Abstract
Induced abortion is a reproductive behavior that remains difficult to measure in countries where the procedure is highly restricted by law. Additionally, in some countries where abortion is broadly legal, a high proportion of abortions are carried out by illegal and untrained providers. In these contexts, official statistics are non-existent or highly incomplete. Measurement of the incidence of induced abortion is essential to inform sexual and reproductive health policies and programs. Researchers have developed diverse methodologies over the years. Direct methods, such as population-based surveys that ask women about their abortion experience, generally are subject to high levels of underreporting. A range of indirect methods have been developed to obtain more accurate estimates. Created in the early 1990s, the Abortion Incidence Complications Method (AICM) is a widely applied indirect method that has produced robust estimates of abortion incidence in a range of contexts. This paper presents the original AICM methodology used in countries where abortion is highly restricted. It also highlights modifications made for two situations, one of which is newly emerging. First, the methodology has been adapted recently for countries where, despite the restrictive abortion laws, a new, relatively safe method—medication abortion (mainly misoprostol alone)—is increasingly used. Second, it has been adapted for countries where abortion is broadly legal but unsafe abortion remains common. The paper also assesses performance of the methodology to the extent available data permit. The paper provides guidance to researchers who want to conduct abortion incidence studies using the AICM and to further advance the measurement of abortion incidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Measuring abortion incidence continues to be a challenge for researchers because of the difficulty of assessing its magnitude in settings where the procedure is carried out clandestinely, both where it is highly restricted by law and where it is legally permitted under broad grounds but a high proportion of abortions are carried out by non-approved and untrained providers (Remez et al. 2010). The difficulty stems from the lack of health systems data and the typically high levels of underreporting in surveys that ask women directly about their abortion experience. Abortion remains one of the most sensitive sexual and reproductive behaviors because of social stigma, privacy concerns, and fear of legal sanctions (Singh et al. 2018). Yet, to make informed decisions to prevent unintended pregnancies and unsafe abortions and to improve women’s reproductive health, policy makers and health planners require timely and reliable information on the incidence of induced abortion, on the conditions under which abortion occurs and on inequities in access to safe abortion. Reliable, current estimates of abortion incidence also inform public debate about prioritizing resources, changing abortion law and ensuring access to services under existing legal criteria.
Due to the difficulty of obtaining precise information on pregnancy terminations, researchers have developed diverse methodologies and data collection approaches over the years to measure abortion incidence. These approaches fall under two main categories: direct and indirect methods (Rossier 2003). The direct methods include official statistics (potentially of good quality in countries where abortion is broadly legal); surveys of known abortion providers on the number of abortions performed, (also feasible in countries where abortion is broadly permitted); and surveys of women on the number of abortions they have had in a specific period. However, these approaches are either not feasible or not likely to produce good quality data in countries where unsafe and clandestine abortion remains widespread. For example, a 2001 study in Mexico pilot tested four methods, three of which were direct and one indirect, and found that the indirect method obtained notably higher levels of reporting on attempts to induce abortion (Lara et al. 2004).
To improve the measurement of abortion in contexts where direct approaches do not work well, researchers have developed several indirect methods over the years, including some new and innovative ones (Sedgh et al. 2016). Indirect methods are varied; they use a range of data sources, assumptions, and elements from both direct and indirect approaches to obtain the most complete and accurate reporting. Indirect methods that have existed for some years include the Abortion Incidence Complications Method (AICM), the Randomized Response Technique (RRT), the Anonymous Third Party Reporting method (ATPR), and the Secret Ballot or Sealed Envelope method. (Singh et al. 2010a; Juarez et al. 2010; Oliveras and Letamo 2010; Rossier et al. 2006; Zamudio et al. 1999). Unlike the AICM, the other three methods have been used in very few studies. A few new methods (adapted from other fields or variants of previously existing methods) are now being applied to estimate abortion incidence: the Best Friend method, the List Experiment, the Double List Experiment, and the Network Scale-up method (Miller et al. 1986; Moseson et al. 2015; Rastegari et al. 2014; Yeatman and Trinitapoli 2011). Studies are on-going to test these methods and assess them against other methods, including the AICM.
The purpose of this paper is to focus on one of these methods, the AICM, to provide an overview of how the method is applied, including modifications to the original formulation, and to assess how well it has performed as far as available data permit. The key reason for focusing on this method is that it has been widely applied—in 23 countries in the three major regions of the developing world, as of 2017—and has produced useful and robust estimates of abortion incidence, and the incidence of women treated in facilities for abortion complications. (See Appendix, Table A in Online Resource 1 for a list of countries where AICM studies have been conducted). The goal of this paper is to help researchers apply the AICM method or compare its performance with that of other methods in new studies to measure abortion incidence in contexts where good quality data are lacking.
The paper first presents a description of the standard AICM approach, as used in contexts where abortion is highly restricted. It then discusses two key adaptations of the methodology: to include measurement of medication abortion (misoprostol, or misoprostol and mifepristone), which has gained prominence recently in many countries with highly restrictive abortion laws; and to estimate legal, safe abortion in contexts where the law has been broadened but unsafe abortion remains common.
Following the overview of the three variants of the methodology, we summarize evidence to crosscheck and assess the validity or reliability of particular assumptions or data used for the AICM methodology. Finally, we comment on the strengths and limitations of the AICM approach (within the limits of available data), and discuss areas for further research to improve the methodology.
Review of AICM Methodology
The method is built on the empirical observation that of all women who have abortions in highly restrictive settings, some experience complications and some do not. Of those who experience complications, some seek and obtain care in a health facility and some do not obtain treatment, for a number of reasons. The subgroup of women who are treated for abortion complications is visible and measurable, and the AICM method requires collection of data on the number of women in this group. Second, the method estimates the proportion that this subgroup constitutes among all women who had abortions through a survey of health professionals and key informants who have extensive experience and knowledge about abortion services in their country. Third, the total number of women having abortions is then calculated based on data from these two sources. The following paragraphs describe data sources, key questions, calculations, and the measures estimated.
Standard AICM Approach
Researchers developed the methodology in the early 1990s and initially applied it in Latin America, where abortion was highly restricted and when the use of misoprostol for abortion was just beginning (Singh and Wulf 1994). Since then, the methodology has been applied widely and modifications have been made as needed in different legal and service provision contexts, as discussed below. However, the basic approach remains relevant and continues to be appropriate for some contexts. Figure 1 provides an overview of the approach, which is explained in detail below.

Note †The proportion of women who experience complications from their abortion is calculated for each of the four population subgroups: urban nonpoor, rural nonpoor, urban poor and rural poor. The subgroup estimates are then weighted by the proportion of women in each population subgroup. The weighted estimates are summed to yield the proportion of all women having abortion who received care in facilities for abortion related complications
Standard AICM methodology for estimating abortion
Data Sources
The AICM method requires two types of data:
-
The number of women treated for abortion complications at health facilities;
-
The proportion of all women having abortions who have complications and receive treatment in health facilities.
Health Facility Survey: The Number of Women Treated for Abortion Complications
In the first study, in the early 1990s, covering six countries in Latin America, reliable government health statistics were available on the number of women treated for abortion complications in public-sector hospitals. These statistics were supplemented by estimates of the proportion of women who were likely treated for abortion complications in private-sector facilities, which at that time provided a small fraction of these services. The methodology was subsequently generalized to other regions, in countries where good quality health systems data on postabortion care (PAC) services did not exist. In these countries, researchers developed an alternative approach for estimating the PAC caseload: a survey of a nationally representative sample of health facilities that have the capacity to provide postabortion care, referred to as a Health Facilities Survey (HFS). Between these two sources of data on the number of PAC cases, government health systems data are preferred when they are available and of good quality. An additional source of data on the number of PAC cases that has been used in a few countries, in most cases in combination with an HFS, is a Prospective Morbidity Survey (PMS) done in a representative sample of health facilities. This survey interviews each PAC patient and her primary care provider over a period of time in the sampled facilities, typically two to four weeks. The survey collects additional patient-specific information on various topics including socio-demographic characteristics of women who have abortion complications and the severity, clinical management, and treatment of complications (Chae et al. 2017; Gebreselassie et al. 2010).
