Abstract
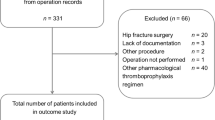
Background The risk of venous thromboembolism following major orthopaedic surgery is among the highest for all surgical specialties. Our hospital guidelines for thromboprophylaxis following elective primary total hip or knee replacement are based on American College of Chest Physicians guidance. The most recent change to local guidelines was the introduction of the extended aspirin regimen as standard thromboprophylaxis. Objective To establish the appropriateness of this regimen by comparing venous thromboembolism rates in patients receiving extended aspirin to previous regimens. Setting The largest dedicated orthopaedic hospital in Ireland. Methods This was a retrospective cohort study. Data were collected from patient record software. All eligible patients undergoing primary total hip or knee replacement between 1st January 2010 and 30th June 2016 were included. Main outcome measure Venous thromboembolism up to 6 months post-operatively. Results Of the 6548 participants (55.3% female, mean age 65.4 years (± 11.8 years, 55.8% underwent total hip replacement), venous thromboembolism occurred in 65 (0.99%). Venous thromboembolism rate in both the inpatient enoxaparin group (n = 961) and extended aspirin group (n = 3460) was 1.04% and was 0.66% in the modified rivaroxaban group (n = 1212). Non-inferiority analysis showed the extended aspirin regimen to be equivalent to the modified rivaroxaban regimen. History of venous thromboembolism was the only significant demographic risk factor for post-operative venous thromboembolism (0.87% vs. 3.54%, p = 0.0002). Conclusion In daily clinical practice, extended aspirin regimen is at least as effective as modified rivaroxaban for preventing clinically important venous thromboembolism among patients undergoing hip or knee arthroplasty who are discharged from the hospital without complications. Aspirin can be considered a safe and effective agent in the prevention of venous thromboembolism after total hip or total knee replacement.


Similar content being viewed by others
References
Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2_suppl):e278S–325S. https://doi.org/10.1378/chest.11-2404.
Anderson DR, Dunbar MJ, Bohm ER, Belzile E, Kahn SR, Zukor D, et al. Aspirin versus low-molecular-weight heparin for extended venous thromboembolism prophylaxis after total hip arthroplasty: a randomized trial. Ann Intern Med. 2013;158(11):800–6. https://doi.org/10.7326/0003-4819-158-11-201306040-00004.
Bozic KJ, Vail TP, Pekow PS, Maselli JH, Lindenauer PK, Auerbach AD, et al. Does aspirin have a role in venous thromboembolism prophylaxis in total knee arthroplasty patients? J Arthroplast. 2010;25(7):1053–60. https://doi.org/10.1016/j.arth.2009.06.021.
Hamilton SC, Whang WW, Anderson BJ, Bradbury TL, Erens GA, Roberson JR. Inpatient enoxaparin and outpatient aspirin chemoprophylaxis regimen after primary hip and knee arthroplasty: a preliminary study. J Arthroplast. 2012;27(9):1594–8. https://doi.org/10.1016/j.arth.2012.02.006.
Holden DN, Maceira E. Thromboembolism prophylaxis failure rates after hip and knee arthroplasty: comparison of aspirin and anticoagulants. Curr Orthop Pract. 2015;26(3):277–80. https://doi.org/10.1097/BCO.0000000000000222.
Jameson SS, Baker PN, Charman SC, Deehan DJ, Reed MR, Gregg PJ, et al. The effect of aspirin and low-molecular-weight heparin on venous thromboembolism after knee replacement: a non-randomised comparison using National Joint Registry Data. J Bone Jt Surg Br. 2012;94(7):914–8.
Jameson SS, Charman SC, Gregg PJ, Reed MR, Van Der Meulen JH. The effect of aspirin and low-molecular-weight heparin on venous thromboembolism after hip replacement: a non-randomised comparison from information in the National Joint Registry. J Bone Jt Surg Ser B. 2011;93 B(11):1465–70. https://doi.org/10.1302/0301-620x.93b11.27622.
