Abstract
Background People diagnosed with serious mental illnesses (SMIs) such as schizophrenia and bipolar affective disorder are frequently treated with antipsychotics. National guidance advises the use of shared decision-making (SDM) in antipsychotic prescribing. There is currently little data on the opinions of health professionals on the role of SDM. Objective To explore the views and experiences of UK mental health pharmacists regarding the use of SDM in antipsychotic prescribing in people diagnosed with SMI. Setting The study was conducted by interviewing secondary care mental health pharmacists in the UK to obtain qualitative data. Methods Semi-structured interviews were recorded. An inductive thematic analysis was conducted using the method of constant comparison. Main outcome measure Themes evolving from mental health pharmacists on SDM in relation to antipsychotic prescribing in people with SMI. Results Thirteen mental health pharmacists were interviewed. SDM was perceived to be linked to positive clinical outcomes including adherence, service user satisfaction and improved therapeutic relations. Despite more prescribers and service users supporting SDM, it was not seen as being practised as widely as it could be; this was attributed to a number of barriers, most predominantly issues surrounding service user’s lacking capacity to engage in SDM and time pressures on clinical staff. The need for greater effort to work around the issues, engage service users and adopt a more inter-professional approach was conveyed. Conclusion The mental health pharmacists support SDM for antipsychotic prescribing, believing that it improves outcomes. However, barriers are seen to limit implementation. More research is needed into overcoming the barriers and measuring the benefits of SDM, along with exploring a more inter-professional approach to SDM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts of findings
-
Pharmacists can play a key role in developing a shared decision making model for antipsychotic prescribing.
-
Greater efforts to engage service users and multidisciplinary team working are required to enable SDM to be implemented.
-
Further research is required on the views of service users on SDM and the role of pharmacy in supporting SDM.
Introduction
At least one in four people in the UK will experience a mental health problem and up to two percent of the population will be diagnosed with a serious mental illness (SMI) during their lifetime [1]. For the purposes of this research SMI is considered to include diagnoses that are treated with antipsychotics, typically schizophrenia and bipolar affective disorder [2]. The adverse effects of antipsychotics can decrease adherence rates [3].
Adherence, the currently accepted term used for medication-taking behaviour, is defined ‘as the extent to which the patient’s action matches the agreed recommendations’ [4]. Adherence presumes agreement about the proposed medication, between the prescriber and the person taking the medicine, emphasising the importance of shared decision-making (SDM; [4]). A third to a half of all medications for long-term conditions are not taken as recommended, and treatment adherence is one of the biggest challenges in mental health [4, 5]. Adherence in SMI is very poor; estimated non-adherence rates for people diagnosed with schizophrenia range from 40 to 75 % [6, 7]. Studies have found that 75 % of people with chronic schizophrenia discontinue their medication within 18 months [8] and non-adherence rates in bipolar disorder range between 20 and 60 % with a mean of 41 % [9, 10]. Antipsychotic prescribing lends itself to SDM, because the adverse event profile is the main factor in the choice of antipsychotics [11].
SDM is defined by the NHS as ‘the conversation that happens between a patient and their healthcare professional to reach a healthcare choice together’, where both parties consider what is important to the other when selecting treatment. There are ethical, clinical and economic arguments for SDM [12]; it represents a method of healthcare communication that promotes patient-centred care and sharing expertise between clinicians and service users [13, 14]. The most accepted model is that of Charles and colleagues, which emphasises patient autonomy, informed consent and empowerment [15]. SDM is founded on partnership and opposed to a paternalistic model of healthcare [16]. A recent Department of Health White Paper stated that ‘care should be personalised to reflect peoples’ needs, not those of the professional or the system’ and patients should be involved in treatment decisions [17]. People diagnosed with SMI can be fully engaged with making decisions and seek a more collaborative approach, thus treatment decisions should be made by the service user and the healthcare professional working together and considering both the likely benefits and possible adverse effects of the medication [11, 18].
SDM has been linked to improved quality of care and service user satisfaction [19, 20]. However, the evidence base supporting the use of SDM for chronic conditions, notably mental health [21] and the use of SDM for decisions made on multiple occasions over the longer-term is limited. Hamann [22] found that SDM increased knowledge and perceived involvement in treatment in inpatients with schizophrenia. However, SDM failed to show long-term benefits in the same study [23]. A Cochrane review found that no conclusions could be drawn regarding the effectiveness of SDM interventions for people with mental health problems and highlighted the urgent need for more research [13]. A more recent study found that although a pharmacist intervention based on SDM significantly improved adherence, treatment satisfaction and beliefs about medication in people with depression, it had no significant effect on depressive symptoms [24].