Sample Design
The HFS survey is based on a sample of all facilities in the country with the potential to provide PAC. The sample is selected from the universe of all facilities stratified by ownership (public, private and NGO) and by type of facility (from tertiary hospitals to primary health clinics), depending on the context of each country. The HFS sample ideally covers all major regions of the country, with the occasional exception where the conditions are such that the safety of field staff cannot be guaranteed. In smaller countries, the sample is drawn from all regions. In very large countries, a two-step procedure is followed—first, a randomly selected representative sample of sub-areas is drawn (e.g., states or districts) and second, a sample of health facilities is drawn from within the selected states or districts. In designing the sample, to ensure adequate representation, attention is paid to maintaining a minimum proportion of facilities in each sample category (a rule of thumb that has been commonly applied in these studies is a minimum of 8%). Typically, an HFS sample includes a very high proportion or all of the large facilities, such as tertiary hospitals, because they have large PAC caseloads, and a lower proportion of smaller facilities, such as health centers that have smaller caseloads and are more numerous.
Key Questions
The HFS survey asks a series of questions to obtain the total number of women treated for any abortion complication—those resulting from induced abortions as well as from miscarriages. Because providers have difficulty distinguishing induced abortions from miscarriages, it is not feasible to obtain information for each of these pregnancy outcomes. Four questions are asked about the number of PAC cases treated in each sampled facility, to be sure to capture both outpatients and inpatients as well as variations in how individuals perceive and describe events in different time periods (See Appendix, Table B1 in Online Resource 1 for key questions used in the HFS):
-
Outpatients in an average/typical month
-
Outpatients in the past month
-
Inpatients in an average/typical month
-
Inpatients in the past month
Use of two reference periods—the average month and the past month—also improves the accuracy of the estimate by obtaining the variation in numbers treated from month to month. In each facility, we interview a key person who is knowledgeable on PAC at the health facility. Depending on the level of the facility, respondents could be the facility director, chief obstetrician/gynecologists, medical officers, clinical officers, trained midwives, nurses, or auxiliary nurses.
Health Professionals Survey: Proportion of All Women Having Abortions Treated in Facilities
The second data source, a survey of knowledgeable health professionals, remains an essential component of an AICM study. For the HPS survey, the research team selects a purposive sample of experts who are well-informed about abortion provision in the study country. Depending on the size of a country, the sample size may vary between 50 and 200 experts from across the country. Informants are selected to represent a broad range of perspectives including health providers (OB/GYNs, general practitioners, medical officers, nurse/midwives), researchers, teachers, policy makers, program planners, leaders of NGOs (e.g., those that provide abortion or focus on women’s health), and leaders of relevant civil society organizations. Where availability of key informants with the required expertise permits, at least 25 respondents are surveyed in each major region, allowing for estimates of multipliers in each major region, so that both regional and national estimates can be calculated.
The HPS survey generates the following data (See Appendix, Table B2 in Online Resource 1 for key questions used in the HPS):
-
The percentage distribution of women having abortions according to type of abortion provider
-
The percentage of women having abortions who have complications serious enough to require treatment in a health facility, by type of provider, and
-
The percentage of women who had such complications who obtain treatment in facilities.
All of these questions are asked for each of four groups of women: urban non-poor; urban poor; rural non-poor; and rural poor. We obtain data separately for these four groups because they are expected to have significantly different access to safe abortion services, and key informants would be better able to estimate for each group separately than for the entire population of women. This approach is expected to more accurately capture the situation of all women in the country.
Data Analysis: Key Steps
Calculating the Number of Women Treated for Any Postabortion Complication
Several calculations are made to estimate the total number of PAC cases treated per year in all facilities providing this service.
-
First step: For each sampled facility, calculate its annual total number of PAC patients (the sum of the average values of the typical and past year annualized estimates—for outpatients and inpatients).
-
Second step: Apply sample weights to obtain national estimates of the annual number of women treated for any abortion complication, for all facilities in the country.
Appendix, Table C in Online Resource 1, provides an example of the calculations needed to estimate the total number of PAC cases for Uganda General Hospital, using the 2013 HFS.
Removing Complications of Miscarriages from Total PAC Cases
As stated earlier, the PAC caseload includes women treated for complications from both induced abortion and miscarriages. We need to estimate and remove the number of women treated for complications of miscarriages to derive the number treated for induced abortion complications. We assume that miscarriages happening at later gestations (weeks 13–22) are likely to require facility-based treatment, while those at earlier gestations would typically not require treatment at a facility, given the more minor symptoms. In addition, miscarriages at 23 or more weeks are not included in this calculation because these events are usually classified as fetal deaths rather than as abortions. To remove PAC cases due to miscarriage, the following calculations are required:
First Step: Estimate Late Miscarriages Potentially Requiring Treatment
According to clinical studies, late miscarriages (those that occur at 13–22 weeks of pregnancy) represent 2.9% of all known pregnancies and 3.41% of live births (Bongaarts and Potter 1983; Harlap et al. 1980). Since estimates of the annual number of births are usually available or can be calculated, the total number of late miscarriages likely to need facility-based treatment is estimated by applying the 3.41% to the annual number of births. The number of births may be obtained from national statistical offices or calculated by applying age-specific fertility rates from the most recent Demographic and Health Survey (DHS) to the number of women in each age-group, obtained from national sources or from the United Nations. In some cases, DHS data are used to obtain region-specific estimates of births.
Second Step: Estimate Late Miscarriages that are Treated in a Health Facility
Not all women with later-term miscarriages receive care in a facility. We assume that the proportion of these women who are treated at facilities is equal to the proportion of women who deliver in a facility, and we apply this proportion to the total number of later-term miscarriages to derive the number treated in facilities. The proportion of women who deliver in a facility is usually obtained from a recent national survey such as the DHS. In some sub-Saharan African countries, DHS data on women’s reason for not delivering in a health facility show that a substantial proportion of women do not deliver in facilities because of cultural reasons (i.e., “it is customary to deliver at home”), not because of lack of access to health facilities. For these countries, we modify the assumption, as it is likely that this group of women would seek care for abortion complications. We assume that the proportion of later-term miscarriages receiving care in a facility includes both women who deliver in a facility as well as those who do not deliver in health facilities for cultural reasons (Moore et al. 2016).
Finally, the number treated in facilities for complications from miscarriage is subtracted from the total cases of abortion complications obtained in the HFS to yield the number treated for induced abortion complications.
Calculation of the Multiplier
As mentioned above, we need to estimate an adjustment factor, or multiplier, that represents women who had abortions other than those who were treated for complications. Data to estimate this factor come from the HPS survey.
Three main steps are needed to estimate the multiplier, and calculations are done for each population subgroup and then combined, weighting each subgroup by its proportion of all women of reproductive age, to yield a national multiplier. Where sample sizes are large enough to provide regional estimates, we make the calculations by region to yield a multiplier for each region (Bankole et al. 2015). Data from the Uganda 2013 (Prada et al. 2016) incidence study are used to illustrate these calculations (Tables 1 and 2).