Parvizi J, Huang R, Restrepo C, Chen AF, Austin MS, Hozack WJ, et al. Low-dose aspirin is effective chemoprophylaxis against clinically important venous thromboembolism following total joint arthroplasty: a preliminary analysis. J Bone Jt Surg Am. 2017;99(2):91–8. https://doi.org/10.2106/JBJS.16.00147.
Pulmonary Embolism Prevention trial Collaborative Group. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: pulmonary embolism prevention (PEP) trial. Lancet. 2000;355(9212):1295–302.
Rath NK, Goodson MW, White SP, Forster MC. The use of rivaroxaban for chemical thromboprophylaxis following total knee replacement. Knee. 2013;20(6):397–400. https://doi.org/10.1016/j.knee.2013.01.006.
Anderson DR, Dunbar M, Murnaghan J, Kahn SR, Gross P, Forsythe M, et al. Aspirin or rivaroxaban for VTE prophylaxis after hip or knee arthroplasty. N Engl J Med. 2018;378(8):699–707. https://doi.org/10.1056/NEJMoa1712746.
Faour M, Piuzzi NS, Brigati DP, Klika AK, Mont MA, Barsoum WK, et al. Low-dose aspirin is safe and effective for venous thromboembolism prophylaxis following total knee arthroplasty. J Arthroplast. 2018;33(7):S131–5. https://doi.org/10.1016/j.arth.2018.03.001.
Charters MA, Frisch NB, Wessell NM, Dobson C, Les CM, Silverton CD. Rivaroxaban versus enoxaparin for venous thromboembolism prophylaxis after hip and knee arthroplasty. J Arthroplast. 2015;30(7):1277–80. https://doi.org/10.1016/j.arth.2015.02.009.
Lazo-Langner A, Fleet JL, McArthur E, Garg AX. Rivaroxaban vs. low molecular weight heparin for the prevention of venous thromboembolism after hip or knee arthroplasty: a cohort study. J Thromb Haemost. 2014;12(10):1626–35. https://doi.org/10.1111/jth.12675.
Sindali K, Rose B, Soueid H, Jeer P, Saran D, Shrivastava R. Elective hip and knee arthroplasty and the effect of rivaroxaban and enoxaparin thromboprophylaxis on wound healing. Eur J Orthop Surg Traumatol. 2013;23(4):481–6. https://doi.org/10.1007/s00590-012-0987-y.
NICE. Venous thromboembolism in over 16 s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism [NG89]. 2018. https://www.nice.org.uk/guidance/ng89/chapter/Recommendations#interventions-for-people-having-orthopaedic-surgery. Accessed 21 Apr 2018.
Australian Commission on Safety and Quality in Health Care. Venous thromboembolism prevention clinical care standard. 2020. https://www.safetyandquality.gov.au/sites/default/files/2020-01/venous_thromboembolism_prevention_clinical_care_standard_-_jan_2020_2.pdf. Accessed 18 Feb 2020.
Cappagh National Orthopaedic Hospital. Annual Report 2016. Ireland East Hospital Group. 2016. http://www.cappagh.ie/sites/default/files/pdf/Annual%20Report%202016.pdf. Accessed 29 July 2017.
Wilson DG, Poole WE, Chauhan SK, Rogers BA. Systematic review of aspirin for thromboprophylaxis in modern elective total hip and knee arthroplasty. Bone Jt J. 2016;98-B(8):1056–61. https://doi.org/10.1302/0301-620x.98b8.36957.
Lakens D, Scheel AM, Isager PM. Equivalence testing for psychological research: a tutorial. Adv Methods Pract Psychol Sci. 2018;1(2):259–69. https://doi.org/10.1177/2515245918770963.
Richardson DB, Kinlaw AC, MacLehose RF, Cole SR. Standardized binomial models for risk or prevalence ratios and differences. Int J Epidemiol. 2015;44(5):1660–72. https://doi.org/10.1093/ije/dyv137.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2017. https://www.R-project.org/. Accessed 10 July 2018.
Khatod M, Inacio MC, Bini SA, Paxton EW. Pulmonary embolism prophylaxis in more than 30,000 total knee arthroplasty patients: Is there a best choice? J Arthroplast. 2012;27(2):167–72. https://doi.org/10.1016/j.arth.2011.04.006.
