Abstract
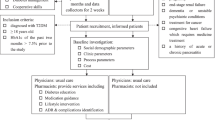
Background Diabetes mellitus is a complex multi-system disorder, requiring multi-disciplinary care. The conventional care model, where physicians are the sole caregivers may not be optimal. Addition of other healthcare team members improves healthcare outcomes for patients with diabetes. Aim To evaluate the impact of pharmacist-involved collaborative care on diabetes-related outcomes among patients with diabetes attending a primary healthcare setting in Qatar using real-world data. Method A retrospective cohort study was conducted among patients with diabetes attending Qatar Petroleum Diabetes Clinic. Patients were categorized as either receiving pharmacist-involved collaborative care (intervention group) or usual care (control group). Data were analyzed using SPSS®. Glycemic control (glycated hemoglobin A1c, HbA1c), blood pressure, lipid profile, and body mass index were evaluated at baseline and up to 17 months of follow-up. Results After 17 months of follow-up, pharmacist-involved collaborative care compared to usual care resulted in a significant decrease in HbA1c (6.8 ± 1.2% vs. 7.1 ± 1.3%, p < 0.01). Moreover, compared to baseline, pharmacist-involved collaborative care significantly improved (p < 0.05) the levels of HbA1c (7.5% vs. 6.8%), low-density lipoprotein cholesterol (3.7 mmol/L vs. 2.8 mmol/L), total cholesterol (5.43 mmol/L vs. 4.34 mmol/L), and body mass index (30.42 kg/m2 vs. 30.17 kg/m2) after 17 months within the intervention group. However, no significant changes for these parameters occurred within the control group. Conclusion The implementation of pharmacist-involved collaborative care in a primary healthcare setting improved several diabetes-related outcomes over 17 months. Future studies should determine the long-term impact of this care model.


Similar content being viewed by others
Availability of data and material
Data support published claims.
References
Schmidt AM. Highlighting diabetes mellitus: the epidemic continues. Arterioscler Thromb Vasc Biol. 2018;38(1):e1–8.
Rhys W, Colagiuri S, Almutairi R, et al. IDF Diabetes Atlas ninth edition. International Diabetes Federation; 2019. ISBN: 978-2-930229-87-4
Internaltional Diabetes Federation. IDF diabetes atlas [Internet]. 2013 [cited 2019 Oct 12]. p. 12. www.idf.org/diabetesatlas
Saudek CD. The role of primary care professionals in managing diabetes. Clin Diabetes. 2002;20:65–6.
World Health Organization. The top 10 causes of death [Internet]. 2018 [cited 2019 Dec 5]. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
DeLoach C. The Impact of Interprofessional Collaboration on Diabetes Outcomes in Primary Care Settings. Dissertation. Walden University; 2018.
Baptista DR, Wiens A, Pontarolo R, et al. The chronic care model for type 2 diabetes: a systematic review. Diabetol Metab Syndr. 2016;8:1–7.
Daiski I. An expanded model of diabetes care based in an analysis and critique of current approaches. J Clin Nurs. 2008;17:310–7.
Noor Abdulhadi NM, Al-Shafaee MA, Wahlström R, et al. Doctors’ and nurses’ views on patient care for type 2 diabetes: an interview study in primary health care in Oman. Prim Heal Care Res Dev. 2013;14:258–69.
Schwartz DD, Stewart SD, Aikens JE, et al. Seeing the person, not the illness: Promoting diabetes medication adherence through patient-centered collaboration. Clin Diabetes. 2017;35:35–42.
Johnson JM, Carragher R. Interprofessional collaboration and the care and management of type 2 diabetic patients in the Middle East: A systematic review. J Interprof Care. 2018;32:621–8.
Gucciardi E, Espin S, Morganti A, et al. Exploring interprofessional collaboration during the integration of diabetes teams into primary care. BMC Fam Pract. 2016;17:12.