First Step
Obtain the proportion of all women obtaining an abortion who will likely develop complications requiring treatment in a facility by multiplying the proportion obtaining an abortion from each provider type (Table 1, column B) by the expected complications rate associated with the provider (Table 1, column C), and then summing across all provider types (Table 1, column D). Table 1 shows calculations for one subgroup, urban non-poor women, and the same calculations are carried out for all four subgroups.
Second Step
Estimate the proportion of all women having an induced abortion who will receive treatment (Table 2, column B). This is obtained by multiplying the total proportion estimated to develop complications for each subgroup (e.g., 31.31% for urban non-poor women, from Table 2, total of Column D) by the proportion likely to obtain care in a facility (83.20% in Table 2, Column C = 26.05% in Table 2, column D). Note that the last number in Table 1 is the first number in Table 2, indicating that the calculations in Table 1 must be done for all four population subgroups.
Third Step
Weight the proportions likely to get care in a facility to reflect the size of the four population subgroups in the country. Information on the distribution of women by socio-economic groups and residence can be estimated using the wealth index (calculated by DHS surveys) or the level of education as a proxy variable for poverty, cross-tabulated by urban and rural place of residence. In the Uganda example (Table 2, Column E), we used women’s level of education, with poor women defined as those who had seven or fewer years of schooling and nonpoor women as those with eight or more years of education. The national proportion of all women having abortions who are treated for complications in health facilities is 29.73%, the sum of the weighted proportions for the four subgroups (Table 2, column. F). The multiplier is the inverse of the weighted national proportion (Table 2, column G) (100/29.7 = 3.37). We also estimated multipliers for each major region of the country, and found that these ranged narrowly between 3.30 and 3.87 (data not shown).
The multiplier represents the number of women having induced abortions and not experiencing complications and those who have complications and do not obtain care, including those who die as a consequence of the abortion. The multiplier is also an indicator of the relative safety of abortion services and accessibility to medical care. In countries where conditions of abortion provision are very poor and the proportion of all women having abortions requiring and receiving treatment is large, the multiplier is low, such as one in three. This estimate of 3.37 for Uganda as a whole means that for every woman treated in a health facility there are more than two who have abortions but who do not receive care, either because they do not need or could not get care. In countries where conditions of abortion provision are better (safer services and better access to PAC) the adjustment factor is typically one in five or higher, and the proportion of women treated in facilities is relatively small. As a rule of thumb, when safe abortion is widely available, the multiplier is higher and the proportion of women who are hospitalized for abortion complications is smaller. The opposite applies when abortion is unsafe: a lower multiplier and higher proportion of women hospitalized.
Calculation of the Estimated Total Number of Induced Abortions Per Year
The product of the multiplier or adjustment factor and the number of women treated for induced abortion complications is the estimated total number of abortions in the country. The AICM methodology does not generate an exact estimate of abortion incidence; rather, it produces a range around a medium estimate, based on the 95% confidence intervals around the estimated PAC caseload. Figure 1 summarizes the standard approach for estimating the number of induced abortions in countries where abortion is highly restricted by law.
Other data needed to estimate abortion incidence include the number of women of reproductive age, the total number of live births and the percentage of women who deliver at a formal health facility, by region and nationally. Calculations to estimate the abortion rate and ratio for Uganda 2013 are shown in Table 3.
Adapting AICM to Changing Contexts
Over the years, the AICM has evolved to adapt to the changing contexts of abortion provision. This section focuses on two important changes and discusses how the AICM was adapted to take them into account. The first is increased use of misoprostol, a relatively inexpensive and accessible pill that is used to induce abortion, which has substantially changed the practice of induced abortion in many developing countries. Misoprostol has gained widespread recognition for its off-label use as an effective abortifacient when used alone within the first nine weeks of pregnancy (Bracken et al. 2007; Grapsas et al. 2008; Middleton et al. 2005). The increasing availability of the method, its efficacy in completing an abortion and the fact that it can be obtained from a range of providers and can be self-managed, has important implications for the AICM. Adaptation is needed in the HPS, while the HFS remains essentially the same.
The second adaptation of the AICM was needed for its application in countries where abortion laws are liberal but clandestine, unsafe abortion is prevalent and coexists with substantial numbers of safe, legal abortions. Numerous reasons account for the persistence of unsafe abortions, including inadequate provision of affordable, accessible safe and legal abortion services, poor quality of existing services, and low levels of awareness of abortion law change. In such mixed service provision settings, both the HPS and the HFS need to be modified to take account of widespread occurrence of both legal and clandestine abortions.
Increased Use of Misoprostol
To incorporate the use of misoprostol in abortion estimates, the distribution of women obtaining abortion according to type of provider, used in the standard AICM approach, needs to be expanded to include type of method.
Researchers expanded the HPS questionnaire to collect information on the distribution of all women having abortions according to three categories of methods: medication abortion, surgical methods and other methods, and within each method category, the distribution by type of provider (Chae et al. 2017; Sully et al. 2018b). They took this approach in recent applications of the AICM in Kinshasa-DRC and Zimbabwe, where the use of misoprostol was considered to be extensive and the abortion law was highly restrictive. They also modified the additional questions required for the calculation of the multiplier according to the three-way categorization of abortion methods. That is, the probability of experiencing abortion complications was asked for each of the three categories of abortion methods by type of provider, and the probability of obtaining care for complications was asked for each method category. They asked each of the four population subgroups these sets of questions (see Appendix, Table D in Online Resource 1 for an illustration of the modified questions used in the HPS survey of Zimbabwe). Figure 2 illustrates the adaptation of the AICM methodology for contexts where the use of misoprostol is extensive and abortion is highly restricted.

Note †The proportion of women who experience complications from their abortion is calculated for each of the four population subgroups: urban nonpoor, rural nonpoor, urban poor and rural poor. The subgroup estimates are then weighted by the proportion of women in each population subgroup. The weighted estimates are summed to yield the proportion of all women having abortion who received care in facilities for abortion related complications
AICM Methodology adapted for countries where misoprostol or MA is widely used and abortion is highly restricted
Analysis: Estimating Abortion Incidence
For this adaptation, researchers incorporated an additional element into the calculation of the multiplier: the distribution of all women having abortions according to the three categories of methods (surgical abortion, medical abortion and other methods, see Fig. 2). They distributed the proportion using each method category according to type of provider, and then multiplied each method-provider category by HPS respondents’ estimates of the proportion of women having complications. The sum of the proportions of women experiencing complications across provider types within each of the three method categories produces estimates of the proportion of all women using that method who would experience complications. They then multiplied these method-specific proportions with complications by method-specific proportions likely to receive treatment, provided by the HPS respondents. They made these calculations for each of the four population subgroups. The sum of the products for the three methods provides an estimate of the proportion of women who receive treatment for complications from induced abortions for each population subgroup. The remaining steps are the same as in the standard AICM: subgroup estimates were weighted by the proportion of women in each population subgroup, and the weighted estimates were then summed to yield the proportion of all women having abortions who receive care for complications. The multiplier is the inverse of this number.
Mixed Legal Settings
In mixed legal settings, where both legal and clandestine abortions are common, the AICM requires some adaptation to estimate both legal abortion and clandestine abortions. For this purpose, we expanded both the HFS and the HPS to collect relevant information. The HFS needed to be expanded to obtain counts of legal abortions and PAC caseload, and the HPS needed to obtain additional information on the proportion obtaining abortions from approved or legal providers separately from the proportion obtaining abortions from non-approved or illegal providers. Researchers have used this adaptation to estimate the incidence of abortions in Nepal, Ethiopia and Bangladesh (Puri et al. 2016; Moore et al. 2016; Singh et al. 2017).
