Abstract
Background Several adverse reactions to tigecycline, which is widely used in patients with severe infections, have been documented. Coagulopathy is a lesser known side effect of tigecycline. Aim of the review We summarize the characteristics, possible mechanisms, and treatment of tigecycline-induced coagulopathy. Method PubMed, Ovid, Embase, ISI Web of Knowledge, CNKI, and Wanfang were searched up to March 5, 2019. All articles concerning coagulopathy induced by tigecycline were included. The article types and languages were not limited. The retrieved articles were screened by two experienced clinicians by reading the titles, abstracts, and full texts. Results Ultimately, 17 articles were targeted, including 13 case reports and 4 retrospective observational studies. Tigecycline-induced coagulopathy usually manifests as the dose-dependent prolongation of prothrombin time and activated partial thromboplastin time and a reduction in the fibrinogen level. Tigecycline and its metabolites may have multiple effects on coagulation, influencing the extrinsic or intrinsic pathway and even the common pathway. There is no specific treatment for tigecycline-induced coagulopathy, but it can be reversed by withdrawing tigecycline. Conclusion Tigecycline acts on the coagulation system in a dose-dependent manner, and the most severe adverse event is bleeding. Overdose and prolonged use should be avoided, suspected coagulopathy must be recognized in time, and tigecycline should be withdrawn to prevent severe adverse events. Also, drug clearance disorders can develop in patients with liver and/or renal dysfunction. For patients with severe hepatic or renal impairment, the maintenance dose should be reduced, and indicators of coagulation function should be closely monitored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact on practice
-
Tigecycline-induced coagulopathy usually manifests as the dose-dependent prolongation of prothrombin time (PT) and activated partial thromboplastin time (APTT) and a reduction in the fibrinogen level.
-
Tigecycline-induced coagulopathy may be due to inhibition of the synthesis of coagulation factors, or direct effects on the coagulation cascade, or both.
-
For patients with hepatic or renal dysfunction, the clearance of tigecycline may be delayed, resulting in tigecycline-induced coagulopathy.
Introduction
Tigecycline is a first-generation glycylcycline antibiotic with broad-spectrum activity, particularly against multidrug-resistant (MDR) bacteria (e.g., methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus). Tigecycline also has good antibacterial activity against Acinetobacter baumannii in vitro and in vivo [1,2,3]. Most patients in the intensive care unit (ICU) have complicated conditions, multiple basic diseases, immunosuppression, and tend to undergo invasive procedures more frequently and require broad-spectrum antimicrobial agents. Together, these factors make ICU patients prone to nosocomial MDR infections. Tigecycline is well tolerated, has minimal drug interactions, and does not require dose adjustment in patients with renal impairment, making it suitable for patients with severe clinical infections. However, adverse reactions to tigecycline are well-established; nausea and vomiting [4,5,6,7] are the most common. Reports of tigecycline-induced coagulopathy have been increasing gradually.
Tigecycline-induced coagulopathy refers to a condition in which the blood’s ability to coagulate is impaired; it occurs after tigecycline has been used for hours or days. In the absence of other factors, this condition may manifest as the prolongation of coagulation parameters or decreases in the fibrinogen level and platelet count. Bleeding may also occur but is rare. To date, few studies have investigated the role of tigecycline in coagulation abnormalities.
Aim
To summarize the characteristics, causes, possible mechanisms, and treatment of tigecycline-induced coagulopathy.
Methods
Search strategy
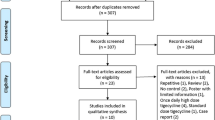
The study was conducted according to Preferred Reporting Items for Systematic Reviews guidelines. We searched the literature using the PubMed, Ovid, Embase, and ISI Web of Knowledge databases up to March 5, 2019. We also searched the CNKI and Wanfang Chinese-language databases. Two investigators performed the literature search using the following search terms: tigecycline, coagulation, coagulopathy, and fibrinogenopenia.
Study selection and data extraction
We found few studies on tigecycline-induced coagulopathy, and most were case reports and retrospective studies. Therefore, the inclusion criteria were studies related to tigecycline-induced coagulopathy published in English and Chinese. The exclusion criteria were languages other than English or Chinese, irrelevant and unpublished articles, and articles that did not state the dosage, duration, and coagulation parameters. The retrieved articles were de-duplicated, selected, and classified by two researchers independently by reading the titles and abstracts. Next, the full text of the articles was reviewed. A database was established, and information was collected on the patients’ characteristics (e.g., age, sex, and nationality), use of drugs, adverse reactions, coagulopathy, and prognosis.