Both service users and clinicians appear to support SDM [25]. However, only 32 % of service users report that their views about treatment were considered ‘to some extent’ and less than half (43 %) were informed about adverse effects, suggesting clinicians are not engaging in SDM [26]. The lack of a multi-disciplinary approach and the perceived difficulty of implementing SDM with service users who may lack insight are barriers to SDM across mental healthcare [21, 27]. In addition, there are structural obstacles to collaborative care in psychiatry which include timely access to relevant, reliable clinical information, and therefore research is vital to understand the practicalities of SDM in practice [21, 28, 29].
Whilst experiences of and attitudes of consultant psychiatrists towards shared decision making in antipsychotic prescribing have been studied, qualitative data on the views of other key groups of healthcare professionals involved in medication management across mental health services, including pharmacists, is lacking [21]. This study aimed to understand the views and opinions of mental health pharmacists in the UK who are increasingly developing clinical roles. These clinical roles include; advising prescribers and clinicians on the most appropriate medication after interviewing patients; patient education and advocacy; attending and directly inputting into multi-disciplinary meetings. These roles are generally independent from the prescribing process although a limited number of pharmacists may have a caseload with a prescribing role.
Aim
To elucidate the experiences and opinions of mental health pharmacists about implementing SDM in the process of antipsychotic choice and prescribing in SMI.
Ethics approval
The project received approval from the Aston University Ethics Committee.
Methods
Design
An exploratory qualitative study design that followed COREQ (Consolidated Criteria for Reporting Qualitative studies) guidelines [30] was employed.
Participant recruitment and consent
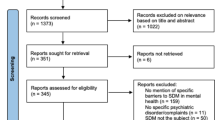
Mental health pharmacists with a minimum of 12 months experience in mental health pharmacy practice were recruited, on the basis that they were more likely to have an understanding of SDM and be undertaking advanced clinical roles. Participants were recruited from the Midlands region of the UK. Initially convenience sampling was used; known contacts meeting the inclusion criteria were identified [31]. Further participants were recruited through active snowballing [32]. Potential participants were emailed with the project aims and participation requirements. Written informed consent was obtained prior to participation.
Inclusion criteria
Mental health pharmacists with a minimum of 12 months experience in mental health pharmacy practice.
Interview structure and collection
A semi-structured interview was used to allow the interviews to be participant-led and participants to express their views openly [33–35]. An initial interview topic guide, based on the literature on research into SDM in mental health, was constructed to focus the interviews [36]. This guide was reviewed and amended by the academic supervisor (IM) and two practising mental health pharmacists (NH, DS; see “Appendix 1” of Supplementary Material). The schedule was adapted following each interview, using an iterative approach [37, 38]. Participants were given a chance to provide feedback and suggest questions to be included in the topic guide. Eleven face-to-face and two phone interviews were conducted; each lasted between 20 and 35 min. These 13 interviews were deemed sufficient to provide the necessary identification of themes. The transcripts were reviewed after each interview and data saturation was perceived to have been met as no new themes were identified in the last set of interviews [39]. Interviews were audio recorded and a verbatim account produced from these recordings [40]. The recordings were checked against the transcripts several times [41].
Data analysis
Thematic analysis, based on the identification of themes, was conducted by MY [34]. The transcripts were independently reviewed by IM; any disagreements on the coding scheme were resolved by discussion between IM and MY.
The constant comparison method informed by grounded theory was used whereby the data analysis takes place alongside data collection [42, 43]. Each interview was reviewed before the next commenced to identify emerging patterns in the data and assist structuring of further interviews [33]. Coding took place in three stages [35, 44], as follows:
-
Open coding was used to identify themes; coding and categories were refined.
-
Axial coding was then used. Extracts were photocopied from the original data and arranged with the codes together in files.
-
Selective coding was used; data was analysed and re-organised. Themes were arranged according to their relation to the research question.