Data Required
In the case of the HFS, data are collected on both legal abortions performed and abortion-related complications treated. In these mixed contexts, the HFS sample of facilities must represent those that provide legal abortion services as well as those that provide postabortion care. A second source of data is often used in these contexts; NGOs generally provide legal abortions and have good quality data on their abortion services. Where these data exist and are reliable, we use them, and this segment of providers does not need to be included in the HFS or HPS data collection because this component of abortions is directly measured. Thus, the total number of legal abortions will come from the combination the HFS and NGO service statistics. See Appendix, Table E1 in Online Resource 1 for illustrative example from Nepal of HFS questions to obtain the count of legal abortions; the standard questions are used to obtain the count of PAC cases.
In the case of the HPS, researchers expanded the types of providers (and subsequent questions on the probability of complications) to include those that are legally permitted to provide abortion care and those that are sources of unsafe or illegal abortions. Countries use different terms to describe legal providers, for example in Nepal, the term is ‘certified’ provider, and in Ethiopia, it is ‘approved’ provider. These categories may differ depending on the country. The usual set of questions are asked for this expanded list of providers—what is the percentage distribution of women having induced abortions by type of provider; what is the proportion estimated to have a complication needing treatment in a facility for each type of provider; and what is the probability of getting care among women who experienced a complication. As in the case of the standard AICM, this information is obtained for four subgroups of women: urban non-poor, urban poor, rural non-poor, and rural poor. See Appendix, Table E2 in Online Resource 1 for Nepal’s HPS questions on approved and non-approved providers.
Analysis: Estimating Abortion Incidence
For this adaptation of the AICM approach, abortion incidence is estimated in two components (Fig. 3). The first component is legal abortions, estimated based on the data sources mentioned above. This is a direct estimate, generally not needing any further adjustments to the number of legal abortions obtained from a nationally representative HFS survey and statistics from NGOs. The second component is an estimate of illegal or unsafe abortions using indirect estimation techniques, applied to data obtained from the HFS and the HPS. Because of the legal abortion component, a couple of additional steps are needed in the calculations to obtain the total number of unsafe abortions.

Note †The proportion of women who experience complications from their abortion is calculated for each of the four population subgroups: urban nonpoor, rural nonpoor, urban poor and rural poor. The subgroup estimates are then weighted by the proportion of women in each population subgroup. The weighted estimates are summed to yield the proportion of all women having abortion who received care in facilities for abortion related complications
AICM adapted for contexts in which both legal/approved abortions and illegal/clandestine abortions are prevalent
-
Some legal abortions result in complications that are treated in health facilities, and these must be subtracted from the total number of women treated for induced abortion complications, to obtain the number of women treated for complications of illegal induced abortion.
-
In addition, the multiplier must be calculated based on the HPS data for those providers that are not approved, or not certified, because these are the providers that conduct illegal and unsafe abortions. Apart from this, the approach remains the same as in the standard AICM.
-
Multiplying these two estimates yields the total number of illegal abortions.
An example of a recent utilization of this adapted methodology for estimating legal and illegal abortion is presented for Nepal (see Appendix, Table F in Online Resource 1) (Puri et al. 2014). In Nepal, abortion was legalized for broad criteria in the first trimester and restricted criteria in the second trimester in 2002. Despite the availability of legal abortion services, many women still obtained illegal and unsafe procedures.
Cross-checking and Validation of AICM Methodology
The reliability of the AICM estimates of abortion incidence must be assessed by cross-checking the adequacy of the data and the validity of the assumptions used wherever possible. A few sources allow for comparison of AICM results with estimates from other indirect or direct estimates of abortion incidence, or allow validation of AICM assumptions. In addition, some internal checks can be used to assess the quality of the data collected for the AICM. In this section, we summarize internal checks as well as external data that permit cross-checking of AICM inputs and/or estimates.
Internal Checks of AICM Data
Average Month and Past Month
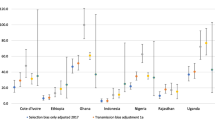
The HFS questionnaire elicits information about abortion complications treated in the facility according to two reference periods: in a typical/average month (in the past year) and in the past month. Demographic studies show that the reference period used may affect reporting: We obtain information for two reference periods to reduce potential bias from using any one period, and we average the numbers reported for the two reference periods to improve the accuracy of the estimate. One of the internal consistency checks that we conduct is to compare the means reported for these two time periods. This comparison shows a systematic differential across countries: Respondents report somewhat higher numbers of women treated for complications for the average month than for the past month. This is plausible because the average month captures variation within a one-year period, while the past month may reflect seasonal differences. We conclude that the systematic difference argues for continuing to obtain both measures, and for using the average of these two measures as the best estimate of the number of PAC cases. The difference between the two estimates for a number of recent AICM studies ranges from a low of 6% to 29% (Table 4).
Pattern of Results from HPS Surveys and Supporting Data from External Sources
The plausibility of results from the HPS can be assessed according to whether key informants’ estimates of the distribution of women according to type of provider within population subgroups and of the probability of complications by type of provider and across subgroups fit expected patterns. The expected pattern is that better-off women, who are able to afford the services of trained medical professionals, and urban women, whose place of residence facilitates finding a safe provider, are more likely than rural and poor women to access abortion from a trained provider. Data for two countries from independently-conducted community-based surveys support these expected patterns. For instance, in a large-scale survey in Nigeria, 59% of non-poor women had a surgical procedure performed by a medically trained professional, compared with only 29% of poor women; and while only 8% of non-poor women used traditional or self-induced methods of abortion, 30% of their poor counterparts did so (Bankole et al. 2006). Similarly, a national survey of women of reproductive age in the Philippines found that higher proportions of non-poor women than poor women sought abortion from general practice doctors and obstetricians/gynecologists (55% vs. 17%); while higher proportions of poor women obtained an abortion with the help of a friend, relative or partner, or induced the abortion themselves (44% vs. 30%) (Singh et al. 2006).
We also expect the probability of complications to be much lower for providers with formal training (doctors, midwives, and nurses) compared with untrained providers or the woman herself using an unsafe method. In Nigeria, evidence from the community-based survey of women shows that the level of abortion-related complications varies with the provider and method used: it was 36% among women who used a remedy with a traditional healer, with a friend or on their own, and 25% among women who underwent a surgical procedure (Dilation & Curettage, Dilation & Evacuation or Vacuum Aspiration) (Bankole et al. 2006). Also, in the Philippines, the level of abortion-related complications varies by the method used: 70% of women who used massage or insertion of a catheter and 44% of those who took misoprostol had severe complications, while only 13% of women who underwent surgical procedures did so (Singh et al. 2006).
Estimates from a cross-section of countries where recent AICM studies have been conducted are consistent with these expected patterns: With few exceptions, health professionals estimate that non-poor women, irrespective of where they live (urban or rural residence) are more likely to obtain abortion from trained providers compared to poor women in urban areas, with poor rural women being least likely to do so (see Appendix, Table G in Online Resource 1). In addition, the typical pattern is that the probability of complications is much higher for untrained providers and women attempting induced abortion themselves compared with trained providers (see Appendix, Table H in Online Resource 1). When combined, these two measures (source of abortion and probability of complication) result in lower probabilities of complications among urban and non-poor women compared to rural and poor women (Table 5). This is consistent with empirical evidence. For example, the Philippines survey found that rural and poor women were more likely to experience severe abortion-related complications than their urban and non-poor counterparts (38% and 41% compared with 33% and 20%, respectively) (Singh et al. 2006).