Results
Patients’ characteristics
In total, 770 relevant articles were retrieved; we identified 17 articles on tigecycline-induced coagulopathy, including 13 case reports and 4 retrospective studies. The age of the patients ranged from 42 to 90 (61 ± 17) years, with eight being male and five female. The study period was 2010–2019. We analyzed a total of 184 patients, mainly from China, Greece, and Italy in the included articles. See Table 1 for details.
All patients in the case reports had a variety of basic diseases, and some had two or more. None of the patients had a history of hereditary hemorrhagic disease. One patient had autoimmune cirrhosis [9], one had acute liver injury [21], and the other patients did not have hepatic dysfunction. Finally, most of the patients had kidney disease. See Table 2 for details.
In these articles, tigecycline was mainly used to treat MDR A. baumannii, methicillin-resistant Staphylococcus warneri, Proteus mirabilis, and Klebsiella pneumoniae. Only five cases [9, 10, 15, 18, 23] involved tigecycline monotherapy; most of the patients were taking combinations of antibiotics and/or antivirals, including cefoperazone, sulbactam, imipenem-cilastatin sodium hydrate, caspofungin, vancomycin, piperacillin sulbactam, voliconazole, and linezolid.
Hemorrhage (5 of 13 cases) was the most severe adverse event, and included ecchymosis [15, 20, 22], rectal bleeding [9], and bloody stool [11]. One patient accepted a reduced dosage, and another took more than the recommended dose. See Table 2 for details.
Discussion
Few studies have investigated tigecycline-induced coagulopathy. Tigecycline-induced coagulopathy manifests mainly as the progressive deterioration of blood hypocoagulability and is characterized by a slowly progressive deterioration of coagulation parameters. The abnormal coagulation parameters typically include prolongation of the prothrombin time and activated partial thromboplastin time, an elevated international normalized ratio, and a decreased fibrinogen level, with or without thrombocytopenia. The most severe adverse event caused by tigecycline is hemorrhage (e.g., bloody stool and subcutaneous ecchymosis).
Tigecycline is mainly metabolized in the liver, and is, together with its metabolites, secreted in bile. The liver plays an important role in coagulation by synthesizing clotting factors [25, 26]. Acute or chronic liver disease may cause disorders in coagulation. The plasma clearance of tigecycline was reduced by 25% and 55% by moderate and severe hepatic impairment, respectively. Therefore, the recommended maintenance dose [27] for severe hepatic impairment is 25 mg, while no adjustment of the dosage is required for patients with mild or moderate hepatic impairment. In the case reports, two patients had liver insufficiency before using tigecycline and one patient had altered levels of liver enzymes after using tigecycline. One patient [9] had autoimmune cirrhosis and liver function of Child–Pugh class C but no changes in liver enzyme levels during tigecycline therapy, and experienced multiple rectal bleeding events. One patient [22] with mild hepatic impairment had no changes in the levels of liver enzymes, and developed patchy ecchymosis and bleeding while taking tigecycline. One patient [10] had no liver disease but increased transaminase and total bilirubin levels after taking tigecycline. The liver function of the remaining 10 patients was not impaired during tigecycline treatment, but 3 suffered bleeding events [11, 15, 20], all of whom took the recommended dose. Regarding the retrospective studies, Routsi et al. [12] reported that the bilirubin level did not change significantly, while Zhang et al. [13] and Leng et al. [24] showed that there was no change in alanine aminotransferase (ALT), aspartate aminotransferase, and creatinine (Cr) levels during therapy. However, Sun et al. [16] found that 33 of 59 patients had an elevated ALT or total bilirubin level.
Based on the above, we inferred that tigecycline-induced coagulopathy may be a result of affecting the synthesis of clotting factors. Tigecycline may influence the levels of liver enzymes and/or bilirubin, as well as the synthesis of coagulation factors, but the levels of coagulation factors cannot be assessed by routine testing. Also, the FDA reports that tigecycline may inhibit the synthesis of vitamin K by destroying the intestinal microflora, resulting in vitamin K-dependent coagulopathy, or may directly affect the coagulation cascade. However, vitamin K supplementation is reported not to improve coagulopathy, and the coagulation parameters recover after the infusion of blood products. These results suggest that tigecycline-induced coagulopathy is not caused by alteration of the gastrointestinal flora or vitamin K synthesis. Hence, additional studies are needed.
