Abstract
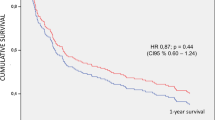
Background Potentially inappropriate medications (PIMs) are common in older patients with polypharmacy, and are related to negative clinical results. Little information is available on the characteristics and consequences of PIMs in patients with advanced chronic conditions and palliative care needs. Objective To evaluate, for this population: (i) the prevalence of PIMs; (ii) the possible risk factors associated with its onset; and (iii) the related clinical consequences. Setting Acute-hospital care Geriatric Unit (AGU) in County of Osona, Spain. Method Ten-month prospective cross-sectional study. Patients with palliative care needs were identified according to the NECPAL CCOMS-ICO® test. Upon hospital admission, a multidisciplinary team consisting of a pharmacist and two AGU physicians determined the PIMs of the routine chronic medication of the patients. Sociodemographic and pharmacological data were collected with the objective of determining possible risk factors related to the existence of PIMs. Main outcome measure Prevalence and type of PIMs according to STOPP version 2 and MAI criteria at the time of hospital admission. Furthermore, days of hospital admission, destination at hospital discharge and survival analysis at 12 months related to PIMs were evaluated. Results Two hundred thirty-five patients (mean age 86.80, SD 5.37; 65.50% women) were recruited. According to the STOPP criteria, 88.50% of patients had ≥1 criterion (mainly ‘indication of medication’, followed by those that affect the nervous system and psychotropic drugs and risk drugs in people suffering from falls), and according to the MAI tool, 97.40% of the patients had some criterion related to inappropriate medication (mainly, duration of therapy). The following conditions were identified as risk factors for the existence of PIMs: insomnia, anxiety–depressive disorder, falls, pain, excessive polypharmacy and therapeutic complexity. There were no differences among patients in days of hospital stay, discharge’s destination or survival at 12 months, regardless of the tool used. Conclusion The presence of PIMs is high in patients requiring palliative care. Some potentially modifiable risk factors such as the pharmacological ones are associated with a greater presence of inappropriate medication. The presence of PIMs does not affect this population in terms of mortality.

Similar content being viewed by others
References
Connor MNO, Gallagher P, Mahony DO. Inappropriate prescribins: criteria, detection and prevention. Drugs Aging. 2012;29:437–52.
Beers E, Moerkerken DC, Leufkens HGM, Jansen PAF. Participation of older people in preauthorization trials of recently approved medicines. J Am Geriatr Soc. 2014;62:1883–90.
Corsonello A, Pedone C, Incalzi RA. Age-related pharmacokinetic and pharmacodynamic changes and related risk of adverse drug reactions. Curr Med Chem. 2010;17:571–84.
American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;2015(63):2227–46.
O’Mahony D, O’Sullivan DP, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–8.
Wallace E, McDowell R, Bennett K, Fahey T, Smith SM. Impact of potentially inappropriate prescribing on adverse drug events, health related quality of life and emergency hospital attendance in older people attending general practice: a prospective cohort study. J Gerontol Ser A Biol Sci Med Sci. 2017;72:271–7.
Hudhra K, Beçi E, Petrela E, Xhafaj D, García-Caballos M, Bueno-Cavanillas A. Prevalence and factors associated with potentially inappropriate prescriptions among older patients at hospital discharge. J Eval Clin Pract. 2016;22:707–13.
Kaufmann CP, Tremp R, Hersberger KE, Lampert ML. Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol. 2014;70:1–11.
Hanlon JT, Schmader KE, Samsa GP. A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992;45:1045–51.
Hedna K, Hakkarainen KM, Gyllensten H, Jönsson AK, Petzold M, Hägg S. Potentially inappropriate prescribing and adverse drug reactions in the elderly: a population-based study. Eur J Clin Pharmacol. 2015;71:1525–33.
Brown JD, Hutchison LC, Li C, Painter JT, Martin BC. Predictive validity of the beers and screening tool of older persons’ potentially inappropriate prescriptions (STOPP) criteria to detect adverse drug events, hospitalizations, and emergency department visits in the United States. J Am Geriatr Soc. 2016;64:22–30.
Ryan C, O’Mahony D, Kennedy J, Weedle P, Byrne S. Potentially inappropriate prescribing in an Irish elderly population in primary care. Br J Clin Pharmacol. 2009;68:936–47.