According to HPS surveys in 12 countries with recent studies of abortion incidence, key informants’ estimates of the proportion obtaining needed care matches the expected pattern. Urban and non-poor women are much more likely to obtain care than rural and poor women: On average, among 12 countries with recent studies, an estimated 55% of poor women who need care from complications obtain it, while 77% of non-poor women obtain such care (Table 5).
Additional External Validation of AICM Results
Only a few sources of external data allow for cross-checking of the AICM assumptions and estimates, but such comparisons are extremely useful to validate the methodology. These include comparisons of HFS estimates of the number of women treated for complications with official statistics or with results from other data collection approaches such as a Prospective Morbidity Survey (PMS); comparison of a multiplier based on the HPS with multipliers from population-based surveys; and AICM estimates of abortion incidence with estimates obtained through different methodologies, such as the secret ballot or sealed envelope approach.
AICM Estimates of PAC Cases Versus Facilities’ Own Statistics: The Case of Colombia
In the case of Colombia, data on the number of women treated for postabortion complications were available for a subset of facilities covered by the HFS. This permitted comparison of HFS estimates of the number of PAC patients for each of these individual facilities. Of the 188 health facilities that reported providing postabortion care, less than half (87) were able to provide statistics for 2008 disaggregated by ICD-10 diagnostic codes, which are necessary to identify patients (Prada et al. 2011).
Comparing data from facilities that had data from both sources, we found that the number of PAC patients estimated by the two sources were within 20% of each other (the HFS estimate was 30,026, compared to 24,083 based on facility statistics). Factors that contribute to this difference include the fact that the calendar period covered by the ICD-10 statistics and the HFS estimates were somewhat different (2008 and 2008–2009, respectively); and that some cases were likely misclassified or incorrectly coded within the ICD-10 system. The miscoding could occur because of difficulty identifying symptoms, or in some cases, providers’ unwillingness to code a case as abortion-related because of stigma. Given that part of the difference can be accounted for, the observed gap suggests that the two sources can be considered to have yielded similar results.
AICM Estimates of PAC Cases Versus PMS Data
Another type of external crosscheck of PAC caseload estimates from HFS surveys is to compare these results with estimates from a Prospective Morbidity Survey (PMS). The PMS focuses on documenting morbidity and treatment, and it collects data on all women admitted to facilities with a diagnosis of complications of abortion. When conducted in the context of an AICM, the survey may be implemented in all facilities sampled for the HFS, or in a subsample of such facilities. The PMS covers all such patients treated over a period of a few weeks, typically 4 weeks. Because the PMS attempts to capture all PAC patients treated during a recent period, it approximates the past month estimate from the HFS. To make an accurate comparison, results shown in Tables 6 and 7 are limited only to facilities with data from both sources.
In three recent Sub-Saharan African studies, Kenya (Mohamed et al. 2015; Ziraba et al. 2015), Ethiopia (Gebrehiwot et al. 2016; Moore et al. 2016), and Zimbabwe (Madziyire et al. 2018; Sully et al. 2018b), AICM studies included Prospective Morbidity Surveys, providing the opportunity to compare estimates from these two sources. The results show that the HFS past month estimate is substantially higher than the PMS estimate in Ethiopia (a difference of 24%) and much closer (and in the opposite direction) in the two other countries (− 6% and − 7%) (Table 6). Overall, it is likely to be more difficult to ensure complete coverage of all patients, especially in larger facilities, because greater caseloads combined with multiple points of admission and treatment may make it difficult to achieve 100% coverage of incoming patients. Table 7 examines differences by type of facility, which is closely related to size. In the case of Ethiopia, the difference between the two sources is somewhat larger for public hospitals than for public health centers. The expected pattern is more evident in Kenya and Zimbabwe. In Kenya, facility size increases systematically from level 2 to level 6: In smaller facilities, the PMS count exceeds that of the HFS, and the reverse is true in larger facilities. In Zimbabwe, the expected pattern occurs within the public sector in the progression from the smallest facilities (health centers) to smaller district hospitals and somewhat larger provincial hospitals; the difference is greatest for the largest central hospitals. It is helpful to see that despite the differential in estimates between the two sources by type of facility, the overall difference at the national level is negligible in Kenya and Zimbabwe, although it remains sizable for Ethiopia.
Reasons for the much larger difference between the two data collection approaches in Ethiopia may be linked to the observed pattern of much greater differences in the public sector: Although we are not aware of specific factors that would make it more difficult to achieve high levels of coverage of incoming patients in the public than in the private sector, it is possible that collecting patient data for 24 h every day, including weekends, may differ between sectors, and 100% coverage may be especially difficult to achieve during the busiest hours in the larger facilities. In addition, it appears that in Ethiopia, issues that affect coverage may have a greater impact in certain regions: The fact that in six of the 11 regions, differences are relatively small (− 9% to + 16%, data not shown) but very large for two regions that account for large proportions of the national PAC caseload (+ 28% and + 48%) suggests that under- or over-counting may have occurred in these two regions due to factors beyond the application of two different data collection approaches. More applications of these two approaches are needed to provide a broader evidence base on which evaluate the two approaches.
Comparison of Multipliers from AICM Studies and Population-Based Surveys
Information from surveys of women themselves is a valuable alternative source for estimating the multiplier. External estimates of multipliers that use approaches such as this provide a valuable check against AICM estimates of multipliers based on the opinions of knowledgeable key informants.
In Burkina Faso, a study conducted in 2008 (Sedgh et al. 2011), estimated multipliers using two methodologies: the standard AICM and the Anonymous Third Party Reporting method (ATPR), which involved interviewing women about abortions of their confidantes in a community-based survey (CBS) of women of reproductive age. The information collected included whether a confidante who had an abortion had a complication and whether she received treatment for it, which could be used to calculate a multiplier comparable to the AICM multiplier. In this study, the CBS survey generated a slightly larger multiplier than the AICM (4.2 versus 3.8): It is possible that the CBS-based multiplier is more accurate than that of the AICM; however, the difference is relatively small, and the similarity of results from these two very different methodologies provides some validation of the AICM’s HPS-based multiplier.
Discussion and Conclusions
Measuring the incidence of abortion and its root cause, unintended pregnancy, remains a central goal because of the importance of having accurate estimates of these outcomes for better planning and monitoring of reproductive health and service needs. And where abortion is occurring clandestinely for legal or social reasons, having accurate estimates will help to determine the extent to which unsafe abortions might be contributing to maternal mortality and morbidity. Currently, abortion is the most elusive component of unintended pregnancy because of difficulty measuring it. Having an accurate measure of abortion is essential for developing a reliable measure of unintended pregnancy: And as a corollary, assessment of existing methodologies for estimating abortion incidence is an essential step towards further improvement in measurement.
Furthermore, any methodology that aims to accurately measure abortion incidence must be dynamic and flexible to accommodate the changing environment surrounding abortion elicited by legal reform and technological advancement, such as the use of misoprostol as an abortifacient. The situation is likely to be in flux for several years to come, given countries’ changes in abortion laws and regulations and the increasing quest for safer abortion services. In light of the above needs, efforts to improve existing methods of measuring abortion incidence, direct and indirect, remain critical. Ideally, methodologies would produce comparable and reliable estimates of abortion incidence across countries, over time and in changing contexts. The AICM methodology deserves serious consideration as an indirect estimation method, given its application in many developing countries with restrictive abortion laws over the past three decades, and the adaptations made in response to changing legal and service provision environments.
Strength of the AICM Methodology
This methodology has some important advantages. One key advantage is its adaptability to different conditions across countries and to changing conditions of abortion provision over time. An example of this is the recent incorporation of medication abortion to respond to the steady increase in use of this method in restrictive legal contexts. Another example is the incorporation of questions to develop separate estimates of abortion incidence according to whether the abortion is performed by legal/approved and illegal/non-approved providers.