Reflexivity
Qualitative research as a process necessitates and acknowledges the key role of reflexivity, and the important role played by any researcher’s background, perceptions and interests in the topic [30, 33, 36, 37]. Within this study, the interviews were conducted by a female pharmacy undergraduate student of Indian sub-continent descent. In preparation for the study, the student received training in research methods including qualitative research, supervisory guidance during the development of the interview schedule and support from the research team in relation to the interpretation and analytic process.
Results
Fifteen participants were recruited but two interviews didn’t take place due to time constraints. Of the 13 participants interviewed the majority were aged between 30 and 40 years old (six of the 11 participants who reported this information). Ten participants were female and three were male. Four main themes were identified: attitudes to SDM; barriers to implementation; benefits of SDM; and the role of mental health pharmacists.
Attitudes to shared decision making
Pharmacist attitudes
Almost all the pharmacists felt SDM was a positive concept and supported its use in antipsychotic prescribing.
I totally support the idea…they’re powerful drugs therefore….patients should have the opportunity to articulate what factors are most important to them and this should be taken into consideration when choosing treatment. (In01)
The complexity of antipsychotic use was recognised, with reference in particular to side effects and the impact on adherence rates. For these reasons, patient choice was highlighted as being particularly important:
The choice should be dependent on what the patient will tolerate in regards to side effects. (In13)
The pharmacists believed that it was important to involve service users in the discussion, even if agreement could not be reached.
We get that quite a lot. We have involved them in the treatment plan but they might not agree still with the decision that we have tried to involve them with. (In06)
However, some pharmacists viewed SDM as a tool to achieve adherence, to persuade the patient to take the medication, rather than an agreement negotiated between two equal parties.
A few cases it has helped but we still need to persist in getting them to take their medication so it’s still an issue. Once they realise that medication is important they feel better then hopefully…sometimes when we have given them a lot of choice the patient seems to change their mind a lot. (In06)
The views of pharmacists on the attitudes of prescribers
Pharmacists believed that attitudes towards SDM amongst prescribers were variable.
There’s a very broad church amongst (prescribers)…some are excellent and some have the view the patients should do as they’re told. (In04)
The majority, however, felt that there had been a positive cultural shift, with attitudes moving towards greater service user involvement.
Attitudes have definitely changed in my 16 years in mental health, early on it was very much…I’m the doctor and this is what’s right. I think health as a whole has shifted…engaging with the patient a lot more. At one time…it was…if you tell patients about side effects they won’t take the medication. (In03)
However, some pharmacists felt that SDM was not practised as widely as it should be due to the perceived difficulties in relation to patient engagement:
I’m not saying…they don’t want to involve patients but I think it’s because of the difficulty of engaging patients. (In11)
The views of pharmacists on the attitudes of service users
The pharmacists also believed that the attitudes of service users towards SDM were variable; some service users were seen to want involvement in the decision-making process whereas others preferred the clinicians to make the decisions.
Some patients want to be told what to do; other patients want…to make the decision themselves. (In04)
There was, however, a general consensus amongst the pharmacists that service users, particularly younger service users, were increasingly wanting to be involved in the decision-making process and have more choice, partly due to changes in society.
They crave that involvement and…empowerment…in a largely consumerist society people want and expect choice and…more autonomy. (In01)
Barriers to implementation of SDM
Capacity and insight
A lack of service user insight was seen by the participants as an obstacle to SDM.
If they don’t have insight…it doesn’t matter what decision you make or information you give (them)…(if they believe that) there’s nothing wrong with them they don’t need to take treatment. (In04)
Several pharmacists highlighted the fact that when treatment decisions (initiation, dose change or switching) are frequently made, that service users are often acutely unwell and so these are times of difficulty in relation to SDM. Moreover, if they are detained under the mental health act then treatment decisions may be imposed on the service user as being in their best interests rather than attempting to overcome the barriers associated with SDM at these points:
They might be acutely unwell…they might not be in a position to make a decision they might be forced to have treatment against their wishes so in that scenario you’re not going to be able to provide them with SDM. (In03)
When medication regimes were working well, there was often hesitancy from clinicians to make changes.
