of a brief self-report measure. Psychol Assess. 2017;29(5):509.
Silva B, Pauli G, Diringer O, Morandi S, Bonsack C, Golay P. Perceived fairness as main determinant of patients' satisfaction with care during psychiatric hospitalisation: An observational study. Int J Law Psychiatry. 2022;82:101793. https://doi.org/10.1016/j.ijlp.2022.101793.
Barry MJ, Edgman-Levitan S. Shared decision making — The pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–1.
Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract. 2000;50:892–7.
Henderson C, Flood C, Leese M, Thornicroft G, Sutherby K, Szmukler G. Effect of joint crisis plans on use of compulsory treatment in psychiatry: single blind randomised controlled trial. Brit Med J. 2004;329(7458):136. https://doi.org/10.1136/bmj.38155.585046.63.
Acknowledgements
The authors would like to thank Line Morier-Genoud, Charlotte Bonalumi, Guillaume Pauli Louis Prod’Hom, Remy Volet, Maude Bertusi, Sandrine Valloton, Remi Gravier, Rachele Brodard and Lilith Abrahamyan Empson for their help with the patients’ recruitment.
Funding
Open access funding provided by University of Lausanne. This study was based on institutional funding.
Author information
Authors and Affiliations
Contributions
PG designed this research. AB and DM acquired the data. PG and AB analyzed and interpreted the data. PG, AB and DM drafted the first version of the manuscript. BS, SM, OD and CB critically revised the manuscript for important intellectual content. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Disclosure of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martinez, D., Brodard, A., Silva, B. et al. Satisfaction and Perceived Coercion in Voluntary Hospitalisations: Impact of Past Coercive Experiences. Psychiatr Q 93, 971–984 (2022). https://doi.org/10.1007/s11126-022-10005-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-022-10005-8