In a country where medication abortion is widely used and the abortion law has been expanded, resulting in both legal and illegal abortions being practiced, it is possible to combine the two adaptations. While this is yet to be done, the success of applying each of the adaptations on its own indicates that the two can be implemented simultaneously. In such contexts, the HPS would integrate questions on the three categories of methods and approved/non-approved providers to collect information for calculating the multiplier. This will enable researchers to calculate multipliers to estimate the total number of illegal abortions. In addition, the HFS would obtain data on the number of legal abortions provided and on the PAC caseload.
Besides providing estimates of abortion incidence (the number and annual rate of induced abortions) nationally and for major regions, the AICM method also provides estimates of an important indicator of abortion morbidity—that is, the annual rate of treatment for induced abortion complications per 1000 women. A further advantage of AICM studies is that they permit estimation of the incidence of unintended pregnancy and of pregnancy overall, since the other major components of these measures are usually available in community-based surveys such as the DHS.
For many years, the AICM has also been relied on as an essential source of country level inputs into global models that estimate the incidence of abortion and unintended pregnancy for all regions and subregions and the world (Sedgh et al. 2016; World Health Organization 2011). Their contribution is important, particularly because a large number of countries have restrictive abortion laws and lack data on abortion incidence. By strengthening global estimates, country-specific AICM studies contribute to policymaking, program planning, and advocacy at the global and regional levels.
Challenges and Limitations of the AICM Method
There are several challenges when applying the AICM approach. Some can be addressed or minimized when the study is being designed. One challenge is the completeness of coverage of the Health Facility Survey, which depends on availability of up-to-date listings of all facilities that may provide postabortion care (and/or legal abortion services in countries where this is relevant). In some countries, lists of private facilities are not available: This can be addressed by undertaking additional fieldwork to conduct a listing exercise in a representative selection of areas of the country. Another challenge is political instability or civil unrest in some parts of the county that prevents data collection in those areas: This calls for adjustment in the calculation of incidence estimates to reflect these coverage constraints. In addition, terminology (and concepts in general), must be adapted for each country to ensure the quality of the data collected. Some terms have multiple interpretations; for example, complication, inpatient and average month could mean different things in different countries, and questionnaires must be adapted accordingly.
In the case of the HPS, in some countries it is hard to find a sufficient number of people who are highly knowledgeable about abortion provision, which is a prerequisite for answering questions concerning the proportions of women obtaining abortions by type of providers, the likelihood of complications and the likelihood of getting care when women experience complications. Recent AICM studies have expanded the types of medical providers to include nurses and similar mid-level professionals, as it became clear that this cadre of providers are likely to have close knowledge of abortion conditions because of their more extensive interaction with patients and closer proximity to their communities compared with physicians, for example. HPS respondents may have trouble providing needed estimates of proportions and probabilities: Finding skilled interviewers who are knowledgeable about abortion and providing adequate training is essential for addressing this type of challenge.
Some limitations of the AICM methodology are inherent in the type of data collected, and some result from evidence gaps (e.g., new studies are needed to validate certain assumptions): These types of limitations can be addressed by broadening the AICM to collect additional data or by new research studies. For example, the method does not provide data on individual women, such as their background characteristics or details about their abortion complications; it only provides aggregate estimates. These limitations can be addressed by conducting additional surveys, such as a Prospective Morbidity Survey, which collects data on women treated for abortion complications (or obtaining legal abortions) in formal health facilities, or through quantitative or qualitative community-based studies of women.
Another limitation of AICM estimates of abortion incidence is that they are approximate estimates. The early AICM studies used a simple approach to establish a range around the multiplier, by adding and subtracting one unit (e.g., if the estimated multiplier was 4, the range was based on multipliers of 3 and 5). More recently, researchers improved the approach by using estimates of the confidence interval around the number of women treated for abortion complications, which was feasible given the representative sample design used by HFS surveys. Examples include: Bangladesh (Singh et al. 2012), Pakistan (Sathar et al. 2014), Malawi (Polis et al. 2017) and Ethiopia (Moore et al. 2016). The HPS survey is based on a purposive sample of respondents, and until recently, a statistical approach for estimating confidence intervals around the multiplier had not yet been developed. However, the Zimbabwe study developed a bootstrapping approach to estimate bounds around the multiplier, and used this approach to estimate a range around abortion incidence (Sully et al. 2018b).
Key assumptions—concerning the proportion of all pregnancies that end in miscarriage and the proportion of miscarriages that occur at later gestations—are based on relatively old clinical studies because of the lack of recent studies. Also, empirical data are lacking on the proportion of women who obtain care at health facilities among those experiencing miscarriages, and how this may vary by gestation. As a result, the AICM uses an assumption that women experiencing miscarriages in the second trimester are likely to be treated at health facilities, and that the proportion of such women who get care in facilities is approximately equal to the proportion of women who deliver in facilities. (As discussed earlier, an adjustment is made in contexts where some women do not deliver in a facility for cultural reasons, but would likely seek care for a later-term miscarriage). While these assumptions are plausible and based on available information, the methodology would be greatly strengthened if it were to draw on a solid evidence base. Substantial evidence gaps need to be addressed by entirely new research efforts.
Areas Needing Further Research
Additional research is needed to measure whether women are using misoprostol correctly; the extent to which women have accurate information on use, side effects and complications; about the safety/risk of abortion complications due to incorrect use of misoprostol; and misoprostol literacy. The increasing use of misoprostol can affect abortion estimates in two ways: (a) underestimating the total number of induced abortions if the true proportion of all induced abortions that are self-induced with misoprostol goes undocumented; and (b) increasing temporary abortion morbidity treated in health facilities, a crucial input of the AICM method. The temporary increase in hospital admissions of women with abortion complications are more likely related to women having inadequate information about how the medication works, what the signs of complications are, when to seek medical care, and for confirming the pregnancy has ended. As a result, we hypothesize that many women are seeking care in health facilities because of fear of bleeding, which is part of the process of the method, not a health risk.
At present, it is difficult to know with precision the degree of correct use of medical abortion, particularly misoprostol. Additional research is necessary to measure whether women are using misoprostol (or the combined medication abortion method) according to protocol, and the risk of abortion complications due to incorrect use of these methods.
New research is also needed on the proportion of pregnancies that end in miscarriage and the proportion of miscarriages that result in complications requiring treatment in a facility, according to gestational age. Furthermore, since the occurrence of miscarriage and the likelihood of seeking care are context-dependent, such studies should ideally be conducted in a number of socio-cultural contexts. Evidence from such studies would not only help to improve care for women who have miscarriages, but would also help to more accurately categorize women treated for complications according to whether they had an induced abortion or a miscarriage.
Conclusion
One of the key features of the AICM methodology is its proven adaptability to different conditions across countries and to changing conditions of abortion provision over time. The method has been applied in over 20 countries and has been recognized as the most robust method available to date, among the several indirect methodologies developed for estimating abortion. Studies using this methodology have contributed to the body of evidence on which global estimates of abortion incidence are based. In addition, abortion incidence estimates have provided policy makers and health planners with reliable information to make informed decisions and plans to prevent unintended pregnancies, unsafe abortions, and improve women’s reproductive health.