Almost all patients in the case reports had acute or chronic kidney disease, but no deterioration of renal function after tigecycline administration. In the small study by Zhang et al. [13] there was no change in the Cr level after using tigecycline. Also, the dosage did not need to be adjusted in patients with impaired renal function or undergoing hemodialysis [27, 28]. Also, the clearance of tigecycline in patients with severe renal impairment was reduced by 20%, and the concentration–time curve increased by about 30%. Thus, tigecycline may have no influence on renal function but a reduction in its clearance prolongs the duration of drug activity, increasing the risk of tigecycline-induced coagulopathy.
Coagulopathy occurred after using tigecycline alone or in combination with another agent. Also, the relationship of tigecycline with coagulopathy is time- and dose-dependent: the higher the dose or the longer the course, the more severe the coagulopathy [8,9,10,11, 18,19,20, 23]. Coagulopathy can occur 1–39 days after tigecycline administration. Finally, a duration of tigecycline therapy of > 14 days was a risk factor for tigecycline-induced coagulopathy [16].
Vitamin K supplementation [8, 9, 15, 18, 22] does not reverse coagulopathy, while the abnormal indicators typically recover within 10 days of tigecycline discontinuation. Also, the infusion of plasma, blood factors, fibrinogen, and cryoprecipitate can temporarily correct or improve coagulation abnormalities. So, when the fibrinogen level decreases to < 1.2 g/L, an infusion of clotting factors should be considered [13]. Once a bleeding event occurs, the best response is to stop using tigecycline and to infuse blood products.
This study has several limitations. First, it was based on a literature review that yielded few articles and may have been subject to publication bias. Second, the data may be incomplete, and so unsuitable for in-depth analysis. Third, due to the lack of basic research and large-scale studies, the mechanisms of tigecycline-induced coagulopathy are unclear.
Conclusion
In conclusion, tigecycline can cause coagulopathy, but the mechanisms are unclear; possible causes include altering the synthesis of clotting factors. In addition, tigecycline may not significantly damage the liver and kidneys. However, in patients with abnormal liver and kidney function, drug clearance may be prolonged and the area under the blood concentration–time curve is increased, leading to an increased drug concentration. Therefore, we recommend that the dosage should be adjusted patients with liver and kidney dysfunction. During tigecycline treatment, blood coagulation function, routine blood parameters, and stool occult blood should be monitored. If there is no bleeding but the course of tigecycline is > 2 weeks and the fibrinogen level is < 1.2 g/L, it is recommended to infuse clotting factors and continue to monitor the coagulation function. If blood stasis and bloody stools occur, tigecycline should be stopped immediately.
References
Boucher HW, Wennersten CB, Eliopoulos GM. In vitro activities of the glycylcycline GAR-936 against gram-positive bacteria. Antimicrob Agents Chemother. 2000;44(8):2225–9.
Edlund C, Nord CE. In-vitro susceptibility of anaerobic bacteria to GAR-936, a new glycylcycline. Clin Microbiol Infect. 2000;6(3):159–63.
Liu Y, Pu Z, Zhao M. Successful treatment of extensively drug-resistant Acinetobacter baumannii ventriculitis with intravenous plus intraventricular tigecycline—a case report. Antimicrob Agents Chemother. 2018;62:e01625-18.
Gilson M, Moachon L, Jeanne L, Dumaine V, Eyrolle L, Morand P, et al. Acute pancreatitis related to tigecycline: case report and review of the literature. Scand J Infect Dis. 2008;40(8):681–3.
Bonilla MF, Avery RK, Rehm SJ, Neuner EA, Isada CM, van Duin D, et al. Extreme alkaline phosphatase elevation associated with tigecycline. J Antimicrob Chemother. 2011;66(4):952–3.
Prot-Labarthe S, Youdaren R, Benkerrou M, Basmaci R, Lorrot M. Pediatric acute pancreatitis related to tigecycline. Pediatr Infect Dis J. 2010;29(9):890–1.
Hung WY, Kogelman L, Volpe G, Iafrati M, Davidson L. Tigecycline-induced acute pancreatitis: case report and literature review. Int J Antimicrob Agents. 2009;34(5):486–9.
Pieringer H, Schmekal B, Biesenbach G, Pohanka E. Severe coagulation disorder with hypofibrinogenemia associated with the use of tigecycline. Ann Hematol. 2010;89(10):1063–4.
Rossitto G, Piano S, Rosi S, Simioni P, Angeli P. Life-threatening coagulopathy and hypofibrinogenaemia induced by tigecycline in a patient with advanced liver cirrhosis. Eur J Gastroenterol Hepatol. 2014;26:681–4.