Switching a treatment when they have been stabilised a long period of time is actually a very scary thing to do. (In13)
However, the majority of pharmacists felt that SDM could be implemented with most of the service users, most of the time:
If you are flexible in your approach…but nevertheless you can still have some degree of conversation to enable them to be a part of the SDM process the vast majority of the time. (In07)
Time
Time was a key barrier to SDM. Pharmacists believed that clinicians often did not have the opportunity to speak to service users or time to fully implement techniques of SDM:
It takes a lot longer than just writing a prescription. (In06)
Such time pressures were increasingly problematic with services experiencing high demand:
There’s always a demand for beds, it does have an impact on SDM. (In05)
Not having the time in outpatient clinics. (In13)
Potential benefits of SDM
Adherence
Pharmacists felt that if service users were genuinely involved in the prescribing decision, this could improve adherence.
If they’re taking part in the decision they have an interest in the outcome…if you don’t involve them and you are imposing something, as soon as they go out of the door they won’t actually be interested in continuing with it. (In05)
Mental health was viewed as similar to any other chronic illness management in that giving more autonomy to service users improved adherence to medication.
I think it’s like any other condition…the more autonomy you give the patient…the more likely they are to comply. (In10)
Importantly, the absence of SDM was believed to result in non-adherence and high rates of re-admission to hospitals.
It’s not as high as it ought to be otherwise…they wouldn’t have so many patients relapsing, we have these revolving door patients that keep coming in again and again, people just don’t take their medication. (In02)
However, there was recognition that those service users who were engaged and interested in SDM could be those who were more likely to be adherent regardless of approach.
Those patients who can actually engage are more likely I think to actually be concordant. (In11)
Service user satisfaction
Service users were said to respond well to SDM, and appreciate being involved in decisions about their care, improving the therapeutic alliance. One pharmacist who believed that SDM had a positive effect on the therapeutic alliance quoted one service user saying:
You were one of the few people who saw me as a human being and gave me a choice, when everyone else was just telling me what to do. (In07)
SDM could help service users feel more valued and respected, and work towards removing some of the stigma that is associated with mental health.
It’s huge stigma all around… so if you treat them like every other human being… they’re going to feel valued and respected definitely …there’s definite improvement, they feel at the centre of their care…they will respect you for giving them that rather than being domineering and telling them…. I know better than you. (In02)
The role of the mental health pharmacist
Service user counselling
The pharmacists felt that service users were often more open about medication issues with them than other health professionals, particularly about sensitive side effects such as sexual dysfunction.
I’ve had a patient discuss sexual dysfunction with myself……where they didn’t discuss it on the ward review because they felt embarrassed to talk about it with the consultant. (In13).
Pharmacists felt they were often seen as an independent person compared to the prescriber and therefore able to have an open conversation with service users about medication.
I do think we’re in a very good position to discuss things because we are….seen as independent. (In10)
More research into the impact pharmacists can have upon clinical outcomes such as relapse rates was suggested.
I think we could reduce (the) relapse rate. Somebody needs to do a study into pharmacist input….and the impact it has on non-concordance. (In13)
Multi-disciplinary team (MDT) working
The level of input that mental health pharmacists have in SDM was dependent on the leadership of the MDT, with some clinical teams more collaborative than others, and resourcing within pharmacy services.
Some of the clinical teams I’m in are very collaborative and very collegiate… I’ve also worked in teams where there’s very little conversation apart from between nurses and doctors, me as the pharmacist has to almost fight to say something. (In07)
Mental health pharmacists clearly felt that they had more to offer and were often underutilised.
I think they have a really difficult job, but if they let us help them, a bit more in recognising we have a resource here, that we can actually use that we have the knowledge. (In11)
Pharmacists believed that a more inter-disciplinary approach with a referral system could support their involvement in SDM.
Some way of referring patients to a pharmacist clinic….but there’s no actual referral process (In13)
Discussion
Pharmacist participants were supportive in principle for SDM, particularly when considering the use of antipsychotic medication, and believed that practising SDM was a key part of stigma-free clinical care. Like previous research, the pharmacists felt SDM increased service user satisfaction, which in turn improved the therapeutic relationship and was key to achieving long term treatment success and positive outcomes by improving adherence to medication [19, 45–50].
The pharmacists perceived that attitudes of both services users and prescribers to SDM varied. Some pharmacists felt that a minority of service users were happy with the clinician making treatment decisions on their behalf. Other research has also identified this group who believe ‘the doctor knows best’; perhaps because they undervalue their expertise in relation to clinicians and want to be ‘a good patient’ [47, 51]. Most service users, however, particularly those in younger age groups, were said by the pharmacists to increasingly crave involvement, which is in line with previous research [27, 46, 52]. This change may reflect an increasingly consumerist society, where choice is expected [53–55].