Abdulrhim S, Sankaralingam S, Ibrahim M, et al. The impact of pharmacist care on diabetes outcomes in primary care settings: An umbrella review of published systematic reviews. Prim Care Diabetes. 2020;14:393–400.
Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28:421–36.
Machado M, Bajcar J, Guzzo GC, et al. Sensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes management. Ann Pharmacother. 2007;41:1569–82.
Lee JK, McCutcheon RM, Fazel MT, et al. Assessment of interprofessional collaborative practices and outcomes in adults with diabetes and hypertension in primary care: a systematic review and meta-analysis. JAMA Netw Open. 2021. https://doi.org/10.1001/jamanetworkopen.2020.36725.
Nogueira M, Otuyama LJ, Rocha PA, et al. Pharmaceutical care-based interventions in type 2 diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials. Einstein (Sao Paulo). 2020;18:eRW4686. https://doi.org/10.31744/einstein_journal/2020RW4686
Hughes J, Wibowo Y, Sunderland B, et al. The role of the pharmacist in the management of type 2 diabetes: current insights and future directions. Integr Pharm Res Pract. 2017;6:15–27.
Simpson SH, MacCallum L, Mansell K. Pharmacy practice and diabetes care. Can J Diabetes. 2017;41:549–50.
Yu J, Shah BM, Ip EJ, et al. A Markov model of the cost-effectiveness of pharmacist care for diabetes in prevention of cardiovascular diseases: evidence from Kaiser Permanente Northern California. J Manag Care Pharm. 2013;19:102–14.
Nau DP, Pacholski AM. Impact of pharmacy care services on patients’ perceptions of health care quality for diabetes. J Am Pharm Assoc. 2007;47:358–65.
Fazel MT, Bagalagel A, Lee JK, et al. Impact of diabetes care by pharmacists as part of health care team in ambulatory settings: a systematic review and meta-analysis. Ann Pharmacother. 2017;51:890–907.
Madden J, Barnard A, Owen C. Utilisation of multidisciplinary services for diabetes care in the rural setting. Aust J Rural Health. 2013;21:28–34.
Pannick S, Davis R, Ashrafian H, et al. Effects of interdisciplinary team care interventions on general medical wards: a systematic review. JAMA Intern Med. 2015;175:1288–98.
Najarian J, Bartman K, Kaszuba J, et al. Improving glycemic control in the acute care setting through nurse education. J Vasc Nurs. 2013;31:150–7.
Grembowski D, Paschane D, Diehr P, et al. Managed care, physician job satisfaction, and the quality of primary care. J Gen Intern Med. 2005;20:271–7.
Conca T, Saint-Pierre C, Herskovic V, et al. Multidisciplinary collaboration in the treatment of patients with type 2 diabetes in primary care: analysis using process mining. J Med Internet Res. 2018;20:e127.
Saint-Pierre C, Herskovic V, Sepúlveda M. Multidisciplinary collaboration in primary care: a systematic review. Fam Pract. 2018;35:132–41.
Faul F, Erdfelder E, Buchner A, et al. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60.
Cranor CW, Christensen DB. The Asheville project: Short-term outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (2003). 2012;52:838–50.
Cranor CW, Bunting BA, Christensen DB. The Asheville project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (Wash). 2003;43:173–84.
Wishah RA, Al-Khawaldeh OA, Albsoul AM. Impact of pharmaceutical care interventions on glycemic control and other health-related clinical outcomes in patients with type 2 diabetes: Randomized controlled trial. Diabetes Metab Syndr. 2015;9:271–6.
Passarella P, Kiseleva TA, Valeeva FV, et al. Hypertension management in diabetes: 2018 update. Diabetes Spectr. 2018;31:218–24.
Al Mazroui NR, Kamal MM, Ghabash NM, et al. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67:547–57.
Choe HM, Mitrovich S, Dubay D, et al. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11:253–60.
Santschi V, Chiolero A, Paradis G, et al. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2012;35:2706–17.