Cahir C, Bennett K, Teljeur C, Fahey T. Potentially inappropriate prescribing and adverse health outcomes in community dwelling older patients. Br J Clin Pharmacol. 2013;77:201–10.
Grace AR, Briggs R, Kieran RE, Corcoran RM, Romero-Ortuno R, Coughlan TL, et al. A comparison of beers and STOPP criteria in assessing potentially inappropriate medications in nursing home residents attending the emergency department. J Am Med Dir Assoc. 2014;15:830–4.
Chen LL, Tangiisuran B, Shafie AA, Hassali MAA. Evaluation of potentially inappropriate medications among older residents of Malaysian nursing homes. Int J Clin Pharm. 2012;34:596–603.
Sevilla-Sánchez D, Espaulella-Panicot J, de Andrés-Lazaro AM, Torres-Allezpuz R, Soldevila-Llagostera M, Codina-Jane C. Potentially inappropriate medication on admission to a medium-stay unit according to STOPP and START criteria. Rev Esp Geriatr Gerontol. 2012;47:155–7.
Corsonello A, Pedone C, Lattanzio F, Lucchetti M, Garasto S, Di Muzio M, et al. Potentially inappropriate medications and functional decline in elderly hospitalized patients. J Am Geriatr Soc. 2009;57:1007–14.
Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Frequency of inappropriate medication prescription in hospitalized elderly patients in Italy. PLoS ONE. 2013;8:e82359.
Cahir C, Fahey T, Teeling M, Teljeur C, Feely J, Bennett K. Potentially inappropriate prescribing and cost outcomes for older people: a national population study. Br J Clin Pharmacol. 2010;69:543–52.
Barry PJ, Gallagher P, Ryan C, O’mahony D. START (screening tool to alert doctors to the right treatment)—an evidence-based screening tool to detect prescribing omissions in elderly patients. Age Ageing. 2007;36:632–8.
Gallagher P, Lang PO, Cherubini A, Topinková E, Cruz-Jentoft A, Errasquín BM, et al. Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol. 2011;67:1175–88.
Di Giorgio C, Provenzani A, Polidori P. Potentially inappropriate drug prescribing in elderly hospitalized patients: an analysis and comparison of explicit criteria. Int J Clin Pharm. 2016;38:462–8.
Vidal X, Agustí A, Vallano A, Formiga F, Moyano AF, García J, et al. Elderly patients treated with psychotropic medicines admitted to hospital: associated characteristics and inappropriate use. Eur J Clin Pharmacol. 2016;72:755–64.
Ailabouni NJ, Nishtala PS, Tordoff JM. Examining potentially inappropriate prescribing in residential care using the STOPP/START criteria. Eur Geriatr Med. 2016;7:40–6.
Tommelein E, Mehuys E, Petrovic M, Somers A, Colin P, Boussery K. Potentially inappropriate prescribing in community-dwelling older people across Europe: a systematic literature review. Eur J Clin Pharmacol. 2015;71:1415–27.
Lang P-O, Hasso Y, Dramé M, Vogt-Ferrier N, Prudent M, Gold G, et al. Potentially inappropriate prescribing including under-use amongst older patients with cognitive or psychiatric co-morbidities. Age Ageing. 2010;39:373–81.
Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. Lancet. 2015;385:540–8.
Schenker Y, Arnold R. The next era of palliative care. JAMA. 2015;314:1565–6.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Gómez-Batiste X, Martínez-Muñoz M, Blay C, Amblàs J, Vila L, Costa X. Identification of people with chronic advanced diseases and need of palliative care in sociosanitary services: elaboration of the NECPAL CCOMS-ICO© tool. Med Clin (Barc). 2013;140:241–5.
Gómez-Batiste X, Martínez-Muñoz M, Blay C, Amblàs J, Vila L, Costa X, et al. Prevalence and characteristics of patients with advanced chronic conditions in need of palliative care in the general population: a cross-sectional study. Palliat Med. 2014;28:302–11.
Gómez-Batiste X, Martínez-Muñoz M, Blay C, Espinosa J, Contel JC, Ledesma A. Identifying needs and improving palliative care of chronically ill patients: a community-oriented, population-based, public-health approach. Curr Opin Support Palliat Care. 2012;6:371–8.