As discussed above, the AICM has important limitations, in particular with respect to the multiplier, which is estimated based on opinions of key informants. As a result, there is need for more work to improve on the methodology, to test other methodologies, and to scale up and apply new methodologies more widely. Some new methodologies and adaptations of older methods are currently being tested in on-going studies: This new work includes application and further development of the network scale-up method (Sully et al. 2018a), adaptation of the respondent-driven sample approach to measuring abortion incidence (Jayaweera et al. 2018; Rossier et al. 2018), and further applications of the List Experiment method to reduce underreporting (Moseson et al. 2018). In developing new methods and improving existing methods, researchers need to identify the contextual factors that make particular methods more effective in obtaining robust and accurate estimates of abortion incidence. This would provide users with a choice of methods and a basis for selecting among them in specific country contexts. Considering the high level of policy and programmatic relevance of reliable estimates of abortion incidence, continued efforts to improve the AICM method and to develop and test other methods are high priority. Wider application of existing indirect estimation methodologies and methodological research would be especially helpful in countries that have highly restrictive abortion laws and in those that have liberal laws but inadequate access to safe abortion services.
References
Bankole, A., Adewole, I. F., Hussain, R., Awolude, O., Singh, S., & Akinyemi, J. O. (2015). The incidence of abortion in Nigeria. International Perspectives on Sexual and Reproductive Health, 41(4), 170–181. https://doi.org/10.1363/4117015.
Bankole, A., et al. (2006). Unwanted pregnancy and induced abortion in Nigeria: Causes and consequences. New York: Guttmacher Institute.
Basinga, P., Moore, A. M., Singh, S. D., Carlin, E. E., Birungi, F., & Ngabo, F. (2012). Abortion incidence and postabortion care in Rwanda. Studies in Family Planning, 43(1), 11–20. https://doi.org/10.1111/j.1728-4465.2012.00298.x.
Bongaarts, J., & Potter, R. (1983). Fertility, biology, and behavior: an analysis of the proximate determinants. New York: Academic Press.
Bracken, H., Ngoc, N. T. N., Schaff, E., Coyaji, K., Ambardekar, S., Westheimer, E., et al. (2007). Mifepristone followed in 24 hours to 48 hours by misoprostol for late first-trimester abortion. Obstetrics and Gynecology, 109(4), 895–901. https://doi.org/10.1097/01.AOG.0000259319.18958.76.
Chae, S., Kayembe, P. K., Philbin, J., Mabika, C., & Bankole, A. (2017). The incidence of induced abortion in Kinshasa, Democratic Republic of Congo, 2016. PLoS ONE, 12(10), e0184389. https://doi.org/10.1371/journal.pone.0184389.
Gebrehiwot, Y., Fetters, T., Gebreselassie, H., Moore, A., Hailemariam, M., Dibaba, Y., et al. (2016). Changes in morbidity and abortion care in Ethiopia after legal reform: National results from 2008 and 2014. International Perspectives on Sexual and Reproductive Health, 42(3), 121–130. https://doi.org/10.1363/42e1916.
Gebreselassie, H., Fetters, T., Singh, S., Abdella, A., Gebrehiwot, Y., Tesfaye, S., et al. (2010). Caring for women with abortion complications in Ethiopia: National estimates and future implications. International Perspectives on Sexual and Reproductive Health, 36(1), 6–15. https://doi.org/10.1363/ipsrh.36.006.10
Grapsas, X., Liberis, V., Vassaras, G., Tsikouras, P., Vlachos, G., & Galazios, G. (2008). Misoprostol and first trimester pregnancy termination. Clinical and Experimental Obstetrics and Gynecology, 35(1), 32–34.
Harlap, S., Shiono, P., & Ramcharan, S. (1980). A life table of spontaneous abortions and the effects of age, parity, and other variables. In I. Porter & E. Hook (Eds.), Human embryonic and fetal death (pp. 145–158). New York: Academic Press.
Jayaweera R., Munoz, M., Motana, R., Bessemaar. T, & Gerdts, C. (2018). Using respondent driven sampling to measure the incidence and prevalence of informal sector abortion: A methodological assessment. Paper presented at IUSSP seminar on “Incidence and Safety of Abortion: New Evidence and Improvements in Measurement, Watamu, Kenya.
Juarez, F., Cabigon, J., & Singh, S. (2010). The sealed envelope method of estimating induced abortion: How much of an improvement? In S. Singh, L. Remez, & A. Tartaglione (Eds.), Methodologies for estimating abortion incidence and abortion-related morbidity: A review (pp. 107–123). New York and Paris: Guttmacher Institute and International Union for the Scientific Study of Population.
Keogh, S. C., Kimaro, G., Muganyizi, P., Philbin, J., Kahwa, A., Ngadaya, E., et al. (2015). Incidence of induced abortion and post-abortion care in Tanzania. PLoS ONE, 10(9), e0133933. https://doi.org/10.1371/journal.pone.0133933.
Lara, D., Strickler, J., Diaz Olavarrieta, C., & Ellertson, C. (2004). Measuring induced abortion in Mexico: A comparison of four methodologies. Sociological Methods & Research, 32(4), 529–558.
Madziyire, M. G., Polis, C. B., Riley, T., Sully, E. A., Owolabi, O., & Chipato, T. (2018). Severity and management of postabortion complications among women in Zimbabwe, 2016: A cross-sectional study. BMJ Open, 8(2), e019658. https://doi.org/10.1136/bmjopen-2017-019658.
Middleton, T., Schaff, E., Fielding, S. L., Scahill, M., Shannon, C., Westheimer, E., et al. (2005). Randomized trial of mifepristone and buccal or vaginal misoprostol for abortion through 56 days of last menstrual period. Contraception, 72(5), 328–332. https://doi.org/10.1016/j.contraception.2005.05.017.
Miller, J., Cisin, I., & Harrel, A. (1986). A new technique for surveying deviant behavior: item count estimates of marijuana, cocaine, and heroin. Presented at the American Association of Public Research Conference, St. Petersberg, FL.
Mohamed, S. F., Izugbara, C., Moore, A. M., Mutua, M., Kimani-Murage, E. W., Ziraba, A. K., et al. (2015). The estimated incidence of induced abortion in Kenya: a cross-sectional study. BMC Pregnancy and Childbirth, 15, 185. https://doi.org/10.1186/s12884-015-0621-1.
Moore, A. M., Gebrehiwot, Y., Fetters, T., Dibaba Wado, Y., Bankole, A., Singh, S., et al. (2016). The estimated incidence of induced abortion in Ethiopia, 2014: Changes in the provision of services since 2008. International Perspectives on Sexual and Reproductive Health, 42(3), 111–120. https://doi.org/10.1363/42e1816.
Moseson, H., Jayaweera, R., Norris, A., Huber, S., Garver, S., & Gerdts, C. (2018). Two test applications of the List Experiment method to reduce under-reporting of abortion: Results from Malawi and Senegal. Paper presented at IUSSP seminar on “Incidence and Safety of Abortion: New Evidence and Improvements in Measurement”. Watamu, Kenya.
Moseson, H., Massaquoi, M., Dehlendorf, C., Bawo, L., Dahn, B., Zolia, Y., et al. (2015). Reducing under-reporting of stigmatized health events using the List Experiment: Results from a randomized, population-based study of abortion in Liberia. International Journal of Epidemiology, 44(6), 1951–1958. https://doi.org/10.1093/ije/dyv174.
Oliveras, E., & Letamo, G. (2010). Examples of methods to address underreporting of induced abortion: preceding birth technique and randomized response technique. In S. Singh, L. Remez, & A. Tartaglione (Eds.), Methodologies for estimating abortion incidence and abortion-related morbidity: a review (pp. 63–70). New York and Paris: Guttmacher Institute and International Union for the Scientific Study of Population.
Polis, C. B., Mhango, C., Philbin, J., Chimwaza, W., Chipeta, E., & Msusa, A. (2017). Incidence of induced abortion in Malawi, 2015. PLoS ONE, 12(4), e0173639. https://doi.org/10.1371/journal.pone.0173639.