Davis CS, Ross LAR, Bloodworth LS. The impact of clinical pharmacist integration on a collaborative interdisciplinary diabetes management team. J Pharm Pract. 2017;30:286–90.
Renfro C, Ferreri S, Barber T, et al. Development of a communication strategy to increase interprofessional collaboration in the outpatient setting. Pharmacy (Basel). 2018;6:4.
Congdon HB, Eldridge BH, Truong H, et al. Development and implementation of a navigator-facilitated care coordination algorithm to improve clinical outcomes of underserved latino patients with uncontrolled diabetes. J Health Care Poor Underserved. 2013;24:1604–13.
Mohamed H, Al-Lenjawi B, Amuna P, et al. Culturally sensitive patient-centred educational programme for self-management of type 2 diabetes: a randomized controlled trial. Prim Care Diabetes. 2013;7:199–206.
Cander S, Gül Ö, Gül CB, et al. Re-training of type 2 diabetic patients for better adherence to diabetes care plan in oral anti-diabetics and plus insulin treatment groups. Turk JEM. 2015;19:49–54.
Deters MA, Laven A, Castejon A, et al. Effective interventions for diabetes patients by community pharmacists: A meta-analysis of pharmaceutical care components. Ann Pharmacother. 2018;52:198–211.
van Eikenhorst L, Taxis K, van Dijk L, et al. Pharmacist-led self-management interventions to improve diabetes outcomes. A systematic literature review and meta-analysis. Front Pharmacol. 2017;8:891.
Bener A, Abdulmalik M, Al-Kazaz M, et al. Medical audit of the quality of diabetes care: is primary care more successful than hospitals? J Prim Care Community Health. 2012;3:42–50.
Blonde L, Khunti K, Harris SB, et al. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35:1763–74.
Mochtar I, Al-Monjed MF. Is diabetes management in primary care improving clinical outcomes? A study in Qatar. East Mediterr Health J. 2015;21:239–45.
Jahangard-Rafsanjani Z, Sarayani A, Nosrati M, et al. Effect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trial. Diabetes Educ. 2015;41:127–35.
Al AdAwi RM, Stewart D, Ryan C, et al. A systematic review of pharmacist input to metabolic syndrome screening, management and prevention. Int J Clin Pharm. 2020;42:995–1015.
Greenfield S. Making real-world evidence more useful for decision making. Value Heal. 2017;20:1023–4.
Berger ML, Sox H, Willke R, et al. Good practices for real-world data studies of treatment and/or comparative effectiveness: Recommendations from the joint ISPOR-ISPE special task force on real-world evidence in health care decision making. Value Health. 2017;20:1003–1008.
Ye S, Krupka DJ, Davidson KW. Diagnosing medication non-adherence in a patient with myocardial infarction. Front Psychol. 2012;3:267
Acknowledgements
The authors would like to express their sincere thanks to Qatar Petroleum (QP) Health Department and QP Medical Center Dukhan, for providing us with the permission and all the required resources to conduct this project. We would also like to thank all healthcare providers and patients at the diabetes clinic who participated in the study and for sharing their lived experiences in Phase 2 of the study.
Funding
The authors acknowledge Qatar University for funding the research through the Office of Research Support grant numbers QUST-2-CPH-2019-1 and QUST-2-CPH-2018-12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Qatar Petroleum Health Department and Qatar University Institutional Review Board (QU-IRB) approved the research protocol and and the associated data collection tools (Approval number: QU-IRB 1067-E/19). Confidentiality of patients’ data was maintained, and there was no disclosure of any identifiers. No patient consent was required in this study as it involved retrospective data collection without any patient interaction.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abdulrhim, S., Awaisu, A., Ibrahim, M.I.M. et al. Impact of pharmacist-involved collaborative care on diabetes management in a primary healthcare setting using real-world data. Int J Clin Pharm 44, 153–162 (2022). https://doi.org/10.1007/s11096-021-01327-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-021-01327-x