Sevilla-Sanchez D, Molist-Brunet N, Amblàs-Novellas J, Roura-Poch P, Espaulella-Panicot J, Codina-Jané C. Adverse drug events in patients with advanced chronic conditions who have a prognosis of limited life expectancy at hospital admission. Eur J Clin Pharmacol. 2017;73:79–89.
George J, Phun Y-T, Bailey MJ, Kong DCM, Stewart K. Development and validation of the medication regimen complexity index. Ann Pharmacother. 2004;38:1369–76.
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry. 1982;140:566–72.
Reisberg B. Global measures: utility in defining and measuring treatment response in dementia. Int Psychogeriatr. 2007;19:421–56.
Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud. 1988;10:64–7.
Frankenthal D, Lerman Y, Lerman Y. The impact of hospitalization on potentially inappropriate prescribing in an acute medical geriatric division. Int J Clin Pharmacol Ther. 2015;37:60–7.
Cahir C, Moriarty F, Teljeur C, Fahey T, Bennett K. Potentially inappropriate prescribing and vulnerability and hospitalization in older community-dwelling patients. Ann Pharmacother. 2014;48:1546–54.
Heppenstall CP, Broad JB, Boyd M, Hikaka J, Zhang X, Kennedy J, et al. Medication use and potentially inappropriate medications in those with limited prognosis living in residential aged care. Australas J Ageing. 2016;35:E18–24.
Suhrie EM, Hanlon JT, Jaffe EJ, Sevick MA, Ruby CM, Aspinall SL. Impact of a geriatric nursing home palliative care service on unnecessary medication prescribing. Am J Geriatr Pharmacother. 2009;7:20–5.
Hajjar ER, Hanlon JT, Sloane RJ, Lindblad CI, Pieper CF, Ruby CM, et al. Unnecessary drug use in frail older people at hospital discharge. J Am Geriatr Soc. 2005;53:1518–23.
O’Mahony D, O’Connor MN. Pharmacotherapy at the end-of-life. Age Ageing. 2011;40:419–22.
Steinman MA, Beizer JL, DuBeau CE, Laird RD, Lundebjerg NE, Mulhausen P. How to use the American Geriatrics Society 2015 Beers Criteria—a guide for patients, clinicians, health systems, and payors. J Am Geriatr Soc. 2015;63:e1–7.
Molist Brunet N, Sevilla-Sánchez D, Novellas JA, Jané CC, Gómez-Batiste X, McIntosh J, et al. Optimizing drug therapy in patients with advanced dementia: a patient-centered approach. Eur Geriatr Med. 2014;5:66–71.
Molist Brunet N, Espaulella Panicot J, Sevilla-Sánchez D, Novellas JA, Jané CC, Altimiras Roset J, et al. A patient-centered prescription model assessing the appropriateness of chronic drug therapy in older patients at the end of life. Eur Geriatr Med. 2015;6:565–9.
Gomez-Batiste X, Martinez-Munoz M, Blay C, Amblas J, Vila L, Costa X, et al. Identifying patients with chronic conditions in need of palliative care in the general population: development of the NECPAL tool and preliminary prevalence rates in Catalonia. BMJ Support Palliat Care. 2012;3:300–8.
Moroni M, Zocchi D, Bolognesi D, Abernethy A, Rondelli R, Savorani G, et al. The “surprise” question in advanced cancer patients: a prospective study among general practitioners. Palliat Med. 2014;28:959–64.
Lakin JR, Robinson MG, Bernacki RE, Powers BW, Block SD, Cunningham R, et al. Estimating 1-year mortality for high-risk primary care patients using the “surprise” question. JAMA Intern Med. 2016;176:1863–5.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (screening tool of older person’s prescriptions) and START (screening tool to alert doctors to right treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46:72–83.
Acknowledgements
We thank all the nurses, patients and caregivers who have participated and collaborated in the study.
Funding
This study was partially supported by a Ph.D. Research Fellowship granted by “Consultori Bayes”. The funders had no role in the design, execution, analysis, interpretation or writing of the study.
Conflicts of interest
The authors declare that they have no conflict of interest with respect to the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sevilla-Sánchez, D., Molist-Brunet, N., Amblàs-Novellas, J. et al. Potentially inappropriate medication at hospital admission in patients with palliative care needs. Int J Clin Pharm 39, 1018–1030 (2017). https://doi.org/10.1007/s11096-017-0518-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0518-3