Abstract
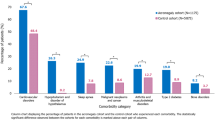
The economic burden of acromegaly in the US has been largely unknown. We describe the prevalence of treatment patterns, complication rates, and associated healthcare utilization and costs of acromegaly in the US. Patients were identified between 1/1/2002 and 12/31/2009 in claims databases. During 1-year after each continuously-enrolled patient’s first acromegaly claim, pharmacy and medical claims were used to estimate outcomes. Regression models were used to adjust outcomes. There were 2,171 acromegaly patients (mean age: 45.3 years; 49.7 % female); 77.8 % received the majority of their care from non-endocrinologists. Pharmacologic treatment was used by 30.8 % of patients: octreotide-LAR in 18.6 %, dopamine agonists in 9.8 %, short-acting octreotide in 4.7 %, pegvisomant in 4.1 %, and lanreotide in 1.2 %; 56 % had biochemical monitoring. Comorbidities were common, ranging from 6.6 % (colon neoplasms) to 25.6 % (musculoskeletal abnormalities). Mean healthcare costs were $24,900. Adjusted analyses indicated comorbidities increased the odds of hospitalization: by 76 % for musculoskeletal abnormalities; 193 % for cardiovascular abnormalities; and 56 % for sleep apnea (p < 0.05). Odds of emergency department visits increased by 87 % (musculoskeletal) and 132 % (cardiovascular abnormalities) (p < 0.01). After adjustments, colon neoplasms were associated with $8,401 mean increase in costs; musculoskeletal abnormalities with $7,502, cardiovascular abnormalities with $13,331, sleep apnea with $10,453, and hypopituitarism with $6,742 (p < 0.01). Complications are common and increase utilization and cost in acromegaly patients. Cardiovascular complications nearly tripled the odds of hospitalization (OR 2.93) and increased annual mean cost by $13,331. Adequate management of this disease may be able to reduce health care utilization and cost associated with these complications and with acromegaly in general.
Similar content being viewed by others
References
Ben-Shlomo A, Sheppard M, Stephens J, Pulgar S, Melmed S (2011) Clinical, quality of life, and economic value of acromegaly disease control. Pituitary 14(3):284–294
Melmed S (2006) Medical progress: acromegaly. N Engl J Med 355(24):2558–2573
Chanson P, Salenave S, Kamenicky P et al (2009) Acromegaly. Best Pract Res Clin Endocrinol Metab 23(5):555–574
Dekkers O, Biermasz N, Pereira A, Romijn J, Vandenbroucke J (2008) Mortality in acromegaly: a metaanalysis. J Clin Endocrinol Metab 93(1):61–67
Colao A, Ferone D, Marzullo P, Lombardi G (2004) Systemic complications of acromegaly: epidemiology, pathogenesis, and management. Endocr Rev 25(1):102–152
O’Malley A, Pham H, Schrag D, Wu B, Bach P (2007) Potentially avoidable hospitalizations for COPD and pneumonia: the role of physician and practice characteristics. Med Care 45:562–570
Agency for Healthcare Research and Quality (AHRQ): HCUP Chronic Condition Indicator. Healthcare Cost and Utilization Project (HCUP). AHRQ. www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. Accessed 5 Sep 2012
Hwang W, Heller W, Ireys H, Anderson G (2001) Out-of-pocket medical spending for care of chronic conditions. Health Aff 20:267–278
Charlson M, Pompei P, Ales K, MacKenzie C (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Ezzat S, Serri O, Chik CL et al (2006) Canadian consensus guidelines for the diagnosis and management of acromegaly. Clin Invest Med 29(1):29–39
Burton T, Le Nestour E, Bancroft T, Neary M (2013) Real-world comorbidities and treatment patterns of patients with acromegaly in two large US health plan databases. Pituitary 16(3):354–362
Katznelson L, Atkinson J, Cook D, Ezzat S, Hamrahian A, Miller K (2011) AACE Acromegaly Task Force. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Diagnosis and Treatment of Acromegaly—2011 update. Endocr Pract 17(4):1–44
Wier L, Pfuntner A, Maeda J, Stranges E, Ryan K, Jagadish P, Collins Sharp B, Elixhauser A (2011) HCUP facts and figures: statistics on hospital-based care in the United States, 2009. Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/reports.jsp. Accessed 17 Oct 2012
Didoni G, Grottol S, Gasco V et al (2004) Cost-of-illness study in acromegalic patients in Italy. J Endocrinol Invest 27(11):1034–1039
Wilson L, Shin J, Ezzat S (2001) Longitudinal assessment of economic burden and clinical outcomes in acromegaly. Endocr Pract 7(3):170–180
Knutzen R, Ezzat S (2006) The cost of medical care for the acromegalic patient. Neuroendocrinology 83:139–144
Tyree P, Lind B, Lafferty W (2006) Challenges of using medical insurance claims data for utilization analysis. Am J Med Qual 21(4):269–275
Acknowledgments
Funding for this study was provided by Novartis Pharmaceuticals Corporation.
Conflict of interest
This study was funded by Novartis Pharmaceuticals Corporation. Financial relationships with the organization that sponsored the research is as follows: Laurence Katznelson has been a consultant for Novartis Pharmaceuticals Corporation; Maureen Neary is an employee of Novartis Pharmaceuticals Corporation; and Michael S. Broder, Eunice Chang, and Dasha Cherepanov are employees of Partnership for Health Analytic Research, LLC, a health services research company, which received funding for this research.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Broder, M.S., Neary, M.P., Chang, E. et al. Treatments, complications, and healthcare utilization associated with acromegaly: a study in two large United States databases. Pituitary 17, 333–341 (2014). https://doi.org/10.1007/s11102-013-0506-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-013-0506-0