Prada, E., Atuyambe, L. M., Blades, N. M., Bukenya, J. N., Orach, C. G., & Bankole, A. (2016). Incidence of induced abortion in Uganda, 2013: new estimates since 2003. PLoS ONE, 11(11), e0165812. https://doi.org/10.1371/journal.pone.0165812.
Prada, E., Biddlecom, A., & Singh, S. (2011). Induced abortion in Colombia: new estimates and change between 1989 and 2008. International Perspectives on Sexual and Reproductive Health, 37(3), 114–124. https://doi.org/10.1363/3711411.
Puri, M., Regmi, S., Tamang, A., & Shrestha, P. (2014). Road map to scaling-up: translating operations research study’s results into actions for expanding medical abortion services in rural health facilities in Nepal. Health Research Policy and Systems, 12, 24. https://doi.org/10.1186/1478-4505-12-24.
Puri, M., Singh, S., Sundaram, A., Hussain, R., Tamang, A., & Crowell, M. (2016). Abortion incidence and unintended pregnancy in Nepal. International Perspectives on Sexual and Reproductive Health, 42(4), 197–209. https://doi.org/10.1363/42e2116.
Rastegari, A., Baneshi, M. R., Haji-maghsoudi, S., Nakhaee, N., Eslami, M., Malekafzali, H., et al. (2014). Estimating the annual incidence of abortions in Iran applying a Network Scale-up Approach. Iranian Red Crescent Medical Journal, 16(10), e15765. https://doi.org/10.5812/ircmj.15765.
Remez, L., Singh, S., & Tartaglione, A. (2010). Introduction. In S. Singh, L. Remez, & A. Tartaglione (Eds.), Methodologies for estimating abortion incidence and abortion-related morbidity: A review. New York and Paris: Guttmacher Institute and International Union for the Scientific Study of Population.
Rossier, C. (2003). Estimating induced abortion rates: a review. Studies in Family Planning, 34(2), 87–102.
Rossier, C., Feehan, D., & Owolabi, O. (2018). A multiplex RDS for abortion? Assessing the potential of the Respondent-Driven Sampling to study abortion safety in restrictive contexts. Paper presented at IUSSP seminar on “Incidence and Safety of Abortion: New Evidence and Improvements in Measurement”. Watamu, Kenya.
Rossier, C., Guiella, G., Ouédraogo, A., & Thiéba, B. (2006). Estimating clandestine abortion with the confidants method—results from Ouagadougou Burkina Faso. Social Science & Medicine, 62(1), 254–266. https://doi.org/10.1016/j.socscimed.2005.05.024.
Sathar, Z., Singh, S., Rashida, G., Shah, Z., & Niazi, R. (2014). Induced abortions and unintended pregnancies in Pakistan. Studies in Family Planning, 45(4), 471–491. https://doi.org/10.1111/j.1728-4465.2014.00004.x.
Sedgh, G., Bearak, J., Singh, S., Bankole, A., Popinchalk, A., Ganatra, B., et al. (2016). Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet, 388(10041), 258–267. https://doi.org/10.1016/S0140-6736(16)30380-4.
Sedgh, G., Rossier, C., Kaboré, I., Bankole, A., & Mikulich, M. (2011). Estimating abortion incidence in Burkina Faso using two methodologies. Studies in Family Planning, 42(3), 147–154.
Sedgh, G., Sylla, A. H., Philbin, J., Keogh, S., & Ndiaye, S. (2015). Estimates of the incidence of induced abortion and consequences of unsafe abortion in Senegal. International Perspectives on Sexual and Reproductive Health, 41(1), 11–19. https://doi.org/10.1363/4101115.
Singh, S., Fetters, T., Gebreselassie, H., Abdella, A., Gebrehiwot, Y., Kumbi, S., et al. (2010). The estimated incidence of induced abortion in Ethiopia, 2008. International Perspectives on Sexual and Reproductive Health, 36(1), 16–25. https://doi.org/10.1363/ipsrh.36.016.10.
Singh, S., Hossain, A., Maddow-Zimet, I., Ullah Bhuiyan, H., Vlassoff, M., & Hussain, R. (2012). The incidence of menstrual regulation procedures and abortion in Bangladesh, 2010. International Perspectives on Sexual and Reproductive Health, 38(3), 122–132. https://doi.org/10.1363/3812212.
Singh, S., Hossain, A., Maddow-Zimet, I., Vlassoff, M., Bhuiyan, H. U., & Ingerick, M. (2017). The incidence of menstrual regulation procedures and abortion in Bangladesh, 2014. International Perspectives on Sexual and Reproductive Health. https://doi.org/10.1363/43e2417.
Singh, S., Remez, L., Sedgh, G., Kwok, L., & Onda, T. (2018). Abortion worldwide 2017: Uneven progress and unequal access. New York: Guttmacher Institute.
Singh, S., Remez, L., & Tartaglione, A. (Eds.). (2010b). Methodologies for estimating abortion incidence and abortion-related morbidity: A review. New York and Paris: Guttmacher Insttute and International Union for the Scientific Study of Population.
Singh, S., & Wulf, D. (1994). Estimated levels of induced abortion in six Latin American countries. International Family Planning Perspectives, 20(1), 4–13. https://doi.org/10.2307/2133331.
Singh, S., et al. (2006). Unintended Pregnancy and Induced Abortion in the Philippines: Causes and Consequences. New York: Guttmacher Institute.
Sully, E., & Giorgio, M., (2018a). Estimating abortion incidence using the Network Scale-Up Method. Paper presented at IUSSP seminar on “Incidence and Safety of Abortion: New Evidence and Improvements in Measurement”. Watamu, Kenya
Sully, E. S., Madziyire, M. G., Riley, T., Moore, A. M., Crowell, M., Nyandoro, M. T., et al. (2018). The incidence of induced abortion in Zimbabwe, 2016. PLoS ONE, 13(10), e0205239. https://doi.org/10.1371/journal.pone.0205239.
World Health Organization. (2011). Unsafe abortion global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. Geneva: World Health Organization.
Yeatman, S., & Trinitapoli, J. (2011). Best-friend reports: A tool for measuring the prevalence of sensitive behaviors. American Journal of Public Health, 101(9), 1666–1667. https://doi.org/10.2105/AJPH.2011.300194.
Zamudio, L., Rubiano, N., & Wartenberg, L. (1999). The incidence and social and demographic characteristics of abortion in Colombia. In A. I. Mundigo & C. Indriso (Eds.), Abortion in the developing world (pp. 407–446). New Delhi: Vistaar Publications.
Ziraba, A. K., Izugbara, C., Levandowski, B. A., Gebreselassie, H., Mutua, M., Mohamed, S. F., et al. (2015). Unsafe abortion in Kenya: a cross-sectional study of abortion complication severity and associated factors. BMC Pregnancy and Childbirth, 15, 34. https://doi.org/10.1186/s12884-015-0459-6.
Acknowledgements
The authors are grateful to Lorraine Kwok for research support and to Suzette Audam, Nakeisha Blades, Ann Moore, Jesse Philbin, Zoe Pleasure and Taylor Riley for their assistance with data analysis. This article has been made possible by UK Aid from the UK Government. The views expressed are those of the authors and do not necessarily reflect the positions and policies of the UK Government.
Funding
This article has been made possible by UK Aid from the UK Government (Grant Number 203177–101).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Singh, S., Juarez, F., Prada, E. et al. Estimating Abortion Incidence: Assessment of a Widely Used Indirect Method. Popul Res Policy Rev 38, 429–458 (2019). https://doi.org/10.1007/s11113-019-09517-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11113-019-09517-2