Sabanis N, Paschou E, Gavriilaki E, Kalaitzoglou A, Vasileiou S. Hypofibrinogenemia induced by tigecycline: a potentially life-threatening coagulation disorder. Infect Dis (Lond Engl). 2015;47(10):743–6.
Zhang Q, Zhou J. Fibrinogenopenia caused by tigecycline: a case report. Eur Rev Med Pharmacol Sci. 2015;19(6):915–7.
Routsi C, Kokkoris S, Douka E, et al. High-dose tigecycline-associated alterations in coagulation parameters in critically ill patients with severe infections. Int J Antimicrob Agents. 2015;45(1):90–3.
Zhang Q, Zhou S, Zhou J. Tigecycline treatment causes a decrease in fibrinogen levels. Antimicrob Agents Chemother. 2015;59(3):1650–5.
Bourneau-Martin D, Crochette N, Drablier G, Lagarce L, Lainé-Cessac P. Hypofibrinogenemia complicated by hemorrhagic shock following prolonged administration of high doses of tigecycline. In: 20th Annual Meeting of French Society of Pharmacology and Therapeutics, 37th Pharmacovigilance Meeting, 17th APNET Seminar, 14th CHU CIC Meeting. Fundamental and Clinical Pharmacology 2016;30(Suppl 1):29.
Zhong B, Peng F, Yang R. Yisitijiahuansuzhipizhenjiyanzhongningxuegongnengzhangaiyili (Chinese). Chin J Hosp Pharm. 2016;36(18):1620.https://doi.org/10.13286/j.cnki.chinhosppharmacyj.2016.18.22.
Sun L, Zhang B, Wu B, Zhang Q. Effects and related factors analysis of tigecycline on the level of plasma fibrinogen in the hospitalized patients. Adverse Drug Reactions J. 2017;19(1):31–6.
McMahan J, Moenster RP. Tigecycline-induced coagulopathy. Am J Health Syst Pharm. 2017;74(3):130–4.
Giryes S, Azzam ZS, Ismael-Badarneh R, Krivoy N, Berger G. Severe coagulation disorder and thrombocytopenia associated with tigecycline—case report and review of literature. Curr Drug Saf. 2017;12(1):7–9.
Wu X, Zhao P, Dong L, Zhang X. A case report of patient with severe acute cholangitis with tigecycline treatment causing coagulopathy and hypofibrinogenemia. Medicine. 2017;96(49):e9124.
Wu P, Wu C. Tigecycline-associated hypofibrinogenemia: a case report and review of the literature. IDCases. 2018;11:56–7.
Pan H, Dong L, Zhang X. Tijiahuansuzhiyiliningxuegongnzhangai (chinese). Pharm Clin Res. 2018;(03):233–4.
Dai W, Su D. Tijiahuansuzhiningxuegongnengyichangyilideyaoxuejianhu (chinese). Chin J Clin Rational Drug Use. 2018;(01):132–3. https://doi.org/10.15887/j.cnki.13-1389/r.2018.01.074.
Yilmaz DF, Yildirim H, Sen EM. A lesser known side effect of tigecycline: hypofibrinogenemia. Turk J Haematol. 2018;35(1):83–4.
Leng B, Xue YC, Zhang W, et al. A retrospective analysis of the effect of tigecycline on coagulation function. Chem Pharm Bull. 2019;67(3):258–64.
Amitrano L, Guardascione MA, Brancaccio V, Balzano A. Coagulation disorders in liver disease. Semin Liver Dis. 2002;22(1):83–96.
Heinz S, Braspenning J. Measurement of blood coagulation factor synthesis in cultures of human hepatocytes. Methods Mol Biol. 2015;1250:309–16.
Wyeth Pharmaceuticals Inc. ASOP. TYGACIL- tigecycline injection, powder, lyophilized, for solution. 2005; 17 Mar 2019.
Korth-Bradley JM, Troy SM, Matschke K, et al. Tigecycline pharmacokinetics in subjects with various degrees of renal function. J Clin Pharmacol. 2012;52(9):1379–87.
Acknowledgements
The authors thank Drs. Zhong Cheng and Tang QiaoLuan for their advice.
Funding
No specific funding was received.
Conflicts of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Cui, N., Cai, H., Li, Z. et al. Tigecycline-induced coagulopathy: a literature review. Int J Clin Pharm 41, 1408–1413 (2019). https://doi.org/10.1007/s11096-019-00912-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-019-00912-5