A strong, trusting relationship, with health care professionals and service users both accepting an active role, is essential to the success, or otherwise of SDM [47]. Yet service users often describe mixed feelings, that they are both helped and misunderstood by healthcare professionals, and commonly report experiencing discrimination [56, 57]. SDM involves the clinician respecting the right of service users to make treatment decisions, even if they disagree with this decision [58]. However, like other research, we found a mixed picture; the pharmacists perceived that some prescribers adopted an authoritative approach, dominating consultations and failing to take into account the views of service users [26, 59–62].
The participants perceived a lack of service user insight as the main barrier to SDM. Service users suffering from acute illness were said to lack capacity precisely when medication was most likely to be initiated or changed and, therefore, when SDM was important. However, when the illness being treated was well controlled, and the service user may be more likely to be able to be engaged in SDM, the pharmacists perceived that clinicians would be reluctant to change medication due to concerns about the illness becoming less well-controlled.
Generally the pharmacists reported that SDM was not possible with service users treated under the mental health act without their consent [63]. This act is designed to protect the rights, health and safety of people with a mental health disorder and the safety of others; it covers the circumstances in which someone can be detained for treatment [63]. Unlike some other studies, some pharmacists in this study did not view capacity in absolute terms [21]. They felt more should be done to engage service users and that SDM should be attempted with all service users to varying degrees depending on the level of insight and capacity. This echoes other research, which has found that service users with SMI value the opportunity to collaborate with those providing their care and are prepared to engage with SDM within the current patient-professional relationship [47]. SDM can also improve treatment knowledge amongst service users with schizophrenia potentially reducing the risk of medication errors [18, 64–66].
However, rather than focus on individual barriers, it may be more relevant to consider structural barriers to SDM in mental health practice such as a lack of time, poor communication between clinicians and service users, and limited access to evidence-based information [28, 58]. SDM can be seen to be a time consuming activity to undertake [22, 27]. In this research pharmacists reported the lack of time of both pharmacists and prescribers to be a barrier, with pharmacists identifying that other duties were seen to override SDM; other research has found that lack of time is a commonly reported barrier by both health professionals and service users [27, 51, 59, 60].
The pharmacists felt they were able to play a vital role in SDM partly because their independence from the prescribing process enabled them to engage in SDM. Previous research has identified the need for an inter-disciplinary approach involving autonomous clinicians to engage service users in SDM [67–70]. However, many of the pharmacists felt that they did not always get the opportunity to be involved in the SDM process due to the lack of a structured referral system and multi-disciplinary approach or resources issues within pharmacy departments.
Implications of study
Services should be structured to support SDM with a more inter-disciplinary approach. This could include a formal referral system to pharmacists or implementation of pharmacist clinics. Training for pharmacists (and potentially other clinicians) should highlight that SDM should be adapted depending on the state of illness at the time, but not abandoned.
Further study
Further qualitative research on SDM, and more specifically the potential role of pharmacy, involving pharmacists, other clinicians and service users is required. Research is also required on the impact of SDM on outcomes including adherence to medication [19, 48–50, 71]. Future research should investigate whether clinicians use SDM differentially depending on various characteristics including how long they have known the service user for and what the medication is being utilized for. It could also cover service users’ views on the role of family members as advocates. Previous research has identified a role for healthcare professional ‘coaches’ not involved in treatment to actively support service users in engaging in SDM [58]. Therefore, future research could investigate the impact of ‘pharmacy medication management coaches’ on key outcomes.
Limitations
All the participants recruited for the study came from the Midlands region and may not be broadly representative of attitudes and experiences of mental health pharmacists nationally and internationally. Moreover, we cannot be sure how long the participants had worked in mental health for (other than more than 1 year), whether they have a formal mental health qualification or their area of practice. We relied on convenience and snowballing sampling and relatively small sample sizes; however we found data saturation with consistent themes identified and no new themes identified in the last set of interviews. Additionally, identifying participants via known contacts may have influenced the interview responses in relation to socially desirable responses.