Westrich GH, Bottner F, Windsor RE, Laskin RS, Haas SB, Sculco TP. VenaFlow plus lovenox vs venaflow plus aspirin for thromboembolic disease prophylaxis in total knee arthroplasty. J Arthroplast. 2006;21(6 SUPPL.):139–43. https://doi.org/10.1016/j.arth.2006.05.017.
Zou Y, Tian S, Wang Y, Sun K. Administering aspirin, rivaroxaban and low-molecular-weight heparin to prevent deep venous thrombosis after total knee arthroplasty. Blood Coag Fibrinol. 2014;25(7):660–4. https://doi.org/10.1097/MBC.0000000000000121.
Brown GA. Venous thromboembolism prophylaxis after major orthopaedic surgery: a pooled analysis of randomized controlled trials. J Arthroplast. 2009;24(6):77–83.
An VVG, Phan K, Levy YD, Bruce WJM. Aspirin as thromboprophylaxis in hip and knee arthroplasty: a systematic review and meta-analysis. J Arthroplast. 2016;31(11):2608–16. https://doi.org/10.1016/j.arth.2016.04.004.
Gómez-Outes A, Terleira-Fernández AI, Suárez-Gea ML, Vargas-Castrillón E. Dabigatran, rivaroxaban, or apixaban versus enoxaparin for thromboprophylaxis after total hip or knee replacement: systematic review, meta-analysis, and indirect treatment comparisons. BMJ. 2012. https://doi.org/10.1136/bmj.e3675.
Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DA Jr, Caprini JA. A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg. 2010;251(2):344–50.
NICE. Venous thromboembolism: reducing the risk for patients in hospital CG92. 2010 (Updated 2015). https://www.nice.org.uk/guidance/cg92/evidence/full-guideline-pdf-243920125. Accessed May 2017.
Anderson FA, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):9–16.
Heit JA. Epidemiology of venous thromboembolism. Nat Revi Cardiol. 2015;12(8):464–74. https://doi.org/10.1038/nrcardio.2015.83.
Imberti D, Bianchi C, Zambon A, Parodi A, Merlino L, Gallerani M, et al. Venous thromboembolism after major orthopaedic surgery: a population-based cohort study. Intern Emerg Med. 2012;7(3):243–9. https://doi.org/10.1007/s11739-011-0567-x.
Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358(26):2765–75. https://doi.org/10.1056/NEJMoa0800374.
Heckmann M, Thermann H, Heckmann F. Rivaroxaban versus high dose nadroparin for thromboprophylaxis after hip or knee arthroplasty. Hämostaseologie. 2015;35(4):358–63. https://doi.org/10.5482/HAMO-14-12-0078.
Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet. 2008;372(9632):31–9. https://doi.org/10.1016/s0140-6736(08)60880-6.
Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008;358(26):2776–86. https://doi.org/10.1056/NEJMoa076016.
Turpie AG, Lassen MR, Davidson BL, Bauer KA, Gent M, Kwong LM, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet. 2009;373(9676):1673–80. https://doi.org/10.1016/s0140-6736(09)60734-0.
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2008;133(6):381S–453S.
Jameson SS, Rymaszewska M, James P, Serrano-Pedraza I, Muller SD, Hui AC, et al. Wound complications following rivaroxaban administration: a multicenter comparison with low-molecular-weight heparins for thromboprophylaxis in lower limb arthroplasty. J Bone Jt Surg. 2012;94(17):1554–8.
Jensen C, Steval A, Partington P, Reed M, Muller S. Return to theatre following total hip and knee replacement, before and after the introduction of rivaroxaban. Bone Jt J. 2011;93(1):91–5.
Acknowledgements
The authors would like to thank all the staff in Cappagh National Orthopaedic Hospital who contributed to the study, particularly the Department of Anaesthetics the Department of Orthopaedic Surgery, and the staff in the Pharmacy Department, Pre-Assessment Clinic and Joint Register.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ní Cheallaigh, S., Fleming, A., Dahly, D. et al. Aspirin compared to enoxaparin or rivaroxaban for thromboprophylaxis following hip and knee replacement. Int J Clin Pharm 42, 853–860 (2020). https://doi.org/10.1007/s11096-020-01032-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01032-1