This research project only sought the views of mental health pharmacists; a future project should triangulate the data collection methods and also interview other clinicians and more importantly service users. Pharmacists are increasingly becoming prescribers and therefore future research should also compare and contrast the views and experiences of prescribing and non-prescribing (who are independent from the prescribing process) pharmacists.
Conclusion
In keeping with previous research in this area, SDM was seen as a positive concept by the mental health pharmacists interviewed. SDM should take into consideration the service user’s ability to tolerate adverse effects and their preferences regarding medication. The pharmacists believed that such an approach could improve service users’ satisfaction with medication management services and ultimately adherence to medication. The pharmacists perceived that the attitudes of prescribers and service users, although noted as variable, to be increasingly in favour of SDM.
The pharmacists identified that the use of SDM was limited by barriers, particularly the difficulties perceived by clinicians of engaging people with SMI who lack insight and mental capacity in the process. Greater effort is seen to be needed to work around these issues and try to engage service users as much as possible. Structural issues, such as time pressures may also limit the use of SDM.
Pharmacists clearly feel they can play a vital role in SDM but their skills and knowledge in this area are being underutilised, limiting their opportunity to contribute. SDM is clearly seen as one way to improve outcomes, and more research on how it can be effectively implemented in mental health is required.
References
Mental Health Foundation. What are mental health problems? n.d. http://www.mentalhealth.org.uk/help-information/an-introduction-to-mental-health/what-are-mental-health-problems/. Accessed 24 Nov 2015.
Hafal. Mental Health in Wales. n.d. http://www.mentalhealthwales.net/mhw/whatis.php. Accessed 9 Oct 2015.
Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373:31–41.
NICE. Clinical guidelines 76: medicines adherence involving patients in decisions about prescribed medications and supporting adherence available. 2009. http://www.nice.org.uk/guidance/cg76/chapter/introduction Accessed 4 Feb 2016.
Nosé M, Barbui C, Gray R, Tansella M. Clinical interventions for treatment non-adherence in psychosis: meta analysis. Br J Psychiatry. 2003;183:197–206.
Moritz S, Hünsche A, Lincoln TM. Nonadherence to antipsychotics: the role of positive attitudes towards positive symptoms. Eur Neuropsychopharmacol. 2014;24:1745–52.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63:892–909.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Clinical antipsychotic trials of intervention effectiveness (CATIE) investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;22:1209–23.
Levin JB, Sams J, Tatsuoka C, Cassidy KA, Sajatovic M. Use of automated medication adherence monitoring in bipolar disorder research: pitfalls, pragmatics, and possibilities. Ther Adv Psychopharmacol. 2015;5:76–87.
Lingam R, Scott J. Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 2002;105:164–72.
NICE. Clinical guideline 178: psychosis and schizophrenia in adults: treatment and management. 2014. https://www.nice.org.uk/guidance/cg178. Accessed 4 Feb 2016.
NHS. Shared decision making. 2012. http://sdm.rightcare.nhs.uk/. Accessed 3 Feb 2016.
Duncan E, Best C, Hagen S. Shared decision making interventions for people with mental health conditions. Cochrane Database Syst Rev. 2010;. doi:10.1002/14651858.CD007297.pub2.
Légaré F, Stacey D, Turcotte S, Cossi MJ, Kryworuchko J, Graham ID, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2014;. doi:10.1002/14651858.CD006732.pub3.
Elwyn G, Edwards A. Shared decision-making in health care: achieving evidence-based patient choice. 2nd ed. Oxford: Oxford University Press; 2009.
Holmes-Rovner M, Llewellyn-Thomas H, Entwistle V, Coulter A, O’Connor A, Rovner DR. Patient choice modules for summaries of clinical effectiveness: a proposal. Br Med J. 2001;322:664–7.
Department of Health. No health without mental health. 2011. https://www.gov.uk/government/publications/the-mental-health-strategy-for-england. Accessed 24 Nov 2015.
Maidment ID, Brown P, Calnan M. An exploratory study of the role of trust in medication management within mental health services. Int J Clin Pharm. 2011;33:614–20.
Joosten EA, DeFuentes-Merillas L, De Weert GH, Sensky T, Van Der Staak CP, De Jong CA. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77:219–26.
Wilson SR, Strub P, Buist AS, Knowles SB, Lavori PW, Lapidus J. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181:566–77.
Shepherd A, Shorthouse O, Gask L. Consultant psychiatrists’ experiences of and attitudes towards shared decision making in antipsychotic prescribing, a qualitative study. BMC Psychiatry. 2014;14:127.
Hamann J, Langer B, Winkler V, Busch R, Cohen R, Leucht S, Kissling W. Shared decision making for in-patients with schizophrenia. Acta Psychiatr Scand. 2006;114:265–73.
Hamann J, Cohen R, Leucht S, Busch R, Kissling W. Shared decision making and long-term outcome in schizophrenia treatment. J Clin Psychiatry. 2007;68:992–7.
Aljumah K, Hassali MA. Impact of pharmacist intervention on adherence and measurable patient outcomes among depressed patients: a randomised controlled study. BMC Psychiatry. 2015;15:219.
Farrelly S, Lester H. Therapeutic relationships between mental health service users with psychotic disorders and their clinicians: a critical interpretive synthesis. Health Soc Care Community. 2014;22:449–60.
Care Quality Commision. National summary of the results for the 2013 community mental health survey. 2013. http://www.cqc.org.uk/sites/default/files/MH14%20national%20summary%20v9%20with%20trust%20section%20FINAL.pdf. Accessed 20 Jan 2016.
Légaré F, Thompson-Leduc P. Advancing theories, models and measurement for an interprofessional approach to shared decision making in primary care: a study protocol. BMC Health Serv Res. 2008;8:2.
Torrey W, Drake R. Practising SDM in the outpatient psychiatric care of adults with SMI. Community Ment Health J. 2010;46:433–40.
Cribb A. Involvement shared decision-making and medicine. London: Royal Pharmaceutical Society, Center for Public Policy Research, Kings College; 2011. www.rpharms.com/news-story-downloads/rpsresearchreport.pdf. Accessed 24 Jan 2016.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57.
Cohen D, Crabtree B. Convenience sampling. Qualitative research guidelines project. 2006a. http://www.qualres.org/HomeRand-3812.htm. Accessed 21 Jan 2016.
Cohen D, Crabtree B. Purposeful sampling. Qualitative research guidelines project. 2006b. http://www.qualres.org/HomeConv-3802.html. Accessed 21 Jan 2016.
Crabtree BF, DiCicco-Bloom B. The qualitative research interview. Med Educ. 2006;40:314–21.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Charmaz K. Constructing grounded theory—a practical guide through qualitative analysis. London: Sage; 2006.
Atkinson P, Bauer MW, Gaskell G. Qualitative researching with text, image and sound: a practical handbook. London: Sage; 2000.
Mason JS, Lewis-Beck M, Bryman A, Liao TF. Semi-structured interview. The SAGE encyclopedia of social science research methods. 2004. http://srmo.sagepub.com/view/the-sage-encyclopedia-of-social-science-research-methods/n909.xml. Accessed 25 Jan 2016.
Srivastava P, Hopwood N. A practical iterative framework for qualitative data analysis. Int J Qual Methods. 2009;8:1.
Johnston M, Francis JJ, Robertson C, Glidewell L, Entwistle V, Eccles MP, Grimshaw JM. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25:1229–45.
Aronson J. A pragmatic view of thematic analysis. Qual Rep 1994;2:2. http://www.nova.edu/ssss/QR/BackIssues/QR2-1/aronson.html. Accessed 20 Mar 2015.
Bird C, How I. Stopped dreading and learned to love transcription. Qual Inq. 2005;11:2226–48.
Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ. 2010;74:8.
Corbin J, Strauss A. Ground theory research, procedures, canons and evaluative criteria. Z Soziol. 1990;6:418–27.
Cohen D, Crabtree B. Constant comparative method—grounded theory. 2006. http://www.qualres.org/HomeCons-3824.html. Accessed 4 Dec 2015.
Marshall SS, Haywood K, Fitzpatrick R. Group patient involvement and collaboration in shared decision-making: a review. Oxford: National Centre for Health Outcomes Development (Oxford Site); 2005.
Adams JR, Drake RE, Wolford GL. Shared decision making preferences of people with severe mental illness. Psychiatr Serv. 2007;58:9.
Eliacin J, Salyers M, Kukla M, Matthias M. Patients’ understanding of shared decision making in a mental health setting. Qual Health Res. 2015;25:668–78.
Malm U, Ivarsson B, Allebeck P, Falloon IR. Integrated care in schizophrenia: a 2-year randomized controlled study of two community-based treatment programs. Acta Psychiatr Scand. 2003;107:415–23.
Hamann J, Leucht S, Kissling W. Shared decision making in psychiatry. Acta Psychiatr Scand. 2003;107:403–9.
Thompson L, McCabe R. The effect of clinician-patient alliance and communication on treatment adherence in mental health care: a systematic review. BMC Psychiatry. 2012;12:87.
Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94:291–309.
Hamann AJ, Cohen R, Leucht S, Busch R, Werner KD. Do patients with schizophrenia wish to be involved in decisions about their medical treatment? Am J Psychiatry. 2005;162:2382–4.
Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1998;44:681–92.
Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. Br J Gen Pract. 1999;49:477–82.
Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behaviour: evidence, models and interventions. Patient Educ Couns. 2006;61:319–41.
Henderson C, Corker E, Lewis-Holmes E, Hamilton S, Flach C, Rose D, et al. England’s Time to Change Antistigma campaign: one-year outcomes of service-user rated experiences of discrimination. Psychiatr Serv. 2012;63:451–7.
Corker E, Hamilton S, Henderson C, Weeks C, Pinfold V, Rose D, et al. Experiences of discrimination among people using mental health services in England in 2008–2011. Br J Psychiatry. 2013;2013(202):s58–63.
Delman J, Clark JA, Eisen SV, Parker VA. Facilitators and barriers to the active participation of clients with serious mental illnesses in medication decision making: the perceptions of young adult clients. J Behav Health Serv Res. 2015;42:238–53.
Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor–patient communication about drugs: the evidence for shared decision making. Soc Sci Med. 2000;50:829–40.
Stevenson FA. General practitioners’ views on shared decision making: a qualitative analysis. Patient Educ Couns. 2003;50:291–3.
Elwyn G, Edwards A, Britten N. ‘Doing prescribing’: how doctors can be more effective. Qual Saf Health Care. 2003;327:864–7.
Towle A, Godolphin W, Grams G, Lamarre A. Putting informed and shared decision making into practice. Health Expect. 2006;9:321–32.
The National Archives. Mental Health Act. 2007. http://www.legislation.gov.uk/ukpga/2007/12/contents. Accessed 10 Nov 2015.
Maidment ID, Paton C, Lelliott P. A review of medication errors in mental health care. Qual Saf Health Care. 2006;15:409–13.
Hamann J, Mendel R, Meier A, Asani F, Pausch E, Leucht S, Kissling W. How to speak to your psychiatrist: shared decision making training for inpatient with schizophrenia. Psychiatr Serv. 2011;62:1218–21.
Ishii M, Okumara Y, Sugiyama N, Hasegaura H, Noda T, Hirayasu Y, Ito H. Efficacy of SDM on treatment satisfaction for patients with first admission schizophrenia: study protocol for a randomised controlled trial. BMC Psychiatry. 2014;14:111.
Légaré F, Stacey D, Pouliot S, Gauvin FP, Desroches S, Kryworuchko J, et al. Interprofessionalism and shared decision-making in primary care: a stepwise approach towards a new model. J Interprof Care. 2011;25:18–25.
Chong WW, Aslani P, Chen T. Understanding barriers and facilitators of decision-making and inter-professional collaboration in mental healthcare: a qualitative study. Res Social Adm Pharm. 2012;8:e36–7.
Kassam R, Volume-Smith C, Albon SP. Informed shared decision making: an exploratory study in pharmacy. Pharm Pract. 2008;6:57–67.
Jones SC. The risks and benefits of shared decision making about medicines in mental health care. University of Bath. Department of Pharmacy and Pharmacology. 2011.
Bunn HM, O’Connor AM, Tansy MS, Jones DBW, Stinson LE. Characteristics of clients with schizophrenia who express certainty or uncertainty about continuing treatment with depot neuroleptic medication. Arch Psychiatr Nurs. 1997;11:238–48.
Acknowledgments
We acknowledge the support and input from the pharmacists who agreed to be interviewed.
Funding
No specific funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest were identified.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Younas, M., Bradley, E., Holmes, N. et al. Mental health pharmacists views on shared decision-making for antipsychotics in serious mental illness. Int J Clin Pharm 38, 1191–1199 (2016). https://doi.org/10.1007/s11096-016-0352-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0352-z